Abstract
Introduction
Postmortem multi-detector computed tomography (PMCT) has become an important part in forensic imaging. Modern reconstruction techniques such as iterative reconstruction (IR) are frequently used in postmortem CT angiography (PMCTA). The image quality of PMCTA depends on the strength of IR. For this purpose, we aimed to investigate the impact of different advanced IR levels on the objective and subjective PMCTA image quality.
Material and methods
We retrospectively analyzed the coronary arteries of 27 human cadavers undergoing whole-body postmortem CT angiography between July 2017 and March 2018 in a single center. Iterative reconstructions of the coronary arteries were processed in five different level settings (0%; 30%; 50%; 70%; 100%) by using an adaptive statistical IR method. We evaluated the objective (contrast-to-noise ratio (CNR)) and subjective image quality in several anatomical locations.
Results
Our results demonstrate that the increasing levels of an IR technique have relevant impact on the image quality in PMCTA scans in forensic postmortem examinations. Higher levels of IR have led to a significant reduction of image noise and therefore to a significant improvement of objective image quality (+ 70%). However, subjective image quality is inferior at higher levels of IR due to plasticized image appearance.
Conclusion
Objective image quality in PMCTA progressively improves with increasing level of IR with the best CNR at the highest IR level. However, subjective image quality is best at low to medium levels of IR. To obtain a “classic” image appearance with optimal image quality, PMCTAs should be reconstructed at medium levels of IR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postmortem multi-detector computed tomography has become an important part in forensic imaging. The number of postmortem CT (PMCT) examinations has increased significantly over the last decades such that PMCT has established into forensic routine [1]. Studies indicate an important impact of PMCT on the detection rate of relevant findings compared to conventional autopsy [2, 3]. Moreover, the quality of diagnostic performance increases by combining these methods [3].
However, unenhanced PMCT, as opposed to contrast-enhanced CT, is limited by low soft tissue contrast, associated with the disability to detect important findings like aortic ruptures or myocardial infarction [1, 4, 5]. Resulting from this limitation, the contrast media-based postmortem CT angiography (PMCTA) has been introduced. According to Grabherr et al., PMCTA improves the detection of soft tissue and vascular findings compared to PMCT performed without contrast media and conventional autopsy [4, 5]. Therefore, PMCTA has become an important part of the workup routine in forensic imaging [5]. Current studies demonstrate that postmortem coronary CT angiography (PMCCTA) could be considered a valid and useful tool for the detection of coronary artery disease and myocardial infarction [6]. Since the introduction of PMCTA, different techniques and contrast substances, such as ioxithalamate, diesel oil, and oily liquids, were analyzed [7,8,9]. Nowadays, multiphase PMCTA protocol using oily contrast agents has established into forensic routine and reflects the worldwide most used angiographic technique [5]. In literature, a different coronary PMCTA technique called targeted coronary angiography (TCA) is introduced [10, 11]. TCA is a less invasive method which injects the contrast agent via a blocked urinary catheter into the ascending aorta and thereby in the coronary arteries [10, 11]. Studies analyzing the performance of TCA revealed a good correlation for identifying coronary lesions and therefore for investigating CAD, by comparing with conventional autopsy and histological investigations [12, 13].
Iterative reconstruction (IR) techniques have been introduced into radiological CT diagnostic as a reliable method to reduce image noise [14]. The underlying method of IR techniques varies with vendor and software. In general, IR methods use correction loops to progressively refine image data and to separate image information from noise. The reduced image noise can be used to lower the radiation exposure while maintaining image quality when imaging living patients [14]. IR techniques are nowadays frequently used in clinical routine as well as in postmortem CT and have replaced the traditional filtered back projection (FBP) in many applications. However, studies reported a limited value of higher IR levels due to altering of the “classic” image appearance, causing a blotchy or aquarelle-like image impression [15, 16]. Noise suppression may reduce the coarseness of images but might at the same time remove small details which impedes the diagnostic quality of an image, though recent advanced IR systems, such as model-based IR, are even more powerful with respect to reducing and preventing artifacts than adaptive statistical IR [16,17,18,19].
Since IR reduces image noise and while clinical radiologists are used to the image impression of IR-processed images in daily routine, it is desirable to acquire images in PMCT using the same reconstruction method. However, the optimal choice of the level of noise suppression depends on the type of CT examination. In PMCT, the situation is different from the clinical setting and dose reduction is less relevant. Because the higher radiation dose in PMCT results in less image noise compared to clinical routine CT, optimal IR levels for noise suppression may differ between PMCT and clinical CT examinations. Further, the IR level specifically needs to be evaluated for different PMCT protocols (e.g., PMCT of the coronary arteries) in terms of quantitative and qualitative image quality [20]. For this purpose, we aimed to investigate the impact of different levels of IR on the objective and subjective image quality in PMCTA.
Materials and methods
Cadavers
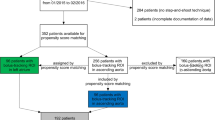
We retrospectively analyzed the coronary arteries of 38 human cadavers undergoing whole-body postmortem CT angiography and conventional autopsy between July 2017 and March 2018 in a single center. As this was a retrospective study and data were treated anonymously, a specific ethical approval was not necessary according to an agreement with the local justice department and the ethical standards. The cadavers showed different causes of death, e.g., myocardial infarction, intoxication, trauma, or death by drowning. All cadavers received a full-body PMCTA after a detailed forensic examination and prior to conventional autopsy. As the time of death is unknown, an exact calculation of the postmortem interval (death to PMCT) cannot be given; however, it ranged from half a day to 3 days maximum (with storage in the refrigerating room).
Of the 38 examined cadavers, 10 cadavers were eventually excluded from the analysis due to lack of contrast in the coronary arteries and 1 due to heavily calcified coronary arteries (see Fig. 1). The remaining 27 cadavers included 9 female and 18 male cadavers with a mean age of 55.5 ± 19.7 years (range 19–92 years).
Scan protocol
Three-phasic (arterial, venous, and dynamic) PMCTA was performed on a 64-row CT scanner (GE LightSpeed VCT, GE HealthCare, Milwaukee, WI, USA) by using the standardized protocol with the following scan parameters: tube potential 120 kVp, automatically modulated tube current 200–400 mA, noise index 20, pitch 0.984, tube rotation time 0.8 s, and scan field of view (FOV) 50 cm (see Table 1). Tube current was automatically modulated to obtain a constant image quality within a cadaver. The CT acquisition covered the vertex to the trochanters, with arm positions along the body. Identical protocol settings for CT acquisition were used for all three phases. The volumetric CT dose index (CTDIvol) and the dose-length product (DLP) were recorded for all cadavers for the arterial phase.
The preparation process was similar to previous studies [3, 4]. Specific single-use sets for femoral vascular cannulation were applied before the injection of a contrast agent mixture of an oil-based solution of defined viscosity (mixture of paraffin oil [paraffinum liquidum] with 6% oil-based contrast agent [Angiofil; Fumedica, Muri, Switzerland]).
According to the protocol of Grabherr et al., the injection included an arterial, venous, and dynamic phase with a volume of 1200 ml and a flow rate of 800 ml/min for the arterial phase [4].
Image reconstruction
Using the raw image data of the arterial phase acquisition, a secondary reconstruction centered on the cardiac region was performed including the aortic arch or the carina down to the diaphragm with a mean scan length of 180.2 ± 24.1 mm (range 130–228 mm). In case of coronary artery bypass graft surgery, the z-axis was extended. We only analyzed the coronary reconstruction of the arterial phase.
Axial images were reconstructed for the heart with a slice thickness of 0.625 mm at a reconstruction increment of 0.400 mm with a FOV of 25 cm (matrix size 512 × 512 pixels) (see Table 1). Iterative reconstructions (IR) of the cardiac region were processed in five levels (0%; 30%; 50%; 70%; 100%) defining the strength of the IR algorithm increasing from 0 to 100%. Adaptive statistical iterative reconstruction (ASiR; GE HealthCare, Milwaukee, WI, USA) was used for all reconstructions. Reconstruction of all cardiac region datasets at all IR levels resulted in 135 image datasets (27 included cadavers × 5 ASiR levels).
Image analysis
Objective image quality
First, we evaluated the objective image quality (IQ) of the 135 datasets, adapting a previously validated method [21]. The measurements were obtained by one radiologist (AAA; 3 years of expertise in reading PMCT). For this purpose, circular regions-of-interest (ROIs) were drawn into the lumen of the coronary arteries (as large as possible, 2–20 mm2) (Fig. 2) in nine locations [21]: left main coronary artery (LM), proximal and distal (distal to the second diagonal branch) left anterior descending coronary artery (LAD), proximal first diagonal branch (D1), proximal and distal left circumflex coronary artery (LCX), first obtuse marginal branch (OM1), and proximal and distal (proximal to the origin of the posterior descending coronary artery) right coronary artery (RCA).
Furthermore, ROIs were drawn in the paravertebral musculature as background measurement (100 mm2), in the ascending and descending aorta (each 100 mm2) and in the adjacent air (100 mm2) to determine the changes in CT numbers for varying levels of IR. In addition, another circular ROI (100 mm2) was placed in the contrast-enhanced lumen of the aortic root to measure the image noise by determining the standard deviation of CT numbers [21]. Every ROI measurement had the exact same size and position in the five levels of iterative reconstruction by transferring the ROI into the different reconstruction levels.
The signal-to-noise ratio (SNR) was analyzed for all 9 coronary locations using the following formula:
The contrast-to-noise ratio (CNR) was analyzed for all 9 coronary locations using the following formula:
Subjective image quality
The subjective image quality was independently evaluated by two radiologists (JB (J Boeven) and LC; 3 and 2 years of experience in reading, respectively). A four-point scale (1 = excellent image quality: “classic” image appearance, no or minimal artifacts, fully diagnostic; 2 = good image quality: slight artifacts, but fully diagnostic; 3 = moderate image quality: relevant artifacts, but evaluable concerning the presence of stenosis; 4 = unevaluable) based on the 18-segment model of the Society of Cardiovascular Computed Tomography was used (based on Society of Cardiovascular Computed Tomography [22]). The main criteria of subjective image quality were on the one hand “classic” image appearance (CT image appearance as known by and familiar to radiologists), which might be influenced by the use of too high IR levels causing blotchy image appearance and on the other hand artifacts due to image noise, resulting from low levels or absent IR. A comparable four-point scale was already applied in a previous study [21].
Subjective scores were given for seven localizations: the complete thorax, left main coronary artery (LM), left anterior descending coronary artery (LAD), left circumflex coronary artery (LXC), right coronary artery (RCA), and ascending and descending aorta, resulting in n = 27 cadavers x 5 reconstruction levels × 7 localizations x 2 readers = 1890 scores.
Statistical analysis
A commercially available software (Microsoft Excel 2016, Redmond, WA, USA; SPSS, 27.0, Inc., Chicago, IL, USA) was used to perform statistical analysis. Continuous data are expressed as mean ± SD. Differences in objective and subjective image quality among the five levels of IR were calculated by means of a Bonferroni-corrected Friedman test with pairwise comparisons and a post hoc Dunn test. In addition, the number of diagnostic images (subjective image quality 1 and 2) between the five ASiR levels was compared and statistical differences tested by means of a Cochran Q test for dependent samples and a post hoc Dunn test. A two-tailed p value < 0.05 was considered statistically significant.
Inter-observer agreement was determined using a Fleiss kappa with chance correction according to Brennan and Prediger [23]. Inter-observer agreement was defined as excellent (κ > 0.81), good (κ = 0.61–0.80), moderate (κ = 0.41–0.60), fair (κ = 0.21–0.40), and poor (κ ≤ 0.20) [24].
Results
Radiation exposure
Averaged over all cadavers, the effective tube current time product of the arterial phase was 305.0 ± 38.2 mAs at 120kVp. The average CTDIvol and DLP for the 27 cadavers were 21.7 ± 2.9 mGy and 2368.5 ± 519.5 mGy∙cm, respectively, for the arterial phase.
Objective image quality
The CT numbers were comparable across the different IR levels in the aortic root, the ascending and descending aorta, paravertebral muscle and air (range aortic root, 555.7–555.8 HU; range aorta asc., 559.4–559.5 HU; range aorta desc., 551.0–551.5 HU; paravertebral muscle, 60.2–60.4 HU; air − 992.0–− 991.9 HU). Although the described ranges were within 1 HU when averaging over all 27 cadavers, there was a significant difference in the CT numbers between IR level 0 and 100 for the paravertebral muscle (p = 0.011), when employing the Friedman test. However, differences in CT numbers between the applied IR levels in the muscle were maximum 2 HU. Image noise decreased from IR level 0 to 100 in the aortic root (− 39%), paravertebral muscle (− 24%), and air (− 51%). The corresponding CT numbers in the coronary arteries (ROI size: 1–20 mm2) showed lower values with increasing IR levels with the highest mean value in level 0% (471.4 ± 120.8 HU, range 202.5 to 1060.3 HU) and the lowest mean value in level 100% (445.6 ± 133.2 HU, range 147.8 to 1072.5 HU). Compared to the highest CT number at IR level 0, CT numbers were 5.5% lower at IR level 100. Changes in mean CT number among the five IR levels were statistically significant (p < 0.001 for all comparisons).
For the different IR levels, the mean SNRs for the nine coronary artery localizations were 7.8 ± 3.6 (0%), 8.5 ± 4.3 (30%), 9.0 ± 5.0 (50%), 9.5 ± 5.6 (70%), and 10.3 ± 6.4 (100%) (see Fig. 3a). The mean SNR significantly improved with each increasing level of IR, by 31% from IR level 0 to 100. The highest SNR was found at the highest level of IR (100%). For the different IR levels, the mean CNRs for the nine coronary artery localizations were 12.1 ± 3.9 (0%), 14.0 ± 4.8 (30%), 15.5 ± 5.6 (50%), 17.4 ± 6.6 (70%), and 20.5 ± 8.5 (100%). The mean CNR significantly improved with each increasing level of IR (see Fig. 3b), by 70% from IR level 0 to 100. The highest CNR was found at the highest level of IR (100%).
Subjective image quality
An excellent image quality with a score of 1 was assessed 854 times (45.2%), score 2 (“good”) was assessed 611 times (32.2%), score 3 (“moderate”) 389 times (20.6%), and score 4 (“unevaluable”) 36 (1.9%) times.
Looking at the different IR levels, the subjective image quality was evaluated best at the IR level 30 with a mean score of 1.20 ± 0.47, following IR level 50 (1.25 ± 0.47), IR level 0 (1.74 ± 0.67), IR level 70 (1.98 ± 0.71), and at last IR level 100 (2.79 ± 0.63) (see Fig. 4). Subjective image score did not differ significantly between IR level 30 and 50. The score 4 (“unevaluable”) was given 32 times in IR level 100 and 4 times in IR level 70, whereas there was no localization in IR level 0, 30, or 50 that was evaluated with score 4. Subjective image quality was rated diagnostic (score 1 and 2) for IR level 50% in 98.4% of the evaluated ROIs, followed by IR level 30 (97.1%) and IR level 0 (87.3%). Cochran’s Q test indicated differences in the number of diagnostic and non-diagnostic ROI scores between the five IR levels (Χ2(4, N = 378) = 712.2, p < 0.001). Compared to IR level 0 (full FBP), IR levels 30 and 50 had significantly more diagnostic scores (p = 0.017 and p = 0.004, respectively), whereas IR levels 70 and 100 had significantly less diagnostic scores (p = 0.023 and p < 0.001, respectively) (see Fig. 5). No statistical significant difference was noted between IR level 30 and 50. The influence of the IR level on the image quality is depicted in Figs. 6 and 7. With increasing level, images appear less noisy. However, small details also appear blurred and the total image appearance looks plasticized, compared to the lower levels of IR.
The inter-observer agreement regarding the subjective image quality analysis was moderate (0.55 ± 0.16) and varied between 0.30 (IR level 70, fair agreement) and 0.73 (IR level 30 good agreement).
Discussion
In the presented study, multiphase PMCTA was applied and evaluated in 27 cadavers resulting in a consistently diagnostic image quality and a good visualization of coronary arteries. Since the selection and volume of a dedicated contrast agent and the used CTA technique are relevant parts of image quality and image impression, we employed the most utilized and proven technique in PMCTA. Published clinical studies that analyzed the impact of advanced IR are often limited by employing diverse flow rates and amounts of contrast agents within one study [21]. In our study, we solely used the same amount of contrast media and the same flow rate.
Iterative reconstruction techniques are well established in CTA of patients due to the extensive and positive experience from clinical routine by means of radiation dose savings, noise reduction, and improvement of low-dose image quality. Regarding the image quality in cardiac CT, several studies pointed out an improvement of the CNR and subjective image quality by using IR techniques [25,26,27].
The employed CT protocol was a standardized protocol for PMCTA in the institute. In contrast to clinical protocols, the PMCT protocol did not specifically aim for a low radiation dose. This distinguishes the purpose of IR in clinical CT (aim for an additional dose reduction) and PMCT (aim for a classic image appearance as available in clinical CT). The dissimilar properties of alive patients and cadavers, e.g., heart movement, and the different requirements for an appropriate CT protocol impede the comparability of CT protocols and radiation exposure. Advanced IR techniques use multiple iterative reconstruction steps resulting in a progressive improvement of the CNR and subjective image quality in cardiac CT [28, 29]. A study by Kroepil et al. demonstrated that an increasing level of IR led to an improvement of the objective image quality, while the subjective image quality was limited by modification of the “classic” image appearance towards looking more plastic at higher IR levels [21]. Lack of familiarity of the image appearance might cause missing diagnoses, since the radiologist might misinterpret manifestations or structures, which appear different with different IR levels or vendors. The optimal IR level might differ between different types of CT examinations and should be evaluated when establishing a standard protocol [20]. In our study, objective image quality increased significantly with higher levels of IR due to the decreasing image noise (Fig. 3). The CT values in the coronary arteries decreased with increasing IR level, possibly due to partial volume effects with surrounding tissues with lower CT values. Subjective image analysis demonstrated that the coronary artery images appear increasingly blurry and plasticized at higher IR levels (Figs. 6 and 7). The overall image quality was rated best (1.2, excellent image quality) at the IR level of 30% (Fig. 4), with no significant differences between IR level of 30% and 50% for subjective image quality and number of diagnostic ROIs. Hence, our results are similar to what has been published for coronary CTA studies in living patients [21]. The authentic CT image appearance that radiologists are used to in clinical routine was preserved at low and medium levels of IR (ASiR 30% and 50%).
Forensic PMCTA reports should always be prepared in conjunction with a radiologist since otherwise, important findings can remain unreported [3]. Most forensic radiologists are adapted to common clinical CT image appearance produced by iterative reconstructions. Therefore, employing medium levels of IR is reasonable even in PMCT scans, as radiologists are familiar with the image appearance. Numerous forensic PMCT studies use filtered back projection (FBP) techniques or do not specify their CT protocols and image processing in detail [30,31,32].
Our study has some limitations. First, we used a retrospective study design with a limited cohort size. Second, a systematic comparison of coronary artery imaging and conventional autopsy has not been performed as the primary aim of this study was the impact on image quality and not the detection rate of coronary artery diseases. Third, the applied contrast agent was not visible in all regions for all cadavers due to cardiac pathologies, such as extravasation after cardiac damage and artifacts like contrast layering or filling defects [33]. There have been ten cadavers with only little or no contrast media in some ROIs, causing highly deviating CT values for these cadavers in the assessed ROIs. For this purpose, we excluded those ten cadavers. Fourth, we only investigated one IR system (ASiR) and one CT scanner of only one manufacturer. Although we cannot generalize our results to reflect all IR algorithms (especially newer ones), the general principle of decreasing image noise with increasing levels of IR also applies to other vendors [21, 34, 35]. Fifth, the rated subjective image quality always depends on the experience of the rating radiologist and the image quality a radiologist is used to. The two radiologists’ inter-reader agreement in this study varied between fair and good. Possible reasons could be the two radiologists’ relatively young reading experience (2 and 3 years), which might reinforce differences in image quality evaluation. Still, both radiologists are familiar in reading postmortem CTs. For different radiologists, e.g., more experienced ones, subjective image quality might differ from the results presented here. When defining institutional protocol settings, radiologists of the institution might rate image quality in consensus to obtain the optimal settings. Last, we did not include the body mass index (BMI) of the cadavers into our analysis, due to incomplete data. For a group of thinner or bigger patients, image quality might differ from the included cohort. However, we do not expect large differences since we had both normal (BMI 19.8 kg/m2) and obese patients (BMI 38.9 kg/m2) included.
Until now, clinical studies have usually evaluated to what degree IR methods enable reducing the effective dose to the patient. This is not the aim of IR in forensic radiology, since the radiation exposure has no negative implication to the examined cadavers. The question remains whether FBP with high-dose levels work better or equal than IR with lower-dose levels. As mentioned in the introduction, several published studies employ FBP as method of image reconstruction, since IR methods are not available in all forensic institutes (cost-intensive purchase, requirement of a state-of-the-art CT scanner). In case IR is available on the CT scanners, then it is presumably not the most modern IR algorithm. In a future study, it is of interest to assess whether increasing the dose in PMCT in combination with FBP outperforms the current protocol with optimal IR level, in terms of diagnostic accuracy and confidence and image appearance.
Conclusion
In PMCTA, objective image quality progressively improves with increasing level of ASiR in the coronary arteries with the best CNR at the highest noise suppression level. Subjective image quality was rated significantly better at low and medium levels of IR, as the “classic” image appearance was preserved. Thus, for PMCTA, a medium level of ASiR seems optimal.
References
Norberti N, Tonelli P, Giaconi C, Nardi C, Focardi M, Nesi G, Miele V, Colagrande S (2019) State of the art in post-mortem computed tomography: a review of current literature. Virchows Arch 475:139–150. https://doi.org/10.1007/s00428-019-02562-4
Chevallier C, Doenz F, Vaucher P et al (2013) Postmortem computed tomography angiography vs. conventional autopsy: advantages and inconveniences of each method. Int J Legal Med 127:981–979. https://doi.org/10.1007/s00414-012-0814-3
Grabherr S, Heinemann A, Vogel H, Rutty G, Morgan B, Woźniak K, Dedouit F, Fischer F, Lochner S, Wittig H, Guglielmi G, Eplinius F, Michaud K, Palmiere C, Chevallier C, Mangin P, Grimm JM (2018) Postmortem CT angiography compared with autopsy: a forensic multicenter study. Radiology 288:270–276. https://doi.org/10.1148/radiol.2018170559
Grabherr S, Doenz F, Steger B, Dirnhofer R, Dominguez A, Sollberger B, Gygax E, Rizzo E, Chevallier C, Meuli R, Mangin P (2011) Multi-phase post-mortem CT angiography: development of a standardized protocol. Int J Legal Med 125:791–802. https://doi.org/10.1007/s00414-010-0526-5
Grabherr S, Grimm J, Dominguez A, Vanhaebost J, Mangin P (2014) Advances in post-mortem CT-angiography. Br J Radiol 87:20130488. https://doi.org/10.1259/bjr.20130488
De Marco E, Vacchiano G, Frati P et al (2018) Evolution of post-mortem coronary imaging: from selective coronary arteriography to post-mortem CT-angiography and beyond. Radiol Med 123:351–358. https://doi.org/10.1007/s11547-018-0855-x
Jackowski C, Sonnenschein M, Thali MJ, Aghayev E, Allmen G, Yen K, Dirnhofer R, Vock P (2005) Virtopsy: postmortem minimally invasive angiography using cross section techniques—implementation and preliminary results. J Forensic Sci 50:1–12. https://doi.org/10.1520/JFS2005023
Grabherr S (2009) Post-mortem angiography after vascular perfusion with diesel oil and a lipophilic contrast agent. In: Thali M, Dirnhofer R, Vock P (eds) The virtopsy approach—3D optical and radiological scanning and reconstruction in forensic medicine. CRC Press, Taylor & Francis
Grabherr S, Djonov V, Friess A, Thali MJ, Ranner G, Vock P, Dirnhofer R (2006) Postmortem angiography after vascular perfusion with diesel oil and a lipophilic contrast agent. AJR Am J Roentgenol 187:515–523. https://doi.org/10.2214/AJR.05.1394
Saunders SL, Morgan B, Raj V, Robinson CE, Rutty GN (2011) Targeted post-mortem computed tomography cardiac angiography: proof of concept. Int J Legal Med 125:609–616. https://doi.org/10.1007/s00414-011-0559-4
Roberts ISD, Benamore RE, Peebles C, Roobottom C, Traill ZC (2011) Diagnosis of coronary artery disease using minimally invasive autopsy: evaluation of a novel method of post-mortem coronary CT angiography (Technical Report). Clin Radiol 66:645–650. https://doi.org/10.1016/j.crad.2011.01.007
Rutty GN, Raj V, Saunders SL, Morgan B (2011) Air as a contrast medium for targeted post-mortem computed tomography cardiac angiography. Acad Forensic Pathol 1:144–145. https://doi.org/10.23907/2011.018
Morgan B, Biggs MJ, Barber J, Raj V, Amoroso J, Hollingbury FE, Robinson C, Rutty GN (2013) Accuracy of targeted post-mortem computed tomography coronary angiography compared to assessment of serial histological sections. Int J Legal Med 127:809–817. https://doi.org/10.1007/s00414-012-0790-7
Stiller W (2018) Basics of iterative reconstruction methods in computed tomography: a vendor-independent overview. Eur J Radiol 109:147–154. https://doi.org/10.1016/j.ejrad.2018.10.025
Singh S, Kalra K, Hsieh J et al (2010) Abdominal CT: comparison of adaptive statistical iterative and filtered back projection reconstruction techniques. Radiology 257:373–383. https://doi.org/10.1148/radiol.10092212/-/DC1
Morsbach F, Desbiolles L, Raupach R, Leschka S, Schmidt B, Alkadhi H (2017) Noise texture deviation: a measure for quantifying artifacts in computed tomography images with iterative reconstructions. Investig Radiol 52:87–94. https://doi.org/10.1097/RLI.0000000000000312
Örgel A, Bier G, Hennersdorf F, Richter H, Ernemann U, Hauser TK (2020) Image quality of CT angiography of supra-aortic arteries. Clin Neuroradiol 30:101–107. https://doi.org/10.1007/s00062-018-0740-y
Schmid AI, Uder M, Lell MM (2016) Reaching for better image quality and lower radiation dose in head and neck CT: advanced modeled and sinogram-affirmed iterative reconstruction in combination with tube voltage adaptation. Dentomaxillofacial Radiol 46. https://doi.org/10.1259/dmfr.20160131
Deák Z, Grimm JM, Treitl M, Geyer LL, Linsenmaier U, Körner M, Reiser MF, Wirth S (2013) Filtered back projection, adaptive statistical iterative reconstruction, and a model-based iterative reconstruction in abdominal CT: an experimental clinical study. Radiology 266:197–206. https://doi.org/10.1148/radiol.12112707
Barca P, Giannelli M, Fantacci ME, Caramella D (2018) Computed tomography imaging with the adaptive statistical iterative reconstruction (ASIR) algorithm: dependence of image quality on the blending level of reconstruction. Australas Phys Eng Sci Med 41:463–473. https://doi.org/10.1007/s13246-018-0645-8
Kröpil P, Bigdeli AH, Nagel HD, Antoch G, Cohnen M (2014) Impact of increasing levels of advanced iterative reconstruction on image quality in low-dose cardiac CT angiography. Rofo 186:567–575. https://doi.org/10.1055/s-0033-1356074
Kirişli HA, Schaap M, Metz CT, Dharampal AS, Meijboom WB, Papadopoulou SL, Dedic A, Nieman K, de Graaf MA, Meijs MFL, Cramer MJ, Broersen A, Cetin S, Eslami A, Flórez-Valencia L, Lor KL, Matuszewski B, Melki I, Mohr B, Öksüz I, Shahzad R, Wang C, Kitslaar PH, Unal G, Katouzian A, Orkisz M, Chen CM, Precioso F, Najman L, Masood S, Ünay D, van Vliet L, Moreno R, Goldenberg R, Vuçini E, Krestin GP, Niessen WJ, van Walsum T (2013) Standardized evaluation framework for evaluating coronary artery stenosis detection, stenosis quantification and lumen segmentation algorithms in computed tomography angiography. Med Image Anal 17:859–876. https://doi.org/10.1016/j.media.2013.05.007
Brennan RL, Prediger DJ (1981) Coefficient Kappa: some uses, misuses, and alternatives. Educ Psychol Meas 41:687–699
Schimmöller L, Lanzman RS, Heusch P, Dietrich S, Miese F, Aissa J, Heusner TA, Antoch G, Kröpil P (2013) Impact of organ-specific dose reduction on the image quality of head and neck CT angiography. Eur Radiol 23:1503–1509. https://doi.org/10.1007/s00330-012-2750-5
Moscariello A, Takx RAP, Schoepf UJ, Renker M, Zwerner PL, O’Brien TX, Allmendinger T, Vogt S, Schmidt B, Savino G, Fink C, Bonomo L, Henzler T (2011) Coronary CT angiography: image quality, diagnostic accuracy, and potential for radiation dose reduction using a novel iterative image reconstruction technique-comparison with traditional filtered back projection. Eur Radiol 21:2130–2138. https://doi.org/10.1007/s00330-011-2164-9
Oda S, Utsunomiya D, Funama Y, Yonenaga K, Namimoto T, Nakaura T, Yamashita Y (2012) A hybrid iterative reconstruction algorithm that improves the image quality of low-tube-voltage coronary CT angiography. Am J Roentgenol 198:1126–1131. https://doi.org/10.2214/AJR.11.7117
Renker M, Ramachandra A, Schoepf UJ, Raupach R, Apfaltrer P, Rowe GW, Vogt S, Flohr TG, Kerl JM, Bauer RW, Fink C, Henzler T (2011) Iterative image reconstruction techniques: applications for cardiac CT. J Cardiovasc Comput Tomogr 5:225–230. https://doi.org/10.1016/j.jcct.2011.05.002
Utsunomiya D, Weigold WG, Weissman G, Taylor AJ (2012) Effect of hybrid iterative reconstruction technique on quantitative and qualitative image analysis at 256-slice prospective gating cardiac CT. Eur Radiol 22:1287–1294. https://doi.org/10.1007/s00330-011-2361-6
Laqmani A, Buhk JH, Henes FO, Klink T, Sehner S, von Schultzendorff H, Hammerle D, Nagel H, Adam G, Regier M (2013) Impact of a 4th generation iterative reconstruction technique on image quality in low-dose computed tomography of the chest in immunocompromised patients. Rofo 185:749–757. https://doi.org/10.1055/s-0033-1335577
Flach PM, Gascho D, Schweitzer W, Ruder TD, Berger N, Ross SG, Thali MJ, Ampanozi G (2014) Imaging in forensic radiology: an illustrated guide for postmortem computed tomography technique and protocols. Forensic Sci Med Pathol 10:583–606. https://doi.org/10.1007/s12024-014-9555-6
Vester MEM, van Rijn RR, Duijst WLJM et al (2019) Added value of post-mortem computed tomography (PMCT) to clinical findings for cause of death determination in adult “natural deaths.”. Int J Legal Med. https://doi.org/10.1007/s00414-019-02219-6
Polacco M, Sedati P, Arena V, Pascali VL, Zobel BB, Oliva A, Rossi R (2015) Visualization of myocardial infarction by post-mortem single-organ coronary computed tomography: a feasibility study. Int J Legal Med 129:517–524. https://doi.org/10.1007/s00414-014-1085-y
Bruguier C, Grabherr S (2016) Radiologic artefacts of postmortem computed tomography angiography. In: Grabherr S., Grimm J., Heinemann A. (eds) Atlas of Postmortem Angiography. Springer, Cham. https://doi.org/10.1007/978-3-319-28537-5_19
Willemink MJ, De Jong PA, Leiner T et al (2013) Iterative reconstruction techniques for computed tomography part 1: technical principles. Eur Radiol 23:1623–1631. https://doi.org/10.1007/s00330-012-2765-y
von Falck C, Bratanova V, Rodt T, Meyer B, Waldeck S, Wacker F, Shin HO (2013) Influence of sinogram affirmed iterative reconstruction of CT data on image noise characteristics and low-contrast detectability: an objective approach. PLoS One 8:1–10. https://doi.org/10.1371/journal.pone.0056875
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consent was not available due to the imaging of human corpses. As this was a
retrospective study and data were treated anonymously, a specific ethical approval was not necessary
according to an agreement with the local justice department and the ethical standards.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A. Steuwe and J. Boeven are joint first authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Steuwe, A., Boeven, J., Cordes, L. et al. Impact of increasing levels of adaptive statistical iterative reconstruction on image quality in oil-based postmortem CT angiography in coronary arteries. Int J Legal Med 135, 1869–1878 (2021). https://doi.org/10.1007/s00414-021-02530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-021-02530-1