Abstract
Increasing evidence suggests that brain edema might play an important role in the pathogenesis of sudden infant death syndrome (SIDS) and that variants of genes for cerebral water channels might be associated with SIDS. The role of the sulfonylurea receptor 1 (SUR1)–transient receptor potential melastatin 4 (TRPM4) non-selective cation channel in cerebral edema was demonstrated by extensive studies. Therefore, we hypothesized that variants at genes of the SUR1-TRPM4 channel complex might be linked to SIDS. Twenty-four polymorphisms in candidate genes involved in the SUR1-TRPM4 non-selective cation channel were investigated in 185 SIDS cases and 339 controls. One (rs11667393 in TRPM4) of these analyzed SNPs reached nominal significance regarding an association with SIDS in the overall analysis (additive model: p = 0.015, OR = 1.438, 95% CI = 1.074–1.925; dominant model: p = 0.036; OR = 1.468, 95% CI = 1.024–2.106). In the stratified analysis, further 8 variants in ABCC8 (encoding SUR1) or TRPM4 showed pronounced associations. However, none of the results remained significant after correction for multiple testing. This preliminary study has provided the first evidence for a genetic role of the SUR1-TRPM4 complex in the etiology of SIDS, and we suggest that our initial results should be evaluated by further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden infant death syndrome (SIDS), the leading cause of death in infants aged 1 month to 1 year in developed countries, is the sudden death of an infant under 1 year of age that remains unexplained after a thorough case investigation, including performing a complete autopsy, examining the death scene, and reviewing the clinical history [1, 2]. However, the specific etiologic mechanisms of SIDS are poorly understood. The triple risk model suggests that a combination of a critical developmental stage, a vulnerable infant, and extrinsic factors is associated with SIDS [3].
Previous relevant studies have shown increased brain weight and/or cerebral edema in some cases of SIDS [4,5,6,7,8], although the results of some studies are inconsistent with this [9,10,11]. For instance, the study conducted by Aranda et al. demonstrated that the cases diagnosed as SIDS had heavier brain weights compared to age-matched controls [4], and the findings were in line with other related studies [6,7,8]. The elevated brain weight in SIDS is thought to be possibly due to abnormal brain development or cerebral edema [4, 6], whereas the exact pathogenic mechanism is still uncertain. In contrary, Studer et al. reported that they did not find an elevated brain-to-body weight ratio in SIDS cases; however, they also mentioned that cytotoxic edema in the central nervous system (CNS) does not always lead to brain swelling [9]. In several Norwegian studies, genetic variants of aquaporin genes (AQP) like AQP1, 4, and 9, as critical rapid water transport channels on the plasma membrane, were associated with SIDS [12,13,14]. Especially, aquaporin-4 (AQP4), a main water channel in the central nervous system, is known to have a key role in the formation of cerebral edema [15,16,17]. For SIDS cases that are carriers of several specific AQP4 variant genotypes (CT/TT, rs2075575), an increased brain-to-body weight ratio was found, and thus a putative association of AQP4 variants and cerebral edema in SIDS [12]. In a recent study, the lower expression of AQP4 in the brain tissue was observed in the carriers with the CT/TT genotype of rs2075575 [18].
In addition to constitutively expressed transporters like AQP4, Kir4.1 as an ATP-sensitive K+ channel could assemble with AQP4 to form a complex (water-ion transport coupling) that plays an important role in cerebral edema [19]. Opdal et al. demonstrated the potential link between the SNP locus of the gene encoding Kir4.1 and SIDS [14]. Like Kir4.1, the inducible SUR1-TRPM4 non-selective cation channel plays a similar role in the mechanism of brain edema formation when ATP is depleted and Ca2+ concentration increases [20,21,22]. It has been previously observed that AQP4 also could co-associate physically with SUR1-TRPM4 to form a heteromultimeric complex, as ion/water osmotic coupling, which exerts an important role in astrocyte swelling and cerebral edema caused after injury [23]. The SUR1-TRPM4 non-selective cation channel includes two subunits: sulfonylurea receptor 1 (SUR1, encoded by the ABCC8 gene) is a member of the ATP-binding cassette transporter family, with its activity modulated by the intracellular ATP/ADP ratio [24]; transient receptor potential melastatin 4 (TRPM4) is a Ca2+-regulated non-selective ion channel [25]. Preclinical and clinical trials indicate that pharmacological blockade of SUR1-TRPM4 could be used to reduce secondary brain swelling after injury [24, 26]. Additionally, studies have shown an association between intracranial pressure or cerebral edema after brain injury and several genetic SNP loci in these genes (ABCC8 and TRPM4) [27,28,29].
Therefore, we hypothesized that variants located in the ABCC8 and TRPM4 genes may lead to an increased risk to develop cerebral edema and thus infants susceptible to SIDS and investigated 185 SIDS cases and 339 controls for 24 polymorphisms in candidate genes involved in the SUR1-TRPM4 non-selective cation channel relevant to the development of cerebral edema.
Materials and methods
Study subjects
The SIDS cohort (n = 185) was enrolled from the Institute of Legal Medicine, Hannover Medical School, and its branch (Oldenburg). The enrollment standards based on the San Diego definition of SIDS [1] were briefly as below: (1) unexpected death during the sleep occurring in their first year of life; (2) no specific cause of death diagnosed after thorough postmortem examination, review of the case history, and death scene investigation. In approximately 50% of the cases, toxicological and/or histological examinations were performed, as commissioned by the respective prosecutor’s office. Radiological or specialized neuropathological investigations as well as genetic screening were performed only for very few cases. 62.6% of the SIDS cases were boys. The average age was 130 days. Among the SIDS cases documented with sleeping positions (n = 46), 73.9% of cases were prone positions. The control cohort (n = 339) comprised 164 males, 146 females, and 29 gender-unrecorded individuals. It comprised 33 children and 306 healthy adults. The 33 included children in controls were in the first year of life but died due to an explicit cause of death but not SIDS (mostly trauma, infections, and congenital heart defects). Owing to anonymization exact age information was not available in controls. The local ethics committee of Hannover Medical School approved this study.
Selection of SNPs and genotyping assays
The selection of candidate SNPs of ABCC8 and TRPM4 was on account of previously published studies in which a potential association with a specific disease or a possible influence on gene expression was reported. In brief, the selection criteria were as follows: (1) the minor allele frequency (MAF) ≥ 0.05 in Caucasians; (2) SNPs were not in high linkage disequilibrium (LD) (R2 < 0.8); (3) SNPs were reported in published studies or in the GTEx portal (https://www.gtexportal.org/home/) to influence related gene expressions.
A total of 24 candidate SNP loci (14 in the ABCC8 gene, 10 in the TRPM4 gene) were included in the analysis. The detailed information of these 24 SNPs is given in Table 1 and Supplementary material 1.
DNA extraction was performed from blood, saliva, or thymus samples using the QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) following the manufacturer’s instructions. All DNA samples were kept at − 20 °C for long-period storage. As described in our previous studies [30], genotyping was performed using 192.24 dynamic arrays in the Biomark EP1 platform (Fluidigm, South San Francisco, CA, USA), and the original data was analyzed using the Fluidigm SNP Genotyping Analysis Software Version 4. Probes and related primers were listed in Supplementary material 2. Total, three genotyping arrays were run. For quality control, 46 duplicates (8.7% samples from both cases and controls) were included in the genotyping, and two negative controls (no DNA) were assigned in each array.
Data analyses
Two SNPs (rs10766397 and rs8104571) had low call rates (< 95%) and were excluded for further analyses. Among the remaining 22 SNPs, one SNP (rs34271662) was excluded owing to the failure of clustering. Chi-square (χ2) tests were applied to check the Hardy–Weinberg equilibrium (HWE) in controls using an online HWE calculator (https://wpcalc.com/en/equilibrium-hardy-weinberg/). Two SNPs (rs4802581 and rs60105962) deviating from HWE were eliminated for the subsequent analysis. For the 19 remaining variants, a 2 × 2 chi-square (χ2) test or a Fisher exact test was utilized to test the association of SNPs and SIDS using dominant, and recessive models and a linear-by-linear model of the χ2 test (same to the Cochrane-Armitage trend test) was used under the additive model. Odds ratios (ORs), 95% confidence intervals (CIs), and corresponding p values were calculated.
For the stratified analysis, study subjects were categorized into 4 different groups according to the risk factors for SIDS. These were (1) gender (males (n = 99), females (n = 59)), age group (0–4 months (n = 104), 2–4 months (n = 75), 4–8 months (n = 51), 8–12 months (n = 9)), time of death season (spring (n = 40), summer (n = 30), spring + summer (n = 70), autumn (n = 35), winter (n = 40), autumn + winter (n = 75)), and sleeping positions (prone position (n = 34), other positions (n = 12)) as shown previously [31].
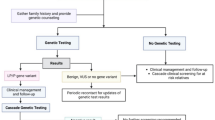
SNPs in linkage with each other (R2 < 0.8 and D′ > 0.75) among the European population were included for the haplotype analysis. Haplotype analysis was performed by Haploview 4.2 (Broad Institute, Cambridge, MA, USA) in the study subjects and by LDlink (https://ldlink.nci.nih.gov/) in the European population (Fig. 1). A two-sided p value < 0.05 was considered indicating statistical significance in all statistical analyses. Bonferroni correction was used for multiple comparisons, and p < 0.0001 was considered statistical significance after multiple testing. All statistical analyses were performed using SPSS 24.0 software (SPSS Inc. Chicago, IL, USA).
Results
We successfully genotyped 19 variants at TRPM4 and ABCC8 in up to 185 SIDS cases and 339 controls. All nominally significant results (p < 0.05) of the chi-square analysis are listed in Table 2. In the overall analysis, one SNP (rs11667393 in the TRPM4 gene) was below the significance threshold of α = 0.05 (additive model: p = 0.015, OR = 1.438, 95% CI = 1.074–1.925; dominant model: p = 0.036; OR = 1.468, 95% CI = 1.024–2.106).
The stratified analysis was performed to evaluate the effects of the variants located in ABCC8 and TRPM4 on the hazards of SIDS by age, gender, time of death season, and sleep positions. In the stratified results, 14 nominally significant results (p < 0.05) were obtained. The only one associated locus in the main analysis, rs11667393, showed no specific associations in any one subcategory. However, rs4148622 in ABCC8 indicated significant differences between cases and controls in four subgroups (“age 0–4 months,” “age 2–4 months,” “Spring,” and “Spring + Summer”), and rs7950189 in ABCC8 in two subgroups (“age 8–12 months” and “other sleep positions”). Both rs3760662 and rs11083962 in the TRPM4 gene were associated with SIDS in two subgroups (“Summer” and “Spring + Summer”). Variants rs7105832 and rs3819521 located in ABCC8 showed associations with SIDS in one subgroup (“age 4–8 months”). In the “Winter” subcategory, rs7112138 from ABCC8 was indicated to be related to SIDS. SNP rs3758953 at the ABCC8 gene had a single association in the category “Prone sleep position.” None of the above-mentioned findings in the stratified analysis remained statistically significant after Bonferroni correction at α = 0.0001, but these results may still suggest a biological relevance for the etiology of SIDS.
In a haplotype analysis, the extent of LD among the identified SNPs in ABCC8 and TRPM4 was estimated using Haploview 4.2 and LDlink. The related haplotype blocks were respectively screened in ABCC8 and TRPM4 (Fig. 1). The haplotype block in ABCC8 was comprised of 4 SNPs (rs7950189, rs3819521, rs1048099, and rs985136). The haplotype-based association analysis provided evidence that the haplotype TCAG in ABCC8 may be relevant for SIDS (p = 0.040) (Table 3). As for TRPM4, three SNPs (rs11083963, rs12980226, and rs7251160) were included in the block. TRPM4 haplotype AAT was significantly associated with SIDS (p = 0.031) (Table 4). Nevertheless, both potentially associated risk haplotypes were rare in both SIDS and controls.
To assess a potential functional relevance for the gene expression, cis-eQTL target gene expression was employed using the online data from Genotype-Tissue Expression (GTEx) project. Eight of the nine SNPs with nominally statistical significance (except rs3758953 from ABCC8) were reported to influence the gene expression in tissue from the CNS.
Discussion
It has been postulated that disturbances in the brain water balance may be involved in the pathogenesis of at least some SIDS cases. Previous studies have uncovered that SNP loci for genes involved in ion channels and water channels (like AQP1, 4, 9, and Kir4.1) might be associated with SIDS [12,13,14], although one study did not confirm this finding [9]. The opening of SUR1-TRPM4 channels is associated with an undifferentiated influx of monovalent cations and cell depolarization, followed by cytotoxic edema, cell death, blood–brain barrier (BBB) breakdown, and formation of vasogenic edema in the CNS, suggesting an important role of the SUR1-TRPM4 non-selective cation channel in brain edema [27,28,29]. Accordingly, it is reasonable to speculate that this SUR1-TRPM4 complex might play a potential role at least in some subgroups of SIDS, although up to now this has never been studied. In the present study, we thus investigated the genotypes and haplotypes of 24 SNP loci located in the corresponding genes (ABCC8 and TRPM4).
Overall, there was evidence that 9 of the 24 candidate SNP loci could be associated with SIDS, though 8 of them only in subgroups. Three putative risk SNPs were located within TRPM4 and the other six in ABCC8. The only nominally significant SNP in the main analysis was located in TRPM4, and the other 8 genetic variants were identified in the stratified analysis (ABCC8 (6 variants) and TRPM4 (2 variants)).
The G allele or GG/AG genotypes of polymorphism rs11667393 located in TRPM4 were associated with SIDS (allele G in SIDS: 32.9%, vs. 26.1% in controls), suggesting that this SNP locus could be an influential predisposing factor. However, in a study on cerebral edema secondary to traumatic brain injury (TBI), no association for this locus was shown [27]. According to the GETx database (although being an intronic variant), carriers of the rs11667393 G allele typically have alerted mRNA levels of TRPM4 in several human tissues, suggesting that this variant may affect the TRPM4 gene expression. The increased expression of TRMP4 could aggravate the cation inward flow into the cells of the nervous system [24]. In a situation of relatively mild cerebral hypoxia, e.g., due to insufficient respiration, this increased inflow might mean the difference between a self-limited disorder and manifest and potentially lethal brain edema. However, this locus was not found to be associated with specific SIDS subsets in the following stratified analysis, suggesting a more general effect. It is possible that SIDS risk factors interacting with this locus were not included in the stratified analysis, such as maternal smoking and maternal alcohol consumption. In previous studies on cerebral edema in SIDS, it was reported that maternal smoking in conjunction with some genetic risk factors showed a borderline association with SIDS, and SIDS cases with maternal alcohol consumption were observed with increased weight ratios of brain to body [9, 12]. Regrettably, maternal smoking and alcohol consumption, as possible co-acting factors, were not included in the present study.
Regarding the 8 SNP loci with statistical significance in the stratified analysis, the locus of greatest interest was rs4148622 (ABCC8), as it was associated with SIDS in multiple stratified analyses. It was reported by Jha et al. that the wild allele at this SNP could be used for predicting 3-month outcomes of cerebral edema after severe TBI [28], indicating that this polymorphism might be associated with the development of brain edema. The effect allele G of rs4148622 was linked to higher mRNA levels of ABCC8 in the brain tissues according to the eQTL analysis from the GTEx database. Therefore, one would expect to find an accumulation of the G allele in SIDS. However, the opposite was the case: the frequency of the G allele was lower in SIDS. Nevertheless, higher mRNA levels do not necessarily indicate increased protein expression, as the probe used for the eQTL analysis might just have recognized one splicing isoform: Rs4148622 and its proxy loci (rs2355017 and rs4757516) act as possible splicing variants and might influence the spatial structure of the SUR1 protein, possibly impairing the assembly of the subunits of the SUR1-TRPM4 complex [28]. Considering this, the low frequency of the G allele in SIDS fits well to the hypothesis of SIDS and genetically determined brain edema as postulated by Opdal et al. [11,12,13].
For rs7105832 and rs3819521 in ABCC8 that were also associated with subgroups of SIDS in the present study, several studies demonstrated a relation to cerebral edema or increased intracranial pressure [28, 29]. It was demonstrated that the variant allele of rs7105832 was associated with increased average intracranial pressure (ICP) in cerebral edema patients [28], and that the rare homozygous genotype of rs3819521 was linked to increased odds of CT edema after TBI [29].
Interestingly, the ABCC8 locus and specifically the variant rs3758953 in this study have been reported to be associated with type 2 diabetes, and the carriers of the risk genotypes of rs3758953 had higher levels of both glucose and insulin [32]. It has been shown that hyperglycemia causes the outflow of intracellular water into the tissue interstitial space and thus edema [33].
Besides a potential role in brain edema, SUR1 and TRPM4 as important ion channels are expressed in several human organs such as the heart, brain, and pancreas. Therefore, their physiological roles are diverse and thus could contribute to the individual SIDS risk in more ways than just via brain edema: Loss-of-function variants in ABCC8 or TRPM4 can cause lethal cardiovascular and metabolic genetic disorders, such as congenital hyperinsulinism, Brugada syndrome, or long QT syndrome (LQTS), potentially leading to sudden infant death instead of genuine SIDS [34,35,36,37,38,39]. In a recent study, 2 of 45 victims from sudden unexplained death (in adults) were reported to show a deletion in the coding region of the TRPM4 gene [40]. In a polygenic context for SIDS etiology, multiple genetic and external risk factors may contribute to SIDS simultaneously rather than one genetic variant leading to accepted genuine SIDS. It should, however, be stressed that the specific loss-of-function variants causing the above-mentioned lethal genetic disorders were not studied in the present study.
Some of the variants in genes ABCC8 (rs7950189, and rs7112138) and TRPM4 (rs11083962) studied herein reached significant results in different subgroups; however, no previous studies reporting their related association with other diseases could be found. Nevertheless, for these loci was demonstrated by the eQTL analysis that they influence gene expression and thus may make carriers of these loci more susceptible to SIDS. The haplotype analysis demonstrated that the haplotypes in ABCC8 and TRPM4, consisting of risk alleles of partial SNPs, were associated with SIDS. Although the frequency of risk haplotypes is low (< 5%), the results suggest that variants may combine to modulate the risk of SIDS.
Several potential limitations in this study should be mentioned. Firstly, all nominal significant results, after multiple testing corrections, no longer reached the required level of significance (although rs4148622 came close). Therefore, future studies involving larger sample sizes should be performed to validate our findings. Secondly, as limited information on their biological functions is available for some loci tested herein, it is needed to be careful when interpreting their potential roles in SNP-mediated SIDS etiology. Thirdly, some well-known SIDS risk factors linked to cerebral edema like maternal smoking and alcohol consumption have not been included in the present study as related records were not available to us.
In summary, we investigated for the first time the association of genetic variants involved in the SUR1-TRPM4 non-selective cation channel genes related to brain edema with SIDS. Despite these promising results, further studies with a larger sample size are supposed to confirm our results. Even more so, it would be informative if functional studies are conducted in the future to determine the function of risk genotypes and to be better able to interpret their impact on the pathogenesis of SIDS.
References
Krous HF, Beckwith JB, Byard RW et al (2004) Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics 114:234–238. https://doi.org/10.1542/peds.114.1.234
Bajanowski T, Vege A, Byard RW et al (2007) Sudden infant death syndrome (SIDS)–standardised investigations and classification: recommendations. Forensic Sci Int 165:129–143. https://doi.org/10.1016/j.forsciint.2006.05.028
Guntheroth WG, Spiers PS (2002) The triple risk hypotheses in sudden infant death syndrome. Pediatrics 110: e64-e.
Aranda FJ, Teixeira F, Becker LE (1990) Assessment of growth in sudden infant death syndrome. Neuroepidemiology 9:95–105. https://doi.org/10.1159/000110756
Goldwater PN (2003) Sudden infant death syndrome: a critical review of approaches to research. Arch Dis Child 88:1095–1100. https://doi.org/10.1136/adc.88.12.1095
Kadhim H, Sébire G, Khalifa M et al (2005) Incongruent cerebral growth in sudden infant death syndrome. J Child Neurol 20:244–246. https://doi.org/10.1177/088307380502000303
Shaw CM, Siebert JR, Haas JE, Alvord EC Jr (1989) Megalencephaly in sudden infant death syndrome. J Child Neurol 4:39–42. https://doi.org/10.1177/088307388900400106
Siebert JR, Haas JE (1994) Organ weights in sudden infant death syndrome. Pediatr Pathol 14:973–985. https://doi.org/10.3109/15513819409037694
Studer J, Bartsch C, Haas C (2014) Aquaporin-4 polymorphisms and brain/body weight ratio in sudden infant death syndrome (SIDS). Pediatr Res 76:41–45. https://doi.org/10.1038/pr.2014.59
Falck G, Rajs J (1995) Brain weight and sudden infant death syndrome. J Child Neurol 10:123–126. https://doi.org/10.1177/088307389501000212
O’Kusky JR, Kozuki DE, Norman MG (1995) Sudden infant death syndrome: postnatal changes in the volumes of the pons, medulla and cervical spinal cord. J Neuropathol Exp Neurol 54:570–580
Opdal SH, Vege A, Stray-Pedersen A, Rognum TO (2010) Aquaporin-4 gene variation and sudden infant death syndrome. Pediatr Res 68:48–51. https://doi.org/10.1203/PDR.0b013e3181df4e7c
Opdal SH, Ferrante L (2021) Aquaporin-1 and aquaporin-9 gene variations in sudden infant death syndrome. 135: 719–25. doi: https://doi.org/10.1007/s00414-020-02493-9
Opdal SH, Vege Å, Stray-Pedersen A, Rognum TO (2017) The gene encoding the inwardly rectifying potassium channel Kir4.1 may be involved in sudden infant death syndrome. Acta paediatrica (Oslo, Norway : 1992) 106: 1474–80. https://doi.org/10.1111/apa.13928
Manley GT, Binder DK, Papadopoulos MC, Verkman AS (2004) New insights into water transport and edema in the central nervous system from phenotype analysis of aquaporin-4 null mice. Neuroscience 129:983–991. https://doi.org/10.1016/j.neuroscience.2004.06.088
Ishikawa T, Yasui M (2021) [Water transportation during cerebral edema formation and aquaporin-4]. Brain and nerve = Shinkei kenkyu no shinpo 73: 983–9. https://doi.org/10.11477/mf.1416201875
Kitchen P, Salman MM, Halsey AM et al (2020) Targeting aquaporin-4 subcellular localization to treat central nervous system edema. Cell 181:784–99.e19. https://doi.org/10.1016/j.cell.2020.03.037
Eidahl JML, Stray-Pedersen A, Rognum TO, Opdal SH (2021) Aquaporin 4 expression in the hippocampus in sudden infant death syndrome and sudden unexplained death in childhood. J Chem Neuroanat 115:101962. https://doi.org/10.1016/j.jchemneu.2021.101962
Nagelhus EA, Mathiisen TM, Ottersen OP (2004) Aquaporin-4 in the central nervous system: cellular and subcellular distribution and coexpression with KIR4.1. Neuroscience 129:905–913. https://doi.org/10.1016/j.neuroscience.2004.08.053
Mehta RI, Tosun C, Ivanova S et al (2015) Sur1-Trpm4 cation channel expression in human cerebral infarcts. J Neuropathol Exp Neurol 74:835–849. https://doi.org/10.1097/nen.0000000000000223
Woo SK, Tsymbalyuk N, Tsymbalyuk O, Ivanova S, Gerzanich V, Simard JM (2020) SUR1-TRPM4 channels, not K(ATP), mediate brain swelling following cerebral ischemia. Int J Mol Sci 718:134729. https://doi.org/10.3390/ijms21020409,DOI:10.1016/j.neulet.2019.134729
Simard JM, Kahle KT, Gerzanich V (2010) Molecular mechanisms of microvascular failure in central nervous system injury–synergistic roles of NKCC1 and SUR1/TRPM4. J Neurosurg 113:622–629. https://doi.org/10.3171/2009.11.jns081052
Stokum JA, Kwon MS, Woo SK et al (2018) SUR1-TRPM4 and AQP4 form a heteromultimeric complex that amplifies ion/water osmotic coupling and drives astrocyte swelling. Glia 66:108–125. https://doi.org/10.1002/glia.23231
Jha RM, Bell J, Citerio G (2020) Role of sulfonylurea receptor 1 and glibenclamide in traumatic brain injury: a review of the evidence. 21. https://doi.org/10.1038/s41401-020-00503-5, https://doi.org/10.3390/ijms21020409
Kahle KT, Luo ZW, Ovcjak A et al (2020) Drug development in targeting ion channels for brain edema. Expert Opin Investig Drugs 41:1272–1288. https://doi.org/10.1080/13543784.2020.1813715,DOI:10.1038/s41401-020-00503-5
Ortega FJ, Gimeno-Bayon J, Espinosa-Parrilla JF et al (2012) ATP-dependent potassium channel blockade strengthens microglial neuroprotection after hypoxia-ischemia in rats. Exp Neurol 235:282–296. https://doi.org/10.1016/j.expneurol.2012.02.010
Jha RM, Desai SM, Zusman BE et al (2019) Downstream TRPM4 polymorphisms are associated with intracranial hypertension and statistically interact with ABCC8 polymorphisms in a prospective cohort of severe traumatic brain injury. J Neurotrauma 36:1804–1817. https://doi.org/10.1016/j.neulet.2019.134729,DOI:10.1089/neu.2018.6124
Jha RM, Koleck TA, Puccio AM et al (2018) Regionally clustered ABCC8 polymorphisms in a prospective cohort predict cerebral oedema and outcome in severe traumatic brain injury. J Neurol Neurosurg Psychiatry 89:1152–1162. https://doi.org/10.1136/jnnp-2017-317741
Jha RM, Puccio AM, Okonkwo DO et al (2017) ABCC8 single nucleotide polymorphisms are associated with cerebral edema in severe TBI. Neurocrit Care 26:213–224. https://doi.org/10.1007/s12028-016-0309-z
Meißner L, Schürmann P, Dörk T, Hagemeier L, Klintschar M (2021) Genetic association study of fatal pulmonary embolism 135:143–151. https://doi.org/10.1007/s00414-020-02441-7
Kerz J, Schürmann P, Rothämel T, Dörk T, Klintschar M (2021) Gene variants associated with obstructive sleep apnea (OSA) in relation to sudden infant death syndrome (SIDS). 135: 1499–506. https://doi.org/10.1007/s00414-020-02480-0
Kilpeläinen TO, Lakka TA, Laaksonen DE et al (2007) Physical activity modifies the effect of SNPs in the SLC2A2 (GLUT2) and ABCC8 (SUR1) genes on the risk of developing type 2 diabetes. Physiol Genomics 31:264–272. https://doi.org/10.1152/physiolgenomics.00036.2007
Bohn D, Daneman D (2002) Diabetic ketoacidosis and cerebral edema. Curr Opin Pediatr 14:287–291. https://doi.org/10.1097/00008480-200206000-00001
Brunetti-Pierri N, Olutoye OO, Heptulla R, Tatevian N (2008) Case report: pathological features of aberrant pancreatic development in congenital hyperinsulinism due to ABCC8 mutations. Ann Clin Lab Sci 38:386–389
Celik N, Cinaz P, Emeksiz HC et al (2013) Octreotide-induced long QT syndrome in a child with congenital hyperinsulinemia and a novel missense mutation (p.Met115Val) in the ABCC8 gene. Hormone research in paediatrics 80:299–303. https://doi.org/10.1159/000354666
Glaser B, Ryan F, Donath M et al (1999) Hyperinsulinism caused by paternal-specific inheritance of a recessive mutation in the sulfonylurea-receptor gene. Diabetes 48:1652–1657. https://doi.org/10.2337/diabetes.48.8.1652
Vaxillaire M, Dechaume A, Busiah K et al (2007) New ABCC8 mutations in relapsing neonatal diabetes and clinical features. Diabetes 56:1737–1741. https://doi.org/10.2337/db06-1540
Hof T, Liu H, Sallé L et al (2017) TRPM4 non-selective cation channel variants in long QT syndrome. BMC Med Genet 18:31. https://doi.org/10.1186/s12881-017-0397-4
Liu H, Chatel S, Simard C et al (2013) Molecular genetics and functional anomalies in a series of 248 Brugada cases with 11 mutations in the TRPM4 channel. PLoS ONE 8:e54131. https://doi.org/10.1159/000471792,DOI:10.1371/journal.pone.0054131
Neubauer J, Wang S, Russo G (2021) Re-evaluation of single nucleotide variants and identification of structural variants in a cohort of 45 sudden unexplained death cases. 135: 1341–9. doi: https://doi.org/10.1007/s00414-021-02580-5
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was financially supported by the CSC grant no. 201908440466 (D.Q.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the local ethics committee at Hannover Medical School.
Informed consent
Not applicable.
Human and animal rights
No animal experiments/No experiments with humans.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qu, D., Schürmann, P., Rothämel, T. et al. Variants in genes encoding the SUR1-TRPM4 non-selective cation channel and sudden infant death syndrome (SIDS): potentially increased risk for cerebral edema. Int J Legal Med 136, 1113–1120 (2022). https://doi.org/10.1007/s00414-022-02819-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-022-02819-9