Abstract
Background
Recreational nitrous oxide (N2O) use has become more widespread worldwide, leading to an increase in myelopathies and peripheral neuropathies. The aim of this study was to describe clinical and socioeconomical characteristics of severe N2O-induced (NI) neurological disorders (NI-NDs), to determine its incidence in the Greater Paris area and to compare it with that of similar inflammatory neurological disorders.
Methods
We performed a retrospective multicentric cohort study of all adult patients with severe NI-NDs in the neurology and general internal medicine departments of the Greater Paris area from 2018 to 2021. The incidence was compared with that of non-NI-myelitis and Guillain–Barré syndrome (GBS) using a sample of 91,000 hospitalized patients sourced from health insurance data.
Results
Among 181 patients, 25% had myelopathy, 37% had peripheral neuropathy and 38% had mixed disease. Most were aged between 20 and 25 years, lived in socially disadvantaged urban areas, and exhibited high rates of unemployment (37%). The incidence of NI-NDs increased during 2020 and reached a peak mid-2021. The 2021 incidence in 20–25-year-olds was 6.15 [4.72; 8.24] per 100,000 persons for NI-myelopathy and 7.48 [5.59; 9.37] for NI-peripheral neuropathy. This was significantly higher than for non-NI-myelitis (0.35 [0.02; 2.00]) and GBS (2.47 [0.64; 4.30]). The incidence of NI-NDs was two to three times higher in the most socially disadvantaged areas.
Conclusion
The recent increase in recreational N2O use has led to a rise in the incidence of severe NI-NDs, particularly in young adults with low socioeconomic status for whom NI-NDs strongly outweigh similar neurological disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, a sharp rise in nitrous oxide (N2O) use for recreational purposes has been observed worldwide [1,2,3]. Due to the inactivation of the cobalt ion responsible for the loss of vitamin B12 activity [4], N2O inhalation can lead to central and peripheral neurological disorders, i.e. myelopathy and peripheral neuropathy. Consequently, the incidence of these complications has increased dramatically to become a major public health concern [5,6,7].
The clinical presentation may mimic differential diagnoses which necessitate prompt and aggressive treatment approaches, such as the administration of intravenous immunoglobulins or corticosteroids. Furthermore, as the incidence of severe N2O-induced (NI) neurological disorders (NI-NDs) increases, so does the risk of confusing NI-NDs with its differential diagnoses, potentially leading to therapeutic errors. Although several small series are available, the incidence of NI-NDs has only been captured indirectly through spontaneous drug safety notifications [8]. We investigated the incidence and characteristics of severe NI-NDs among adults in the Greater Paris area. We assessed the incidence of central and peripheral NI-NDs and compared it to that of the main severe non-NI neurological disorder (non-NI-NDs) differential diagnoses: myelitis and Guillain–Barré syndrome (GBS).
Methods
To estimate the incidence of severe NI-NDs in the Greater Paris area, we established a retrospective multicentric cohort of adult patients with severe NI-NDs from January 1, 2018, to December 31, 2021. We contacted all neurology and general internal medicine departments in the region. The severe NI-NDs considered were hospital-attended N2O-induced myelopathy and peripheral neuropathy. Patients were included in the NI-NDs cohort if they were over 18 years old and presented neurological symptoms during the target period. Symptoms had to be related to N2O consumption with no alternative diagnosis and taken care of/sought hospital care in neurology or internal medicine. Exclusion criteria included being under legal protection (guardianship, curatorship) at the time of hospital consultation. Demographic and paraclinical data were collected by the referring physician using a standardized grid including demographic, clinical, biological and therapeutic data, as well as follow-up data when available (Supplementary Table S1: Survey Form). Demographic data for the Greater Paris area were extracted via government agencies (Details in Supplementary data: Research Protocol). The study received ethics committee approval from Hôpital Delafontaine, Saint-Denis. The incidence of NI-NDs was compared with similar differential diagnoses, which were hospital-attended non-N2O-induced myelitis and Guillain–Barré syndrome (GBS), which is the most common form of severe peripheral neuropathy. To estimate the incidence rate of severe non-NI-NDs, we used hospitalization data from the Échantillon Généraliste de Bénéficiaires (EGB), a 1/97th permanent and representative (in terms of age, sex, and medical expenses) sample of the French Health Insurance database [9] (consisting of 91,000 inpatients). We identified all adult patients hospitalized for myelitis or GBS from January 1, 2011, to December 31, 2019.
Disorders were ascertained based on disease-specific ICD-10 codes recorded as main or related diagnosis (G373 for acute transverse myelitis in demyelinating disease of central nervous system and G610 for GBS). Inclusion criteria for the EGB cohort were being aged 18 years or over on January 1 of each year and having at least 2 years of presence in the EGB database prior to January 1 of each year, with exclusion criteria including presenting any of the studied diseases in the 2 years preceding January 1 of each year.
Considering that severe NI-NDs were rare before 2019 [10] and assuming stable incidence of inflammatory neurological disorders over time, we deemed it appropriate to compare the overall and age-group pre-2019 incidence rates of GBS and myelitis with the 2018–2021 incidence rates of NI-neuropathy and NI-myelopathy, respectively.
We estimated 95% binomial proportion confidence intervals. Non-overlapping 95% CI indicate significant differences between the incidence rates. For the age analysis, age was split into 5-year categories. Detailed information on the research protocol is available in Supplementary data. We followed the recommendations of the RECORD declaration (REporting of Conducted Studies using Observational Routinely-collected health Data).
Results
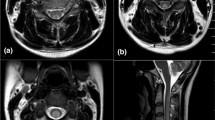
Out of the 81 units contacted, 78 (96%) participated in the retrospective study (Supplementary Fig. S1) and reported a total of 181 patients with NI-NDs. One hundred and sixty-nine patients (95%) came from a neurology department and 143/178 (80%) were hospitalized. Average daily consumption was 2 carboys (equivalent to 1200 g of N2O). Median duration between the beginning of N2O consumption and the onset of symptoms was 6 (IQR 2–12) months. No cases were detected before the end of 2019. The incidence then increased sharply in 2020, with a maximum of 143/178 (80%) cases in 2021 (Fig. 1).
One hundred and seven patients (60%) were aged between 20 and 25 years, with no previous medical history in 169/178 (95%) of cases, 44/181 (25%) had myelopathy, 66/181 (37%) had peripheral neuropathy and 68/181 (38%) had mixed disease. Sensorimotor disorders were the main cause of disability, with an acute Rankin score ≥ 4 in 42/128 (33%) cases with available data. Data on clinical evolution after 1 month were available for 64 patients, with full recovery reported only in 5/64 (8%). One hundred sixty-eight patients (96%) were treated with Vitamin B12. Additionally, 11% (18/161) self-medicated with Vitamin B12 before hospitalization without altering their consumption habits.
The main demographic, clinical and biological data are shown in Table 1, with additional information in Supplementary Table S2.
In the Greater Paris area, there were 60/181 (33%) cases in Paris, 109/181 (61%) in the inner suburbs, and only 29/181 (6%) in the outer ones (Supplementary Fig. S2). Outside Paris, 62/109 (57%) cases were reported in Seine-Saint-Denis, while some more privileged administrative counties reported none.
The unemployment rate was higher in cohort patients (61/167; 37%) than in the Greater Paris area population (8%; p < 0.001), and workers often had low-income jobs. The most affected administrative counties were also the most socially disadvantaged ones. Seine-Saint-Denis, the administrative county with the highest incidence of NI-NDs, has the lowest average incomes (Fig. 2) and 19% of its inhabitants received welfare for the unemployed versus 10% in the whole Greater Paris area [11,12].
In the Greater Paris area, the incidence of NI-myelopathy and non-NI myelitis was 0.75 [95% CI 0.6; 0.91] and 0.66 [95% CI 0.41; 0.92] cases per 100,000 person-years, respectively. The incidence of NI-neuropathy and GBS was 0.84 [95% CI 0.67; 1.00] and 3.77 [95% CI 3.17; 4.38] cases per 100,000 person-years, respectively. Among the 20–25 years old individuals, the incidence of NI-myelopathy was 6.15 [95% CI 4.72; 8.24] cases per 100,000 person-years, which is significantly higher than that of non-NI myelitis estimated at 0.35 [95% CI 0.02; 2.00] cases per 100,000 person-years (Fig. 3). In this same age group, the incidence of NI-neuropathy was 7.48 [95% CI 5.59; 9.37] cases per 100,000 person-years, which was significantly higher than that of GBS with 2.47 [95% CI 0.64; 4.30] cases per 100,000 person-years. In Seine-Saint-Denis, the rate of NI-myelopathy and neuropathy in individuals 20–25 years old individuals was 16.64 [8.96; 24.33] and 20.34 [11.84; 28.84], respectively, which was significantly higher than in the whole Greater Paris area.
Age-specific incidence of NI and non-NI neurological disorders. There is a significantly higher incidence of neurological complications in individuals under the age of 25 following N2O intoxication compared with similar disorders: NI peripheral neuropathy and GBS (left panel), and NI/non-NI myelopathy (right panel). Abbreviation: GBS Guillain–Barré syndrome, NI N2O-induced
Discussion
This multicenter study investigated a large cohort of severe NI-NDs to estimate its incidence, and compared it with similar neurological disorders in the same population. The estimated incidence of NI-NDs was significantly higher than the overall incidence of similar neurological diseases in young people, due to a sharp increase in incidence after 2020 that peaked in 2021. Most patients were young people from socially disadvantaged areas. Complications are severe with motor deficits and significant disability, and complete early recovery was rare.
Since no specific diagnosis code was available to compute the incidence of NI-NDs, our method of collecting individual cases was the only possible method to estimate the incidence of these complications.
The main limitation of our study is that we compared incidence obtained from cases collection to incidence obtained from administrative health database. However, we consider this approach acceptable as selecting only severe NI-NDs could only lower the estimated incidence and the true gap with the incidence of non-NI-NDs could be even greater. The likelihood of having missed any hospitalized cases seems low due by two factors: the almost complete participation of all centers in Greater Paris and a recall bias considered limited.
The latter is attributed to a relatively short study period (4 years) and particularly striking cases due to the novelty of the disease, the severity of the conditions in young patients without medical history and their extraordinarily high consumption of N2O.
The low probability of having missed hospitalized cases is primarily supported by two factors: the near-complete participation of hospital centers in the Paris area and a low memory bias. The latter is attributed to the limited duration of the study, which spans four years, thereby facilitating the recall of information. Moreover, memory retention is enhanced by the unusual nature of the cases observed, characterized by the novelty of the disease, the severity of symptoms in young patients without medical history, and their exceptionally high level of consumption.
A further limitation is a possible border effect as geographical localisation of cases is based on hospitalisations and patients might seek hospital care beyond their nearest facility. However, as individual case data were compared with ecological data on the income levels of the areas, conclusions are inherently broad. Precise individual level conclusions are not possible, we can generally infer that lower-income areas have a higher incidence of cases. Furthermore, the observed higher case numbers in Paris, despite its higher income levels, may be attributed to its greater hospital density. It is interesting to note that a stronger concentration of cases is observed in areas of Paris adjacent to the Parisian suburbs where income is lowest, which could be explained by this border effect.
N2O was the 8th most consumed drug globally in 2017, particularly popular among medical students and the nightclub scene [13,14,15]. During the same period and in the same area, medical students reported an average consumption of 2 cartridges per year, which is equivalent to 16 g of N2O annually, representing a quantity 27,000 times lower than that the mean consumption observed in our study [16]. Moreover, medical students did not manifest any severe neurological complications. This points to a dose-dependent effect of N2O consumption on the onset of neurological disorders as suggested in other studies [17].
In line with DSM-V criteria [18], N2O consumption in our cohort was characteristic of an addictive disorder, in contrast to previous debates on the addictive potential of N2O [15]. Moreover, the psychological profile of these users indicates a marked psychiatric vulnerability [19]. Despite consumption dating back to the eighteenth century, reported cases of NI-NDs were exceptional until recently [10]. A systematic review of literature up to 2018 only found a hundred of patients, published solely in case reports [10]. The recent increase could be attributed to both more frequent consumption and higher intake, a trend that, despite methodological differences in studies, indicates a substantial rise in reported cases that likely surpasses the impact of potential biases. The incidence rates reported here relate only to severe NI-NDs, as we focused on patients suffering from signs severe enough to initiate a hospital diagnosis and care. However, as 2–8% of N2O users may experience minor sensory symptoms [17], therefore the overall rate of NI-NDs is probably far higher.
While this study was restricted to the Greater Paris area, which comprises 20% of the French population (12.4 million inhabitants), N2O consumption has become a worldwide practice [6,7,8,20]. In France, both COVID-19 and lockdown may have contributed to the increased consumption [8,21], but there was already a global trend of increased use before the pandemic in other countries [22,23]. Globally, the escalation in N2O consumption, as well as the reported increase in complications, dates back to around 2018, coinciding with the introduction of N2O carboys on the market23,24. These carboys contain on average 100 times the dose contained in a standard cartridge and their ease of use may have facilitated higher consumption, which could be another factor contributing to the increase in N2O complications.
Conclusion and relevance
High levels of N2O intake may cause severe NI-NDs with disability and uncertain recovery. In 2021, incidence of NI-NDs was significantly higher than those of myelitis and GB. Most affected patients were young people from socially disadvantaged areas. Our findings not only point to a medical concern but also shed light on underlying socioeconomic factors and potential addictive behaviors associated with N2O use. These results indicate a marked shift in consumption patterns towards larger and harmful doses. Given the global prevalence of N2O use, this might signal a growing public health issue extending beyond France’s borders. Education campaigns and comprehensive prevention strategies would be crucial to address this concerning trend.
Data availability
Data not presented in the article are available in the supplements. If more data are necessary, please contact us by mail.
References
Sumnall H (2022) Recreational use of nitrous oxide. BMJ 378:o2297. https://doi.org/10.1136/bmj.o2297
Randhawa G, Bodenham A (2016) The increasing recreational use of nitrous oxide: history revisited. Br J Anaesth 116(3):321–324. https://doi.org/10.1093/bja/aev297
Xiang Y, Li L, Ma X et al (2021) Recreational nitrous oxide abuse: prevalence, neurotoxicity, and treatment. Neurotox Res 39(3):975–985. https://doi.org/10.1007/s12640-021-00352-y
Sanders RD, Weimann J, Maze M, Warner DS, Warner MA (2008) Biologic effects of nitrous oxide: a mechanistic and toxicologic review. Anesthesiology 109(4):707–722. https://doi.org/10.1097/ALN.0b013e3181870a17
Layzer RB, Fishman RA, Schafer JA (1978) Neuropathy following abuse of nitrous oxide. Neurology 28(5):504–504. https://doi.org/10.1212/WNL.28.5.504
Zheng D, Ba F, Bi G, Guo Y, Gao Y, Li W (2020) The sharp rise of neurological disorders associated with recreational nitrous oxide use in China: a single-center experience and a brief review of Chinese literature. J Neurol 267(2):422–429. https://doi.org/10.1007/s00415-019-09600-w
Mair D, Paris A, Zaloum SA et al (2023) Nitrous oxide-induced myeloneuropathy: a case series. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2023-331131. (Published online May 30, 2023)
Guerlais M, Aquizerate A, Lionnet A et al (2023) Nitrous oxide: a unique official French addictovigilance national survey. Front Public Health 11:1167746. https://doi.org/10.3389/fpubh.2023.1167746
Scailteux LM, Droitcourt C, Balusson F et al (2019) French administrative health care database (SNDS): the value of its enrichment. Therapies 74(2):215–223. https://doi.org/10.1016/j.therap.2018.09.072
Oussalah A, Julien M, Levy J et al (2019) Global burden related to nitrous oxide exposure in medical and recreational settings: a systematic review and individual patient data meta-analysis. J Clin Med 8(4):551. https://doi.org/10.3390/jcm8040551
Accueil | Direction de la recherche, des études, de l’évaluation et des statistiques. Accessed Nov 1, 2023. https://drees.solidarites-sante.gouv.fr/
Accueil - Insee - Institut national de la statistique et des études économiques. Accessed Nov 1, 2023. https://www.insee.fr/fr/accueil
Rosenberg H, Orkin FK, Springstead J (1979) Abuse of nitrous oxide. Anesth Analg 58(2):104–106
Kaar SJ, Ferris J, Waldron J, Devaney M, Ramsey J, Winstock AR (2016) Up: the rise of nitrous oxide abuse. An international survey of contemporary nitrous oxide use. J Psychopharmacol 30(4):395–401. https://doi.org/10.1177/0269881116632375
van Amsterdam J, Nabben T, van den Brink W (2015) Recreational nitrous oxide use: prevalence and risks. Regul Toxicol Pharmacol 73(3):790–796. https://doi.org/10.1016/j.yrtph.2015.10.017
Thevenin M (2023) Épidémiologie de la consommation récréative de protoxyde d’azote chez les étudiants en médecine d’Ile-de-France. Doctoral thesis. Université Paris Cité
Winstock AR, Ferris JA (2020) Nitrous oxide causes peripheral neuropathy in a dose dependent manner among recreational users. J Psychopharmacol 34(2):229–236. https://doi.org/10.1177/0269881119882532
Barnhill JW (2013) DSM-5® clinical cases. American Psychiatric Pub
Wu G, Wang S, Wang T et al (2022) Neurological and psychological characteristics of young nitrous oxide abusers and its underlying causes during the COVID-19 lockdown. Front Public Health 10:854977. https://doi.org/10.3389/fpubh.2022.854977
Nabben T, Weijs J, van Amsterdam J (2021) Problematic use of nitrous oxide by young moroccan-dutch adults. Int J Environ Res Public Health 18(11):5574. https://doi.org/10.3390/ijerph18115574
Lapeyre-Mestre M, Boucher A, Daveluy A et al (2020) Addictovigilance contribution during COVID-19 epidemic and lockdown in France. Therapie 75(4):343–354. https://doi.org/10.1016/j.therap.2020.06.006
Bethmont A, Harper CE, Chan BS, Dawson AH, McAnulty J (2019) Increasing illicit use of nitrous oxide in presentations to NSW emergency departments. Med J Aust 211(9):429–429. https://doi.org/10.5694/mja2.50377. (e1)
European Monitoring Centre for Drugs and Drug Addiction. Recreational nitrous oxide use in Europe: situation, risks, responses. Accessed Nov 4, 2023. https://www.emcdda.europa.eu/publications/topic-overviews/recreational-nitrous-oxide-use-europe-situation-risks-responses_en
Winstock A, Munksgaard R, Davies E, Ferris J, ZhuParris A, Barratt M (2022) Drug trend report: time, music, clubbing, age, and diet. Global Drug Survey
Acknowledgements
Acknowledgements for participation and contribution to data collection: Anne Catherine BACHOUD LEVI (MD, Ph.D.) from Henri-Mondor Hospital, Carole HENRY and Karolina HANKIEWICZ (MD) from Saint-Denis Hospital, Ovidiu CORABIANU (MD) from Aulnay Hospital, Laura Venditti (MD) from Kremlin-Bicêtre Hospital, Bertrand DEGOS (MD, Ph.D.) Avicenne Hospital, Pierre LOZERON (MD, Ph.D.) from Lariboisière Hospital, Jean-Christophe CORVOL (MD Ph.D.) and Vincent DAVY (MD) from Pitié Salpêtrière Hospital, Bertrand LAPERGUE (MD, Ph.D.) from Foch Hospital, Bruno STANKOFF (MD, Ph.D.) from Saint-Antoine Hospital, Didier SMADJA (MD) from Sud Francilien Hospital, VANQUAETHEM Helene (MD) from Bégin Hospital, Gayane MELIKSETYAN (MD) and Loubna MAJHADI (MD) from Argenteuil Hospital, Fernando PICO (MD) and Jérôme SERVAN (MD) from Versailles Hospital, Thomas PAPO (MD) and Laure DELAVAL (MD) from Bichat Hospital, Guillaume NICOLAS (MD, Ph.D.) and Edouard BERLING (MD) from Raymond Poincaré Hospital, Mathieu ZUBER (MD, Ph.D.) and Veronique MARCAUD (MD) from Saint-Joseph Hospital, Romain DESCAHMPS (MD) and Olivier GOUT (MD) from Fondation Rothschild Hospital, Damien RICARD (MD, Ph.D.) Percy hospital and Jean-Vincent MARCADIER (MD) from Rambouillet Hospital.
Author information
Authors and Affiliations
Contributions
YD, LA, MB and TDB contributed to conception and design of the study; YD, LA, MB, TG, AM, AEL, JM, AZ, NK, ALD, LG, HBN, WC, AF, and AV contributed to the acquisition and analysis of data; YD, LA, MB, TDB, and TIG contributed to drafting the text or preparing the figures.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standard
The study received ethics committee approval from Hôpital Delafontaine, Saint-Denis.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dawudi, Y., Azoyan, L., Broucker, T.D.E. et al. Marked increase in severe neurological disorders after nitrous oxide abuse: a retrospective study in the Greater Paris area. J Neurol 271, 3340–3346 (2024). https://doi.org/10.1007/s00415-024-12264-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-024-12264-w