Abstract
Hypoxia is a condition in which proliferating tumor cells are deprived of oxygen due to limited blood supply from abnormal tumor microvasculature. This study aimed to investigate the molecular changes that occur in tumor cell hypoxia with special emphasis placed on the efficacy of chemotherapeutic and radiation-related effects. Four commercially available chemotherapeutic agents: cisplatin, cyclophosphamide, doxorubicin, and 5-fluorouracil, were tested for their cytotoxic activity on the cancer cell lines PC3 (prostate), HepG2 (liver), and MCF-7 (breast). Tumor cell lines under hypoxia were treated with both IC50 concentrations of the different chemotherapeutic agents and irradiated with 5 and 10 Gy using a 137Cs gamma source. Hypoxia-inducible factor-1α (HIF-1α) protein levels were examined using an ELISA assay. Hypoxic cells showed a significant change in cell viability to all chemotherapeutic agents in comparison to normoxic controls. HepG2 cells were more resistant to the cytotoxic drug doxorubicin compared to other cancer cell lines. The flow cytometric analysis showed that hypoxic cells have lower levels of total apoptotic cell populations (early and late apoptosis) compared to normoxic cells suggesting decreased hypoxia-induced apoptosis in cancer cells. The highest reduction in HIF-1α level was observed in the MCF-7 cell line (95.5%) in response to the doxorubicin treatment combined with 10 Gy irradiation of cells. Chemoradiotherapy could result in minimal as well as a high reduction of HIF-1α based on cell type, type of chemotherapy, and amount of ionizing radiation. This study highlights future research work to optimize a combined chemoradiotherapeutic regime in individual cancer cell hypoxia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is a known worldwide threat responsible for about 7.6 million deaths per year, and it is predicted to reach 13.1 million by 2030 (WHO 2017). Factors related to the microenvironment play decisive roles in cancer initiation, progression, metastasis, and chemo-radioresistance. An example of such factors is hypoxia which is considered as one of the potential cancer hallmarks, especially in solid tumors. It occurs due to abnormal vascularization and rapid proliferation of tumors that result in fluctuation of oxygen supply throughout the growing tumor mass (Brahimi-Horn et al. 2007).
Hypoxia is defined as a loss of oxygen in tissues and can occur in tumors due to limited perfusion of blood vessels (acute hypoxia) or because of limited oxygen diffusion and its consumption by tumor cells (chronic hypoxia) that leads to hypoxic regions at distances of approximately 100 to 200 µm from functional blood vessels (Brown and Wilson 2004).
Hypoxia enhances the ability of tumors to metastasize and increases their aggressiveness and resistance to apoptosis (Muz et al. 2015; Wilson and Hay 2011). It impacts significantly on radio-chemo-resistance, resulting in poor prognosis in patients with severe hypoxic neoplastic tumors (Doktorova et al. 2015). During radiotherapy, the interaction between oxygen and radiation results in the production of radical oxygen species (ROS), which cause DNA damage, thereby promoting apoptosis. On the other hand, hypoxic areas in large tumors are less susceptible to radiotherapy because of low levels of ROS (Bindra et al. 2007).
Chemo-resistance in hypoxic tumors is largely a consequence of the failure of anti-proliferative drugs to target cancer cells that have undergone hypoxia-induced reversible quiescence (Mistry et al. 2017). Furthermore, the limitations of diffusion and perfusion cause tumor hypoxia to reduce drug delivery to these regions (Huxham et al. 2004). Since the cytotoxic effect of cytostatic drugs is greater in rapidly dividing cells, the slow proliferating tumor cells far away from blood vessels are less sensitive to chemotherapy (Strese et al. 2013).
Hypoxia selects for cells with low expression of p53, and consequently, p53-induced apoptosis is reduced in hypoxic cells (Graeber et al. 1996). In normoxic surroundings, DNA injuries caused by some anticancer drugs are more permanent, whereas higher rates of restoration occur within hypoxic surroundings (Brown and Wilson 2004). Another correlation between hypoxia and chemotherapy resistance is the up-regulation of multidrug-resistance (MDR) genes and overexpression of the gene product P-glycoprotein (P-gp), known to be involved in multidrug resistance (Wartenberg et al. 2003).
Hypoxia-inducible factor 1 (HIF-1) is the heterodimer protein of two subunits: HIF-1α and HIF-1β transcriptional factor. Each contains helix–loop-(HLS-) PER-ARNT-SIM (HLS PAS) domains that facilitate DNA binding and heterodimerization. The beta subunit can also be referred to as the aryl hydrocarbon receptor nuclear translocator (ARNT). The alpha subunit is sensitive to oxygen, whereas the beta subunit (HIF-1β) is oxygen-dependent (Balamurugan 2016).
HIF-1 can essentially be interpreted as a messenger migrating towards the nucleus to activate transcription responses to hypoxia. HIF-1 has been involved in gene regulation involving metastasis, growth, tumorigenesis, angiogenesis, and invasion. The vascular endothelial growth factor (VEGF) is an example of a HIF-1 target gene in which its expression is induced by hypoxia (Akanji et al. 2019). Erythropoietin, the key regulator of red blood cell production is also one of the many target genes activated by HIF-1 under hypoxia which had helped to decipher HIF-1 activation and cellular oxygen sensing (Locatelli et al. 2017).
Despite the relatively large amount of data regarding tumor hypoxia, there might be some lack of knowledge on how the combined chemoradiotherapy could be effective in reducing the cellular concentrations of HIF-1 alpha especially when attempts are made to compare the conventionally used chemotherapeutic drugs versus specific tumor types.
This study aimed to elucidate the impact of chemoradiotherapy on different cancer cell lines, including prostate, breast, and liver under hypoxic conditions with emphasis placed on radiation dose, different chemotherapeutic agents as well as type of cancer.
Materials and methods
Chemotherapeutic agents
Four commercially available and clinically relevant chemotherapeutic agents, namely cisplatin, cyclophosphamide, doxorubicin, and 5-fluorouracil, were used in the study. All compounds were in liquid form and purchased from a local supplier (El-Ezaby Pharmacy Inc, Egypt) with optimal storing condition of 4 °C.
Cell lines and culture condition
Three human cancer cell lines were used in this study originating from prostate cancer (PC3 ATCC® CRL-1435™), liver cancer (HepG2 ATCC® HB-8065™), and breast cancer (MCF-7 ATCC® HTB-22™). PC3, HepG2, and MCF-7 cells were obtained from laboratory of the Tissue Culture Department of the Holding Company for Biological Products and Vaccines (VACSERA, Dokki, Egypt).
The cells were cultured at 37 °C under 5% carbon dioxide and 95% humidity in complete RPMI-1640 medium supplemented with 10% heat-inactivated fetal bovine serum (FBS), 1% antibiotic–gentamicin solution, and 1% sodium pyruvate. Cells were grown in 75 cm2 cell culture flasks to 80% confluence and harvested, counted, and washed with phosphate-buffered saline (PBS). All media and supplies were purchased from Lonza, Belgium.
Hypoxia induction
Normoxic cells were maintained at 37 °C in a humidified incubator containing 21% O2, 5% CO2 in the air. To induce hypoxia; cell culture plates were placed in an acryl chamber (in-house made) and then flushed with a mixture of 1% O2, 5% CO2, and 94% N2 for 24 h. During hypoxia induction, the chamber was gently inflated leaving a moderate pressure over the plates with proper sealing to avoid any sort of leaking. The temperature was normally kept at 37 °C.
Figure 1 shows the chamber with a plastic cover and two 96-well cell culture plates inserted inside. The black frame around the chamber was tight to prevent any leakage of the gas and maintain constant experimental conditions throughout cell incubation. This model was similar to previous reports that showed an acceptable performance in hypoxia induction (Saxena et al. 2020).
Assessment of cell cytotoxicity by MTT assay
The cell lines PC3, HepG2, and MCF-7 were rinsed with PBS, trypsinized, and re-suspended in complete RPMI-1640 culture medium, then cells were counted using a hemocytometer chamber by Trypan blue exclusion technique (Bellamakondi et al. 2014).
For chemosensitivity studies, the cells were cultured in 96-multiwell plate at a density of 104 cells/well for 24 h before treatment with the chemotherapeutic agent to allow attachment of the cells to the wall of the plate. After 24 h incubation, the medium was removed from each well and replaced with a fresh cell culture medium containing the tested compounds at different concentrations using a two-fold serial dilution method. The experiment was carried out in triplicate wells for each drug for each individual dose.
Cell monolayers were then incubated with different concentrations of chemotherapeutic agents for 48 h at 37 °C incubator supplied with 5% CO2 under normoxic and hypoxic conditions. The drug-containing medium was then removed, and the cells were washed twice with PBS. A volume of 50 µl of yellow methyl thiazolyl tetrazolium salt MTT 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (0.5 mg/ml) was immediately added to each well, and the plates were incubated for 4 h at 37 °C under normoxic and hypoxic conditions. Then the medium was removed, and 50 µl dimethyl sulfoxide (DMSO) was added to dissolve the formazan crystals.
The absorbance of the resulting color was measured using an ELISA plate reader (Boster Immunoleader, USA) at 490 nm to estimate the percentage of viable cells. Cell survival was determined as the true absorbance of the treated wells divided by the controls and expressed as a percentage. The correlation between cell viability and drug concentration was plotted to get the viability curve of each cancer cell line versus a particular drug and to determine the drug concentration that inhibits cell growth by 50% (half-maximal inhibitory concentration; IC50). The dose–response curve was fitted using the non-linear Boltzmann formula, Y = A2 + (A1−A2)/1 + e(x−x°)/dx where A1 is the initial value, A2 is the final value, x0 is the center, and dx is the time constant, so that standard analytical derivation of IC50 can be computed.
The effect of hypoxia on the activity of drugs was expressed as the hypoxia/normoxia ratio (HNR), which is defined as the ratio of IC50 values under hypoxic to normoxic conditions.
Detection of apoptosis by flow cytometry
The IC50 concentration of the four tested chemotherapeutic agents determined by the MTT assay was used to treat the three different cancer cell lines at a density of 1 × 106 cells per 25 cm2 culture flasks for 24 h under normoxic and hypoxic conditions. Then, cells were trypsinized and collected by centrifugation (2000 rpm for 10 min) and removal of supernatant. The remaining cells were washed with ice-cold PBS buffer. After centrifugation for 5 min at 500g at 4 °C, the supernatant was discarded, and cell pellets were re-suspended in 100 μl of binding buffer containing 1 μl Annexin V-FITC and 5 μl propidium iodide (PI) staining solution at room temperature in the dark for 15 min.
Finally, 400 μl of binding buffer was added before analysis on COULTER® EPICS® XL™ flow cytometer (Beckman Coulter Co., France). Analysis of data was performed using WinMDI software (version 2.8).
In vitro treatment and irradiation of cancer cell lines
The three cancer cell lines were first grown for 24 h in 25 cm2 culture flasks at a cell density of 1 × 106 under hypoxia, then treated with both the IC50 concentration (obtained from cytotoxicity MTT test) of the tested chemotherapeutic agents, then irradiated with gamma ray doses of 5 and 10 Gy using a 137Cs unit station (0.41 Gy/min, dose rate) (Gamma-cell 40, Canada) under hypoxic and normoxic conditions.
After 24 h of recovery, cells at a density of approximately 2 × 106 were lysed on ice with 200 µl of cold lysis buffer that consists of 20 mM Tris–HCl pH 7.4 containing 137 mM NaCl2, 2 mM EDTA, and a 1% Triton X-100. Lysates were transferred to Eppendorf tubes, incubated for 15 min at 4 °C, and centrifuged for 30 min at 4500 rpm at 4 °C. The supernatant was collected and rapidly frozen and stored at − 20 °C for future detection of HIF-1α protein concentration using ELISA.
Measurement of HIF-1α level using enzyme-linked immunosorbent assay (ELISA)
HIF-1α protein levels were examined as a marker of hypoxia and measured using a commercial human HIF-1α ELISA Kit-96 T (Wuhan Fine Biotech Co., China), according to the manufacturers’ instructions. Figure 2 shows the standard curve of the HIF-1α protein.
In the three above major steps including cell toxicity assay, flow cytometry as well as gamma irradiation, the comparison was performed taking the cells grown in normoxia conditions as reference keeping all experimental conditions as similar as possible. This has been widely used in the literature especially in experimental work looking at the effect of oxygen insufficiency on tumor cells while rendering normoxia as control (Bowyer et al. 2017; Dubbelboer et al. 2019; Saggar and Tannock 2015).
Results
Cell viability assessment
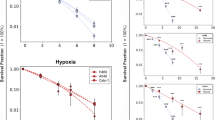
The drug sensitivity as assessed by the MTT assay under normoxic (20% O2) and hypoxic (1% O2) conditions showed that the relative effect of hypoxia on the IC50 was cell line-dependent.
In all chemotherapeutic agents used on PC3 cells, the IC50 was higher when cells were under hypoxic conditions than normal conditions, as shown in Fig. 3 and Table 1. The graphs show the mean absorbance expressed as % of the untreated controls against log concentration of cisplatin, cyclophosphamide, doxorubicin, or 5-fluorouracil. The sigmoid pattern response of cell chemosensitivity was apparent in all drugs used with PC3 cells.
The hypoxia/normoxia ratio (HNR) obtained for PC3 cells is presented graphically in Fig. 4. A similar pattern of response was observed in all chemotherapeutic agents such that the HNR was always greater than one (i.e., HNR > 1). A closer look into Fig. 4 indicated that the HNR was highest in cisplatin, followed by 5-fluorouracil, cyclophosphamide, and doxorubicin, respectively.
Similar to PC3 cells, the IC50 was higher in all drugs used with HepG2 cells when the cells were under hypoxic conditions compared with normoxia, Fig. 5 and Table 1.
As shown in Fig. 4, the HNR was decreased in the order doxorubicin > cisplatin > 5-fluorouracil > cyclophosphamide. The highest HNR of HepG2 cells was about 11-fold when using doxorubicin, while the lowest HNR was obtained when treating with cyclophosphamide at almost slight increase of drug concentration (1.3-fold).
Similar to PC3 and HepG2 cells, all chemotherapeutic agents used with MCF-7 cells revealed that the IC50 was higher when cells were under hypoxic in comparison to normoxic conditions, as shown in Fig. 6 and Table 1. In contrast to the previous two cell lines, the HNR was increasingly higher in this order 5-fluorouracil > cisplatin > doxorubicin > cyclophosphamide, Fig. 4. Moreover, the highest HNR of MCF-7 cells was around threefold when cells were treated with 5-fluorouracil, whereas it was minimum around onefold as shown with cyclophosphamide.
Flow cytometric data analysis
Flow cytometry was used to verify the results obtained from the colorimetric MTT assay to ensure the induction of cellular apoptosis. In all cancer cell lines, the flow cytometric results confirmed that all chemotherapeutic agents were variably less effective in hypoxia than normoxia. The majority of results obtained were in the direction of reduced cell apoptosis in hypoxia than normoxia when the cancer cells were treated with the different chemotherapeutic compounds. Figures 7, 8 and 9 describe the data of the flow cytometry of investigated cancer cell lines versus the four chemotherapeutic agents. Tables 2, 3 and 4 summarize the results of total apoptotic cell populations (i.e., Q2 + Q4) as a new index to describe in part the clinical environment where hypoxic and normoxic cells are often in close neighboring relationships.
Annexin V-FITC/PI analysis showed that the chemotherapeutic agents had induced variable cell populations at early and late apoptosis in PC3 cells, Fig. 7. Under hypoxic conditions, the induction of both early and late apoptosis was the highest when the PC3 cells were treated with doxorubicin while being the lowest with cyclophosphamide treatment, Table 2.
Annexin V-FITC/PI analysis revealed that chemotherapeutic agents also induced early and late apoptosis of variable cell populations in HepG2 cells, Fig. 8. Similar to the findings of PC3, the induction of both early and late apoptosis was relatively higher in all treatments administered to HepG2 cells when cells were in hypoxic conditions using doxorubicin while being lower with cyclophosphamide, Table 3.
The analysis of Annexin V-FITC/PI showed that the different chemotherapeutic agents had induced early and late apoptosis of variable cell populations in MCF-7 cells, Fig. 9. In all treatments applied to MCF-7 cells, the induction of both early and late apoptosis was relatively higher when cells were under hypoxic conditions using doxorubicin, while 5-fluorouracil was the lowest, Table 4.
Quantification of HIF-1α levels using ELISA
The combined chemoradiotherapy in case of PC3 cancer cell line treated with all chemotherapeutic agents showed a reduction of HIF-1α level when the radiation dose has been doubled (i.e., from 5 to 10 Gy), Table 5 summarizes the percent reduction performed of HIF due to cell treatment with combined chemoradiotherapy for all cell lines under 5 and 10 Gy gamma exposure The maximum reduction of HIF-1α level (with respect to hypoxic cells not irradiated) was obtained after treatment of PC3 cells with doxorubicin in addition to radiation doses of 5 and 10 Gy while cyclophosphamide achieved minimal effect in reducing the HIF-1α level in the presence of gamma irradiation, Table 5.
HepG2 cancer cell line treated with all chemotherapeutic agents showed a reduction in the level of HIF-1α when the radiation dose was doubled (i.e., from 5 to 10 Gy). The greatest reduction of the HIF-1α level was achieved with doxorubicin in 10 Gy radiation dose, whereas cyclophosphamide had minimal effect in reducing the HIF-1α level with the radiation doses of 5 and 10 Gy.
In case of MCF-7 cancer cell line treated with all chemotherapeutic agents, the combined chemoradiotherapy also showed a reduction of HIF-1α level when the radiation dose has been doubled (i.e., from 5 to 10 Gy). The maximum reduction of HIF-1α level was observed with doxorubicin in both 5 and 10 Gy radiation doses, whereas 5-fluorouracil achieved minimal effect in reducing the HIF-1α level with 5 Gy radiation dose.
Discussion
Hypoxic tumors remain one of the challenges for chemotherapy and radiotherapy treatment regimes. This is in great part due to the fact that hypoxia creates a state of treatment resistance that potentially reduces drug efficacy and treatment success (McKenna et al. 2018). Our approach was to characterize the response of different cancer cell lines using different chemotherapeutic agents and then evaluate the impact of combined chemoradiotherapy on the levels of HIF-1α on the same cells under hypoxia taking the normoxic conditions as reference.
Several studies have shown that tumor cells are capable of developing adaptive resistance under stress conditions such as hypoxia which interferes with the mechanisms of action for most cancer chemotherapeutic drugs (Davou et al. 2019) leaving the normal cells more vulnerable to the cytotoxic effects of these drugs.
The oxygen concentration in human tumors widely varies and the level of hypoxia seems to be tumor stage- and size-independent. Radiotherapy and conventional chemotherapies are often less effective in oxygen-depressed cells. Therefore, it is of great importance to make use of oxygen deficiency and find drugs that are more effective in hypoxic tumor cells (Strese et al. 2013).
MTT assay was used to evaluate the anticancer effects of different chemotherapeutic agents on PC3, HepG2, and MCF-7 cancer cells. Exposure of cancer cell lines to 24 h treatment of chemotherapeutic agents might not be long enough to see a reduction in cell viability using the MTT assay, and therefore, a later time point of 48 h could also be investigated (Yu et al. 2015). However, an early recording of the drug potency might indicate its effectiveness since a longer time might equalize the effect of different agents.
In all cancer cell lines, exposure to cytotoxic agents under hypoxic conditions led to significant resistance to all chemotherapeutic agents represented by an increased drug concentration (higher IC50) compared to those under normoxic conditions.
Results showed also that when PC3 prostate cancer cells were exposed to hypoxic conditions, they developed resistance to cytotoxic drug cisplatin (i.e. HNR = 5.48) and lower resistance to cytotoxic drug doxorubicin (i.e. HNR = 1.63), whereas hypoxic HepG2 liver cancer cells had more resistance to doxorubicin (i.e. HNR = 10.51) but remarkably lower resistance to drug cyclophosphamide (i.e. HNR = 1.31). MCF-7 breast cancer cells had greater resistance to cytotoxic drug 5-fluorouracil (i.e. HNR = 2.77) and lower resistance to cytotoxic drug cyclophosphamide (i.e. HNR = 1.42).
This signifies that the response of cells to chemotherapeutic agents under normoxic and hypoxic conditions is variable, depending on the cell line and type of chemotherapy. Similar findings were reported with HepG2 when treated with doxorubicin showing more resistance in hypoxia than normoxia after 24 h incubation (Bowyer et al. 2017). On the other hand, chemotherapeutic drugs such as doxorubicin upregulate HIF-1α (Cao et al. 2013) providing a feedback loop amplifying drug resistance responses in tumors. Cisplatin chemo-resistance has been an intriguing issue during hypoxia, and this observation has also been made in the current study as the cisplatin H/N ratio was among the highest across the four drugs in PC3 and comparable with 5-fluorouracil in MCF7 and second after doxorubicin in HepG2 cell lines. Moreover, HepG2 and other liver cell lines showed better response in treatment with cisplatin in normoxia despite the improved cell viability under hypoxia conditions (Chi et al. 2009).
The observed tolerance to doxorubicin was significantly different between the cell lines being higher with HepG2 cells, whereas lowest tolerance with MCF-7 cells. This has been reported not only in different cancers, but also in cell lines of the same type of cancer, for example, liver carcinoma (Dubbelboer et al. 2019). It was shown that hypoxia could interfere with chemotherapeutic treatment and resistance of doxorubicin producing different profiles of protein expression for human-derived liver cancer cells (Dubbelboer et al. 2019).
Highly but variable significant resistance to cisplatin, cyclophosphamide, doxorubicin, and 5-fluorouracil in hypoxia was observed in all the three cancer cell lines, consistent with previous data showing hypoxia-induced resistance to cisplatin and doxorubicin among others in a variety of different tumor types (Adamski et al. 2013).
In all cancer cell lines exposed to various chemotherapeutic agents under hypoxia, apoptosis was generally reduced as displayed by flow cytometry results. However, this reduction was variable being very low in PC3 cells treated with cyclophosphamide and MCF7 treated with cisplatin and doxorubicin. The highest reduction was noted in MCF-7 cells when treated with 5-fluorouracil and in PC3 cells when treated with cisplatin and 5-fluorouracil. This finding confirms the complex nature of hypoxia and its relative impact on different cell lines consistent with previous reports (Blancher et al. 2000; Dubbelboer et al. 2019; Strese et al. 2013).
The difference in the viability of cells after treatment with chemotherapeutic agents is reflected in their differential expression of the apoptotic marker Annexin V.
Inspecting the flow cytometry results, hypoxic cells showed lower levels of total apoptotic cell populations (i.e., Q2 + Q4) after 24 h of treatment with different chemotherapeutic agents compared to substantially higher levels of total populations of an apoptotic cell under normoxia, certainly, the hypoxia cells still have great resistance to chemotherapy compared to normoxic cells. The doxorubicin drug was obviously a more potent treatment for all cancer cell lines studied under hypoxia.
The combined chemoradiotherapy treatment modalities were administered to prevent treatment resistance due to the higher expression of HIF-1α under hypoxia compared to normoxic conditions. It was reported that in prostate patients who were treated with radiotherapy or radical prostatectomy had a reduced time to disease progression in association with increased HIF-1α levels (Vergis et al. 2008). In patients with hepatocellular carcinoma, the increased HIF-1α was associated with lymph node invasion and patient mortality (Xie et al. 2008).
The ELISA test in the present study allowed for in vitro quantitation of the HIF-1α protein. A multitude of findings showed that as a key regulator of hypoxia adaptive response, the expression level of HIF-1α was closely associated with the type of the cell line, chemotherapeutic agent, as well as a level of gamma irradiation. Under hypoxic conditions, suppression of HIF-1α expression can lead to changes in tumor cell proliferation, invasion, metastasis, and apoptosis. Thus, HIF-1α has gradually become a potential target in the treatment of cancer (Chen et al. 2018).
HIF-1α is a protein that is highly dependent on oxygen content. The presence or absence of oxygen also controls the levels of this protein. In normoxia conditions where there is a sufficient amount of oxygen, HIF-1α is degraded by the complex proteasome, whereas in hypoxic conditions, HIF-1α undergoes stabilization by forming a heterodimer with HIF-1β and then translocates to the nucleus and binds to the gene promoter hypoxia response element (HRE) target (Herawati et al. 2017).
Doxorubicin is one of the most effective antitumor drugs against solid tumors, including breast cancer, but the clinical usage has been limited due to its low bioavailability and severe side effects, such as cardiotoxicity (Gomari et al. 2019). It has many mechanisms of action involving intercalation within DNA base pairs resulting in DNA strand breaks and inhibition of both DNA and RNA synthesis, generating the formation of reactive oxygen species (ROS) and oxidative stress (Korga et al. 2019). Doxorubicin might also serve to inhibit the binding of HIF-1 to the promoter region of genes that respond to low oxygen levels (Lee et al. 2009).
A mechanism by which ionizing radiation exerts its therapeutic effects is by inducing single- and double-strand DNA breaks and ROS. The formation of ROS is dependent on the availability of oxygen. Further, oxygen radiosensitizes cells by stabilizing DNA lesions (Huerta et al. 2009). Radiolysis of water provides the reactive free radicals that damage the DNA (Huerta et al. 2009). Thus, hypoxic tissue responds poorly to ionizing radiation treatment.
It is important to note that HIF-1α activity varies between different cancer cell lines under the same level of hypoxia (Dubbelboer et al. 2019). The amount of HIF-1α protein detected with the ELISA in all cancer cell lines in the control normoxia was relatively low compared to hypoxic conditions. A general but expected observation was that the effect of 10 Gy irradiation was relatively higher in reducing the level of HIF-1α concentration in comparison to 5 Gy in all cell lines using the different chemotherapeutic agents. However, this reduction was not consistent in all the cell lines.
The combined chemoradiotherapy approach taken in this study showed that doxorubicin and cisplatin when combined with 5 Gy gamma irradiation produced the maximal effect in comparison to other drugs in reducing HIF-1α. However, increasing the dose to 10 Gy was not associated with a greater increase in reducing HIF-1α levels except 5-fluorouracil where the reduction was threefold. In HepG2 cells, the drugs doxorubicin, 5-fluorouracil, and cisplatin were the most effective in reducing HIF-1α, and again, increasing the dose was not associated with a large increase in reducing HIF-1α levels. In MCF-7 cells, the doxorubicin, cisplatin, and cyclophosphamide were the highest in reducing HIF-1α levels. However, increasing the radiation dose to 10 Gy was only effective in combination with 5-fluorouracil in significantly lowering HIF-1α levels.
These findings demonstrate the necessity to individually optimize radiation dose with chemotherapeutic agents used in particular cancer cells. They also support notion of precision oncology that aims to tailor a given treatment for every individual patient to reach maximal response. Because the chemotherapy drugs can be used in neoadjuvant or adjuvant treatment either with or without radiation therapy, it is interesting to look for drugs that can reduce the HIF at low radiation doses especially in neoadjuvant chemo-radiotherapy. Such drugs could also have desired consequences in reducing side effects of preoperative regimes (Chen et al. 2019; Matuschek et al. 2020).
Chemoradiotherapy can be used to significantly reduce tumor size and shape as well as reduce tumor recurrence. It can also significantly improve overall survival, progression-free survival in comparison to radiation therapy alone in patients with un-resectable stage III non-small cell lung cancer (Hung et al. 2019). The best combination in preoperative phase should employ lower radiation dose and less toxicity with an increase in tumor resection rate and reduced side effects. Therefore, drugs that enhance tumor radiosensitivity and reduce the hypoxic burden would be highly advantageous. This study has focused on elucidating an important aspect which is the reduction of HIF-1α, emphasizing its utility as a concomitant and prognostic biomarker during chemoradiotherapy (Li et al. 2016). Such effect has been revealed in a meta-analysis on head and neck cancer patients who were treated with radiotherapy or chemoradiotherapy, where the hypoxic fraction was found to be independently associated with patients survival (Nordsmark et al. 2005). While the current study has the limitation of being in vitro, we highly recommend dedicated clinical research to further investigate the combinations of chemoradiotherapy and different dosing schemes so that a better clinical inference can be achieved.
This study highlights future research work to understand individual cellular response variation to combined chemoradiotherapy with more focus on cell apoptosis in association with cellular levels of HIF-1α.
Conclusion
Cancer cells under hypoxia have a diverse response against chemotherapeutic agents. While doxorubicin has its well-known cytotoxic effects, it showed promising results in reducing cell survival and capabilities of initiating cell apoptosis in cell hypoxia. The hypoxic PC3 cells have greater resistance to cytotoxic drug cisplatin. HepG2 cells have further resistance to cytotoxic drug doxorubicin while MCF-7 cells have greater resistance to cytotoxic drug 5-fluorouracil verifying that the response of cells to chemotherapeutic agents under normoxic and hypoxic conditions varied depending on the cell type. Furthermore, chemoradiotherapy could result in minimal as well as a high reduction of HIF-1α level based on cell type, type of chemotherapy, and amount of ionizing radiation. This study underlines future research work to optimize chemoradiotherapy regime in individual cancer cell hypoxia.
References
Adamski J, Price A, Dive C, Makin G (2013) Hypoxia-induced cytotoxic drug resistance in osteosarcoma is independent of HIF-1alpha. PLoS ONE 8:1–16. https://doi.org/10.1371/journal.pone.0065304
Akanji MA, Rotimi D, Adeyemi OS (2019) Hypoxia-inducible factors as an alternative source of treatment strategy for cancer. Oxid Med Cell Longev. https://doi.org/10.1155/2019/8547846
Balamurugan K (2016) HIF-1 at the crossroads of hypoxia, inflammation, and cancer. Int J Cancer 138:1058–1066. https://doi.org/10.1002/ijc.29519
Bellamakondi PK, Godavarthi A, Ibrahim M, Kulkarni S, Ramachandra Naik M, Sunitha M (2014) In vitro cytotoxicity of Caralluma species by MTT and Trypan Blue dye exclusion. Asian J Pharm Clin Res 7:17–19
Bindra RS, Crosby ME, Glazer PM (2007) Regulation of DNA repair in hypoxic cancer cells. Cancer Metastasis Rev 26:249–260. https://doi.org/10.1007/s10555-007-9061-3
Blancher C, Moore JW, Talks KL, Houlbrook S, Harris AL (2000) Relationship of hypoxia-inducible factor (HIF)-1α and HIF-2α expression to vascular endothelial growth factor induction and hypoxia survival in human breast cancer cell lines. Cancer Res 60:7106–7113
Bowyer C, Lewis AL, Lloyd AW, Phillips GJ, Macfarlane WM (2017) Hypoxia as a target for drug combination therapy of liver cancer. Anticancer Drugs 28(7):771–780. https://doi.org/10.1097/CAD.0000000000000516
Brahimi-Horn MC, Chiche J, Pouyssegur J (2007) Hypoxia and cancer. J Mol Med 85:1301–1307
Brown JM, Wilson WR (2004) Exploiting tumour hypoxia in cancer treatment. Nat Rev Cancer 4:437–447. https://doi.org/10.1038/nrc1367
Cao Y, Eble JM, Moon E, Yuan H, Weitzel DH, Landon CD, Nien CYC, Hanna G, Rich JN, Provenzale JM, Dewhirst MW (2013) Tumor cells upregulate normoxic HIF-1a in response to doxorubicin. Cancer Res 73:6230–6242. https://doi.org/10.1158/0008-5472.CAN-12-1345
Chen J-Y, Zhang Y-G, Du J-D (2018) HIF-1α restricts proliferation and apoptosis of Tca8113 cells through up regulation of Hippo signaling pathway under hypoxic conditions. Eur Rev Med Pharmacol Sci 22:6832–6837
Chen M, Chen LZ, Xu L, Zhang JS, Song X (2019) Neoadjuvant chemoradiation for locally advanced rectal cancer: a systematic review of the literature with network meta-analysis. Cancer Manag Res 11:741–758. https://doi.org/10.2147/CMAR.S189445
Chi KL, Zhen FY, Ho DW, Ng MN, Yeoh GCT, Poon RTP, Sheung TF (2009) An Akt/hypoxia-inducible factor-1α/platelet-derived growth factor-BB autocrine loop mediates hypoxia-induced chemoresistance in liver cancer cells and tumorigenic hepatic progenitor cells. Clin Cancer Res 15:3462–3471. https://doi.org/10.1158/1078-0432.CCR-08-2127
Davou G, Chuwang N, Essien U, Choji T, Echeonwu B, Lugos M (2019) Cytotoxicity analysis of etoposide and cisplatin on cell lines from human lung cancer and normal human lung. Int Res J Med Med Sci 7:40–47
Doktorova H, Hrabeta J, Khalil MA, Eckschlager T (2015) Hypoxia-induced chemoresistance in cancer cells: the role of not only HIF-1. Biomed Pap 159:166–177. https://doi.org/10.5507/bp.2015.025
Dubbelboer IR, Pavlovic N, Heindryckx F, Sjögren E, Lennernäs H (2019) Liver cancer cell lines treated with doxorubicin under normoxia and hypoxia: cell viability and oncologic protein profile. Cancers (Basel) 11:1024. https://doi.org/10.3390/cancers11071024
Gomari H, Moghadam MF, Soleimani M, Ghavami M, Khodashenas S (2019) Targeted delivery of doxorubicin to HER2 positive tumor models. Int J Nanomed 14:5679–5690. https://doi.org/10.2147/IJN.S210731
Graeber TG, Osmanian C, Jacks T, Housman DE, Koch CJ, Lowe SW, Giaccia AJ (1996) Hypoxia-mediated selection of cells with diminished apoptotic potential in solid tumours. Nature 379:88–91. https://doi.org/10.1038/379088a0
Herawati M, Mulyawan WW, Farhan FS, Ferdinal F, Jusman SWA, Sadikin M (2017) Expression of hypoxia-inducible factor-1α and myoglobin in rat heart as adaptive response to intermittent hypobaric hypoxia exposure. HAYATI J Biosci 24:131–135. https://doi.org/10.1016/j.hjb.2017.08.010
Huerta S, Gao X, Saha D (2009) Mechanisms of resistance to ionizing radiation in rectal cancer. Expert Rev Mol Diagn 9(5):469–480. https://doi.org/10.1586/erm.09.26
Hung MS, Wu YF, Chen YC (2019) Efficacy of chemoradiotherapy versus radiation alone in patients with inoperable locally advanced non-small-cell lung cancer: a meta-analysis and systematic review. Medicine (baltimore) 98(27):e16167
Huxham LA, Kyle AH, Baker JHE, Nykilchuk LK, Minchinton AI (2004) Microregional effects of gemcitabine in HCT-116 xenografts. Cancer Res 64:6537–6541. https://doi.org/10.1158/0008-5472.CAN-04-0986
Korga A, Ostrowska M, Iwan M, Herbet M, Dudka J (2019) Inhibition of glycolysis disrupts cellular antioxidant defense and sensitizes HepG2 cells to doxorubicin treatment. FEBS Open Bio 9:959–972. https://doi.org/10.1002/2211-5463.12628
Lee KA, Qian DZ, Rey S, Wei H, Liu JO, Semenza GL (2009) Anthracycline chemotherapy inhibits HIF-1 transcriptional activity and tumor-induced mobilization of circulating angiogenic cells. Proc Natl Acad Sci U S A 106:2353–2358. https://doi.org/10.1073/pnas.0812801106
Li Y, Wang J, Ma X, Li T, Yan Y, Xue C, Hui B, Liu R, Ma H, Ren J (2016) A review of neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Int J Biol Sci 12:1022–1031. https://doi.org/10.7150/ijbs.15438
Locatelli F, Fishbane S, Block GA, MacDougall IC (2017) Targeting hypoxia-inducible factors for the treatment of anemia in chronic kidney disease patients. Am J Nephrol 45:187–199. https://doi.org/10.1159/000455166
Matuschek C, Nestle-Kraemling C, Kühn T, Fehm T, Bölke E, Corradini S, Fastner G, Maas K, Seidel C, Budach W (2020) Neoadjuvant radio (chemo)therapy for breast cancer: an old concept revisited. Breast Care 15:112–117. https://doi.org/10.1159/000507041
McKenna DJ, Errington R, Pors K (2018) Current challenges and opportunities in treating hypoxic prostate tumors. J Cancer Metastasis Treat. 4:1–13
Mistry IN, Thomas M, Calder EDD, Conway SJ, Hammond EM (2017) Clinical advances of hypoxia-activated prodrugs in combination with radiation therapy. Int J Radiat Oncol Biol Phys 98:1183–1196. https://doi.org/10.1016/j.ijrobp.2017.03.024
Muz B, Puente P, Azab F, Azab AK (2015) The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia 3:83–92. https://doi.org/10.2147/hp.s93413
Nordsmark M, Bentzen SM, Rudat V, Brizel D, Lartigau E, Stadler P, Becker A, Adam M, Molls M, Dunst J, Terris DJ, Overgaard J (2005) Prognostic value of tumor oxygenation in 397 head and neck tumors after primary radiation therapy. An International Multi-Center Study. Radiother Oncol 77:18–24. https://doi.org/10.1016/j.radonc.2005.06.038
Saggar JK, Tannock IF (2015) Chemotherapy rescues hypoxic tumor cells and induces their reoxygenation and repopulation - an effect that is inhibited by the hypoxia-activated prodrug TH-302. Clin Cancer Res 21:2107–2114. https://doi.org/10.1158/1078-0432.CCR-14-2298
Saxena S, Agrawal I, Singh P, Jha S (2020) Portable, low-cost hypoxia chamber for simulating hypoxic environments: development, characterization and applications. Med Devices Sensors 3:1–8. https://doi.org/10.1002/mds3.10064
Strese S, Fryknäs M, Larsson R, Gullbo J (2013) Effects of hypoxia on human cancer cell line chemosensitivity. BMC Cancer. https://doi.org/10.1186/1471-2407-13-331
Vergis R, Corbishley CM, Norman AR, Bartlett J, Jhavar S, Borre M, Heeboll S, Horwich A, Huddart R, Khoo V, Eeles R, Cooper C, Sydes M, Dearnaley D, Parker C (2008) Intrinsic markers of tumour hypoxia and angiogenesis in localised prostate cancer and outcome of radical treatment: a retrospective analysis of two randomised radiotherapy trials and one surgical cohort study. Lancet Oncol 9:342–351. https://doi.org/10.1016/S1470-2045(08)70076-7
Wartenberg M, Ling FC, Müschen M, Klein F, Acker H, Gassmann M, Petrat K, Pütz V, Hescheler J, Sauer H (2003) Regulation of the multidrug resistance transporter P-glycoprotein in multicellular tumor spheroids by hypoxia- inducible factor-1 and reactive oxygen species. FASEB J 17:1–22. https://doi.org/10.1002/ijc.20596
World Health Organization. Fact sheet no 297. 2017. http://www.who.int/mediacentre/factsheets/fs297/en/index.html. Accessed 19 Jun 2017
Wilson WR, Hay MP (2011) Targeting hypoxia in cancer therapy. Nat Rev Cancer 11:393–410. https://doi.org/10.1038/nrc3064
Xie H, Song J, Liu K, Ji H, Shen H, Hu S, Yang G, Du Y, Zou X, Jin H, Yan L, Liu J, Fan D (2008) The expression of hypoxia-inducible factor-1α in hepatitis B virus-related hepatocellular carcinoma: Correlation with patients’ prognosis and hepatitis B virus X protein. Dig Dis Sci 53:3225–3233. https://doi.org/10.1007/s10620-008-0296-9
Yu G, Chen X, Chen S, Ye W, Hou K, Liang M (2015) Arsenic trioxide reduces chemo-resistance to 5-fluorouracil and cisplatin in HBx-HepG2 cells via complex mechanisms. Cancer Cell Int 15:1–12. https://doi.org/10.1186/s12935-015-0269-y
Acknowledgements
This project was supported financially by the Academy of Scientific Research and Technology (ASRT), Egypt, Grant No. 6679), (ASRT) is the 2nd affiliation of this research.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors disclose that they do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ibrahim, A.M., Nady, S., Shafaa, M.W. et al. Radiation and chemotherapy variable response induced by tumor cell hypoxia: impact of radiation dose, anticancer drug, and type of cancer. Radiat Environ Biophys 61, 263–277 (2022). https://doi.org/10.1007/s00411-022-00974-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-022-00974-6