Abstract
Purpose
Ventilator weaning protocols rely in part on objective indices to best predict extubation failure in the critically ill. We investigated static respiratory system compliance (RC) as a predictor of extubation failure, in comparison to extubation readiness using rapid shallow breathing index (RSBI).
Material and Methods
This was a cross-sectional, multi-institutional study of mechanically ventilated patients admitted between 12/01/2017 and 12/01/2019. All patients older than 18 years with a documented spontaneous breathing trial and extubation trial were included. RC and RSBI were calculated prior to the extubation trial. The primary outcome was extubation failure—defined as need for reintubation within 72 h from time of extubation.
Results
Of the 2263 patients, 55.8% were males with a mean age of 68 years. The population consisted mostly of Caucasians (73%) and African Americans (20.4%). 274 (12.1%) patients required reintubation within 72 h. On multivariate logistic regression after adjusting for age, sex, body mass index (BMI), admission Sequential Organ Failure Assessment (SOFA) score, number of ventilator days, and the P/F ratio on the day of extubation, RC remained the strongest predictor for extubation failure at 24 h (aOR 1.45; 95% CI 1.00–2.10) and 72 h (aOR 1.58; 95% CI 1.15–2.17). There was no significant association between RSBI and extubation failure at 24 (aOR 1.00; 95% CI 0.99–1.01) or at 72 h (aOR 1.00; 95% CI 0.99–1.01).
Conclusion
RC measured on the day of extubation is a promising physiological discriminant to potentially risk stratify patients with acute respiratory failure for extubation readiness. We recommend further validation studies in prospective cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Protocolized ventilator weaning trials attempt to identify readiness and likelihood of successful extubation. When compared to non-protocolized weaning practice, these trials significantly reduce total duration of ventilation, weaning duration, and intensive care unit length of stay [1,2,3]. Extubation failure or need for reintubation within 48 to 72 h after extubation is independently associated with increased mortality [2, 4, 5]. Failure of the SBT, whether through a T-tube or a low-level pressure support (< 8 cmH2O), relies on objective and subjective weaning parameters [6]. Such parameters include tachypnea, hypertension, cardiac arrhythmia, diaphoresis, and agitation, which are only quantified in part by the rapid shallow breathing index (RSBI) or the ratio of respiratory frequency to tidal volume (f/VT) [5, 7]. A RSBI value greater than 105 breaths/min/L was associated with weaning failure, while an RSBI less than 105 breaths/min/L predicted weaning success [5]. Despite these weaning predictors, extubation failure rates are still relatively high between 10 and 20% [2, 3, 8]. Further, there are insufficient data on the characteristics of patients who pass SBT with RSBI < 105 breaths/min/L, but require reintubation within 72-h.
Static respiratory system compliance (RC) relies on the elastic properties of the respiratory system. Normal static compliance in healthy adults is reported as 80–100 mL/cm H2O, whereas in acute respiratory distress syndrome, static compliance is notably reduced at 29–42 mL/cm H2O [9, 10]. A reduction in static compliance has also been demonstrated in other critically ill patients with pulmonary edema, pneumonia, pulmonary fibrosis, neuromuscular diseases, obesity, and abdominal distension [6]. Current weaning strategies remain insensitive to worsening respiratory load, particularly in critically older patients, owing to loss of respiratory muscle strength, elastic recoil, and exchange surface area [11]. We hypothesize that a decreased RC to a level less than 50 mL/cm H2O is associated with an increased risk of reintubation within 72-h of extubation. In this study, we investigated the role of RC as a predictor of extubation failure and compared its predictive value to that of the RSBI after controlling for other clinically relevant patient factors.
Methods
Study Design
We conducted a retrospective analysis of all adult (age ≥ 18 years of age) mechanically ventilated patients admitted between December 1, 2017 and December 1, 2019 in a large academic health system composed of eight hospitals in Michigan. This study was reviewed and approved by the Institutional Review Board (IRB # 2020-048).
Patient demographics, comorbid diagnoses, admission and discharge diagnoses, ventilator data, and laboratory data were extracted from electronic medical records. RC was calculated from the following equation after completion of daily weaning trial:
where VT represents the tidal volume (mL), PPlateau is the pressure measured from the onset of end-inspiratory occlusion (cmH2O) and PEEP (positive end-expiratory pressure) (cmH2O)) [9].
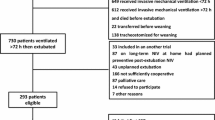
Those patients who underwent a change in code status to no reintubation after extubation or those, who were compassionately extubated or in those, who had a second intubation within the same hospital stay or were extubated without a documented spontaneous breathing trial were excluded from the analysis (Fig. 1). Patients with incomplete datasets were also excluded from the analysis.
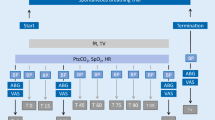
A 30- to 60-min SBT was performed by the respiratory therapist based on institutional protocol for weaning on all ventilated patients. During the SBT, a continuous positive airway pressure (CPAP) of 0 to 5 cm H2O, FiO2 ≤ 40%, and pressure support ventilation (PSV) of 4–5 cm H2O were provided. The SBT was terminated if any of the following was observed: sustained oxygen saturation < 90%, change in blood pressure > 20% from baseline, heart rate > 120 or < 50 beats per minute or 20% change from baseline, respiratory rate > 30 breaths per minute, apnea > 30 s, and signs of increased work of breathing (accessory muscle use, paradoxical respiratory pattern, or change in Richmond Agitation Sedation Scale). SBT was successful if the patient obtained a negative inspiratory force ≥ 20 cm H2O, vital capacity ≥ 10 mL/kg, and RSBI < 100. At completion of the trial, patients were returned to their prior ventilator settings. RC, and ratio of arterial oxygen partial pressure to fractional inspiratory oxygen (P/F ratio) was obtained from the last ventilator measurement.
Outcomes and Statistical Analysis
The main outcome was extubation failure (reintubation) occurring within 72 h of the first extubation attempt compared between patients with a lower (< 50 mL/cm H2O) or higher (≥ 50 mL/H2O) calculated RC on the day of extubation. We elected to transform RC into a dichotomous variable to allow for bedside application. A multivariate logistic regression model including RC as a binary variable was used to assess the impact of patient factors on extubation failure. Candidate variables were preliminarily identified as potentially significant in univariate logistic regression models. Additionally, the predictive value of RC for extubation failure was compared to that of the RSBI employed as a continuous variable using alternative multivariate logistic regression models.
Statistical analysis was performed using JMP version 16 (SAS Institute, Cary, North Carolina). Categorical variables are described as frequency (percentage). Normal or approximately normal variables are reported using the mean (± standard deviation), whereas skewed variables are reported with the median (interquartile range [IQR]). Categorical variables were compared using the Chi-square test or Fisher exact test. Normal variables were compared using a 2-sided Student t test and ordinal variables used the Kruskal–Wallis test. The Wilcoxon test was used for comparison of non-normally distributed data. All p values were 2-sided and a p < 0.05 was considered to indicate statistical significance.
Results
A total of 2263 adult patients were included in the final analysis (Fig. 1). The baseline characteristics of the study population are presented in Table 1. Apart from a predominance of men in the higher RC subset (72.3% vs 48.7%; p value < 0.01), the two groups of interest were balanced in terms of age, race, median body mass index (BMI), admission SOFA score, and days on the ventilator prior to the first extubation attempt. Similarly, the P/F ratio on the day of first extubation was comparable between the two subpopulations.
When considered as a continuous variable, median RSBI values were lower in the higher RC group (32 [IQR 26–39] vs 37 [IQR 31–47]; p value < 0.01). Only 24 patients in the overall population had an RSBI value of 105 or greater and all belonged to the lower RC group.
Extubation failure within 72 h was significantly more frequent in the lower RC group (13.6% vs 8.6%; p value < 0.01; Fig. 2). In either subset, most reintubations occurred in the first 24 h (149/216 in the lower RC group and 41/58 in the higher RC group). Inpatient deaths were also more frequent in the lower compliance group (11.5% vs 6.1%: p value < 0.01).
In a multivariate logistic regression model adjusting for age, sex, BMI, admission SOFA score, number of days on the ventilator, and the P/F ratio on the day of extubation, a calculated RC < 50 mL/cm H2O was associated with higher odds of extubation failure at 24 h (adjusted odds ratio [aOR] 1.45; 95% confidence interval [95% CI] 1.00–2.10) and at 72 h (aOR 1.58; 95% CI 1.15–2.17) (Table 2). By contrast, when the RSBI replaced RC as a continuous variable, it displayed no significant association with extubation failure within 24 h (aOR 1.00 per 1-unit change; 95% CI 0.99–1.01) or within 72 h (aOR 1.00; 95% CI 0.99–1.01).
Discussion
In this study, we investigated the role of RC in patients who had a successful SBT. Our main findings include the following: (1) RC less than 50 mL/cm H2O is associated with extubation failure at 72 h; (2) reintubations occur more often in the first 24 h; (3) RC less than 50 mL/cm H2O is associated with a higher frequency of inpatient deaths. These findings were significant even after adjusting for age, sex, severity of disease, and number of days on the ventilator prior to extubation.
Extubation failure has been associated with post-extubation stridor, upper airway patency, positive fluid balance 24 h prior to extubation, excess bronchial secretions, inadequate cough strength, duration of mechanical ventilation > 72 h, RSBI greater than 105 breaths/min/L, and a prior failed weaning attempt [6, 12, 13]. Some studies have attributed this variation to the patient subpopulation, particularly those with chronic obstructive pulmonary disease or with a high asynchrony index [14, 15]. When comparing cause of respiratory failure in the compliance subsets, those patients with principal admission diagnoses of acute respiratory distress syndrome (ARDS), asthma, or COPD were more likely to have a RC less than 50 mL/cm H2O (Table S1). Our findings suggest the addition of RC as another physiological discriminate to better predict extubation failure, even in those who had successful SBT with RSBI < 105.
The literature examining the role of static compliance in extubation readiness is limited. Okabe et al. concluded that there is an increased probability of extubation failure seen with compliance under 50–60 mL/cm H2O [12]. While we concluded a similar threshold for extubation failure of less than 50 mL/cm H2O, the former study was restricted to postoperative patients alone, whereas our study extended its inclusion to all mechanically ventilated adult critical care patients [12].
The role of static compliance as an index for pulmonary overdistension, which has been independently linked to extubation failure, is well established [16,17,18]. In patients with a reduced inspiratory capacity, an increase in tidal volume impinges on the upper plateau of the pressure–volume curve leading to the decrease in static compliance with clinical implications of increased pulmonary vascular resistance in ventilated regions and susceptibility to eventual collapse [16]. This inverse role in dynamic hyperinflation was later applied to weaning trials in COPD patients. Static compliance was found to not significantly differ from that of normal subjects except on the first day of mechanical ventilation, when subjects exhibited marked dynamic hyperinflation; however, this study was limited in its evaluation of the SBT, when these patients may exhibit marked dynamic hyperinflation [17]. This was further extrapolated in spontaneously breathing patients, when a prospective cohort of patients receiving mechanical ventilation demonstrated that the application of extrinsic PEEP led to an increase in the end-expiratory lung volume which significantly correlated with static compliance [18]. We concluded similar findings in our analysis of 304 patients (13.4%) with a pre-existing history of COPD. At time of SBT, this population subset had a median RC of 36 (IQR 28–50) with 72 patients (23.7%) requiring reintubation.
Several studies have evaluated alternative cutoff RSBI thresholds in predicting extubation failure. Frutos–Vivar et al. reported a threshold of 57 breaths/min/mL increased the risk of reintubation from 11 to 18% [13]. Other studies have documented the significant differences in RSBI between reintubated and non-reintubated patients, but with varying medians [19,20,21]. No significant difference in sensitivity or specificity was noted in RBSI thresholds of 80 to 105 compared to less than 80 [22]. To our knowledge, the comparison of RC to RSBI as a predictive index has not been evaluated. Only 24 of the 2263 extubated patients (1.06%) had a RSBI value of greater than 105 breaths/min/mL, yet 274 (12%) failed extubation in our study. All patients who exceeded the RSBI threshold did, however, have a RC of less than 50 mL/cm H2O.
Extubation failure alone is associated with increased mortality [1]. We found that a RC of less than 50 mL/cm H2O was not only associated with extubation failure, but with an increased inpatient mortality of 11.9% vs 6.1%. Static compliance and its mortality prediction had not been previously defined, but rather suggested in relation to the mortality benefit cited with strategies to decrease driving pressure [23,24,25]. Driving pressure is measured in the absence of inspiratory effort and calculated by the following: plateau pressure–PEEP. When disassociated from this variable, individual changes in VT and PEEP do not lead to mortality benefit [24]. We may have concluded similar findings by electing to measure static versus dynamic compliance.
Limitations
This study has several limitations. First, due to the retrospective design, selection bias may have been introduced pending availability of electronic health records. Such data points excluded due to availability of electronically extracted data included reason for intubation and use of non-invasive ventilatory support following extubation. Second, while a standardized ventilator weaning protocol was in place, adaptation, deviation, and variability of practice among providers may have also introduced bias. Such variability highlighted within the protocol included trial duration and range of CPAP and PSV. Also, while RC was calculated at completion of SBT after patients were returned to their prior ventilatory settings, we cannot account for variability in muscular activity at time of calculation. There was also a male predominance noted in the higher RC subset (72.3% vs 48.7%; p value); however, the multivariate logistic regression model adjusted for this variable when evaluating RC and its primary association. Finally, this study’s inclusion period ended prior to the COVID-19 pandemic. We recommend future studies comparing RC in non-COVID to COVID patients.
Conclusion
Traditional protocolized weaning predictors and parameters remain insensitive in risk stratifying patients with acute respiratory failure for extubation success. We conclude that static RC, measured at the day of extubation, is a promising predictor for extubation failure. We recommend further validation studies in prospective cohorts.
References
Blackwood B et al (2010) Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev (5): CD006904. https://doi.org/10.1002/14651858.CD006904.pub2 Update in: Cochrane Database Syst Rev 11:CD006904 (2014)
Esteban A et al (1999) Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish lung failure collaborative group. Am J Respir Crit Care Med 159(2):512–518
Ely EW et al (1996) Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 335(25):1864–1869
Torres A et al (1995) Re-intubation increases the risk of nosocomial pneumonia in patients needing mechanical ventilation. Am J Respir Crit Care Med 152(1):137–141
Yang KL, Tobin MJ (1991) A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 324(21):1445–1450
Boles JM et al (2007) Weaning from mechanical ventilation. Eur Respir J 29(5):1033–1056
Vallverdu I et al (1998) Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med 158(6):1855–1862
MacIntyre NR et al (2001) Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American college of chest physicians; the American association for respiratory care; and the American college of critical care medicine. Chest 120(6 Suppl):375S-S395
Nassar BS, Collett ND, Schmidt GA (2012) The flow-time waveform predicts respiratory system resistance and compliance. J Crit Care 27(4):418 e7–14
Mora Carpio AL and Mora JI (2021) Ventilator Management. In: StatPearls. StatPearls publishing, Treasure Island
Su K-C et al (2012) Spontaneous breathing trial needs to be prolonged in critically ill and older patients requiring mechanical ventilation. J Crit Care 27(3):324.e1-324.e7
Okabe Y et al (2018) Lung-thorax compliance measured during a spontaneous breathing trial is a good index of extubation failure in the surgical intensive care unit: a retrospective cohort study. J Intensive Care 6:44
Frutos-Vivar F et al (2006) Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest 130(6):1664–1671
Brochard L et al (1994) Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation. Am J Respir Crit Care Med 150(4):896–903
Sousa MLDA et al (2020) Predictors of asynchronies during assisted ventilation and its impact on clinical outcomes: The EPISYNC cohort study. J Crit Care 57:30–35
Suter PM, Fairley HB, Isenberg MD (1978) Effect of tidal volume and positive end-expiratory pressure on compliance during mechanical ventilation. Chest 73(2):158–162
Alvisi R et al (2000) Predictors of weaning outcome in chronic obstructive pulmonary disease patients. Eur Respir J 15(4):656–662
Fernandez Mondejar E et al (1992) Increase in lung volume originated by extrinsic PEEP in patients with auto-PEEP. The role of static lung compliance. Intensive Care Med 18(5):269–273
Lai CC et al (2016) Establishing predictors for successfully planned endotracheal extubation. Medicine (Baltimore) 95(41):e4852
Bien MY et al (2004) Breathing pattern variability: a weaning predictor in postoperative patients recovering from systemic inflammatory response syndrome. Intensive Care Med 30(2):241–247
Smina M et al (2003) Cough peak flows and extubation outcomes. Chest 124(1):262–268
Trivedi V et al (2022) The usefulness of the rapid shallow breathing index in predicting successful extubation: A systematic review and meta-analysis. Chest 161(1):97–111
Toufen Junior C et al (2018) Driving pressure and long-term outcomes in moderate/severe acute respiratory distress syndrome. Ann Intensive Care 8(1):119
Amato MB et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372(8):747–755
Baedorf Kassis E, Loring SH, Talmor D (2016) Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med 42(8):1206–1213
Funding
Authors received no funding for this investigator initiated study.
Author information
Authors and Affiliations
Contributions
All authors contributed equally in manuscript preparation. GN, FI, and LA did all analysis and final interpretation.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report any potential conflicts of interest with the materials presented.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abplanalp, L.A., Ionescu, F., Calvo-Ayala, E. et al. Static Respiratory System Compliance as a Predictor of Extubation Failure in Patients with Acute Respiratory Failure. Lung 201, 309–314 (2023). https://doi.org/10.1007/s00408-023-00625-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-023-00625-7