Abstract
Introduction
In phase 3 trials (COUGH-1/COUGH-2), gefapixant 45 mg twice daily significantly reduced 24-h cough frequency vs placebo in refractory or unexplained chronic cough (RCC or UCC).
Methods
Here, the efficacy of gefapixant 45 mg vs placebo was evaluated across COUGH-1/COUGH-2 in predefined subgroups based on sex, region, age, cough duration, cough severity, cough frequency, and diagnosis (RCC, UCC). Awake cough frequency reductions at Week 12 and LCQ response rates (i.e., ≥ 1.3-point improvement) at Week 24 were assessed.
Results
Among 1360 participants analyzed, gefapixant 45 mg resulted in consistent awake cough frequency reductions overall and across predefined subgroups at Week 12. Gefapixant also resulted in improved LCQ scores across subgroups at Week 24; ≥ 70% of participants in each subgroup treated with gefapixant 45 mg had an LCQ response.
Conclusion
These data suggest gefapixant 45 mg provides consistent objective and subjective efficacy across subgroups of individuals with RCC or UCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic cough (cough lasting > 8 weeks), a burdensome condition that negatively affects quality of life (QOL) [1], has a prevalence between 4 and 18% [2, 3]. Some patients experience chronic cough associated with certain conditions (e.g., asthma, gastroesophageal reflux disease, upper-airway cough syndrome). However, others experience chronic cough that does not resolve despite extensive investigation and appropriate treatment of comorbid conditions [refractory chronic cough (RCC)] or experience chronic cough that has no identifiable associated conditions despite thorough diagnostic workup [unexplained chronic cough (UCC)] [4, 5]. There is a lack of treatments indicated for RCC or UCC. Off-label treatments may have undesirable side effects [6, 7], and patients may have limited accessibility to nonpharmacologic interventions (e.g., speech therapy) [8]. Treatments that improve both objective cough frequency and subjective cough-specific QOL are needed.
Gefapixant is an oral, peripherally acting P2X3-receptor antagonist under investigation for RCC and UCC [9]. Two phase 3, randomized, placebo-controlled trials of gefapixant showed that relative to placebo, twice-daily gefapixant 45 mg resulted in statistically significant reductions in the primary endpoint, 24-h cough frequency, after 12 (COUGH-1) and 24 (COUGH-2) weeks of treatment. The pooled 24-h cough frequency response was consistent across predefined subgroups at Week 12 [10]. The proportion of participants with a clinically meaningful increase from baseline in the Leicester Cough Questionnaire (LCQ) total score, a key secondary endpoint of interest, was significantly improved after 24 weeks of treatment with gefapixant 45 mg vs placebo in COUGH-2 [10].
This analysis further investigated the efficacy of gefapixant, as assessed via 24-h cough frequency and secondary endpoints of awake cough frequency and the LCQ, across a pooled sample of participants from COUGH-1 and COUGH-2, including in predefined subgroups.
Methods
Participants
Participants were enrolled in one of two phase 3, randomized, placebo-controlled, double-blind, parallel-group clinical trials evaluating the P2X3-receptor antagonist gefapixant for treatment of RCC or UCC (COUGH-1, NCT03449134, COUGH-2, NCT03449147). Eligibility criteria have been described, including age of ≥ 18 years, chronic cough lasting ≥ 1 year, self-reported score of ≥ 40 mm on the cough severity visual analog scale (VAS), and RCC or UCC diagnosis per American College of Chest Physicians guidelines [11].
Study Design
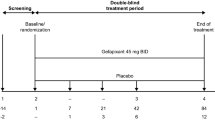
The design and rationale of COUGH-1 and COUGH-2 have been reported [11]. The main study periods were 12 (COUGH-1) and 24 (COUGH-2) weeks. Previous predefined analyses assessed the primary endpoint, 24-h cough frequency, in predefined subgroups including sex, region (North America, Europe, Asia Pacific, other), age (< 65, ≥ 65 years), cough duration (< 10, ≥ 10 years), cough severity VAS (< 60, ≥ 60 mm), 24-h coughs/h (< 20, ≥ 20 coughs/h), and primary diagnosis (RCC, UCC) [10]. The current analysis assessed additional endpoints (awake cough frequency and LCQ) in the same predefined subgroups.
Because cough frequency counts were obtained through Week 12 in COUGH-1 and Week 24 in COUGH-2, pooled awake cough frequency in the current analysis is reported for Week 12 (i.e., the last shared time point across trials for cough frequency measurements). Awake cough frequency was assessed by trained cough analysts. To distinguish awake and sleep periods, Vitalograph analysts defined the starting and ending times for the longest sleep period in each 24-h recording (inclusive of awake periods < 20 min) by considering activity levels, speech, and sounds associated with sleeping (e.g., breathing patterns, snoring). 24-h cough frequency subgroup analyses, but not overall pooled 24-h cough frequency results, were previously reported [10]. For the current analysis, change from baseline in log-transformed cough frequency at Week 12 was evaluated using longitudinal analysis of covariance for the pooled sample (both 24-h and awake cough frequency) and each subgroup (awake cough frequency). Estimated relative reductions from baseline to Week 12 for gefapixant relative to placebo (with 95% CIs) are reported across subgroups. As Week 24 was the time point used for the LCQ as a key secondary endpoint in COUGH-2, data for the LCQ were pooled at Week 24. The proportion of participants with a ≥ 1.3-point increase from baseline to Week 24 on the LCQ total score was evaluated using a logistic regression model for the pooled sample and each subgroup. Odds ratios (with 95% CIs) for achieving a ≥ 1.3-point increase in LCQ total score are reported across subgroups.
Results
Baseline Characteristics and Demographics
Of 1360 participants, 678 were randomized to placebo and 682 were randomized to gefapixant 45 mg. Mean cough duration was ~ 11 years, 75% were female, 62% had a primary diagnosis of RCC, 71% had a cough severity ≥ 60 mm on the 100 mm cough severity VAS, and 51% had a baseline cough frequency ≥ 20 coughs/h. Comorbidities reported with cough included asthma (n = 571, 42%), gastroesophageal reflux disease (n = 538, 40%), and upper-airway cough syndrome (n = 86, 6%). The most frequently prescribed medications were similar between the placebo and gefapixant groups and consistent with prior treatments of cough-associated conditions [i.e., obstructive airway disease (71%), acid reflux-related disorders (54%), and nasal preparations (54%)].
Pooled Overall Data from COUGH-1 and COUGH-2
Primary trial results showed that treatment with gefapixant 45 mg, but not gefapixant 15 mg, resulted in significant reduction of 24-h cough frequency; therefore, only results from the gefapixant 45 mg and placebo cohorts were assessed.
Gefapixant 45 mg reduced 24-h cough frequency [(estimated relative reduction, 18.6% (95% CI 9.2–27.1%)] and awake cough frequency [estimated relative reduction, 17.4% (95% CI 7.5–26.2%)] at Week 12. At Week 24, gefapixant 45 mg was associated with a higher LCQ response rate (i.e., ≥ 1.3-point increase in LCQ total score) than placebo [73.5% vs 67.0%; estimated odds ratio, 1.37 (95% CI 1.06–1.77%)].
Objective and Subjective Efficacy Across Subgroups
Across subgroups, those receiving gefapixant 45 mg demonstrated reductions in awake cough frequency at Week 12 relative to baseline [geometric mean ratios (Week 12/baseline) between 0.32 and 0.46, Table 1]. The range of responses among participants receiving placebo varied between geometric mean ratios of 0.39 and 0.54 across subgroups. Estimated relative reductions in awake cough frequency from baseline to Week 12 for gefapixant 45 mg relative to placebo are reported in Fig. 1a.
Objective and subjective efficacy in subgroups. a Relative reduction in awake cough frequency for gefapixant 45 mg BID vs placebo at Week 12 by subgroups and b odds ratios of achieving a ≥ 1.3-point increase from baseline in LCQ total score with gefapixant 45 mg BID vs placebo at Week 24 by subgroups. BID twice daily, LCQ Leicester Cough Questionnaire, RCC refractory chronic cough, UCC unexplained chronic cough, VAS visual analog scale
Across subgroups, ≥ 70% of participants treated with gefapixant 45 mg had a clinically meaningful increase in LCQ total score at Week 24 (range 70–81%, Table 2). The range of LCQ response rates for the placebo group varied between 60% and 82%. Odds of achieving a ≥ 1.3-point increase from baseline in LCQ total score with gefapixant 45 mg relative to placebo are reported in Fig. 1b.
Discussion
Previous predefined analyses were conducted to assess the primary endpoint of COUGH-1 and COUGH-2 (i.e., 24-h cough frequency) in protocol-defined subgroups [10]. The purpose of this analysis of additional endpoints (e.g., awake cough frequency, LCQ) in the same predefined subgroups was to determine if any one subgroup was driving overall trial results for these endpoints. Overall results demonstrate that gefapixant 45 mg improved 24-h cough frequency, awake cough frequency, and cough-specific QOL vs placebo in participants with RCC or UCC and, consistent with previous subgroup analyses reported for 24-h cough frequency [10], gefapixant 45 mg improved awake cough frequency and LCQ across predefined subgroups. Collectively, these results support the broad clinical benefit of gefapixant 45 mg in RCC and UCC. The main limitations were that sample sizes were not sufficiently powered to formally assess differences between subgroups with prespecified hypotheses, and sample sizes were limited for some subgroups or imbalanced between categories within subgroups (e.g., males vs females). Although statistical precision increases in a larger, pooled data set, apparent differences in efficacy between subgroups should be carefully interpreted for the reasons explained below.
Improvement with gefapixant 45 mg from baseline was generally consistent across subgroups. However, estimated relative reductions are impacted by both the treatment effect in the active group as well as the placebo response, which must be considered for interpretation. For example, although participants with a ≥ 10- vs < 10-year cough duration at baseline who were treated with gefapixant 45 mg had similar reductions in awake cough frequency from baseline (60–62%), participants with a baseline cough duration < 10 years experienced a greater placebo effect (58% reduction from baseline to Week 12) compared with those with a baseline cough duration ≥ 10 years (46% reduction), which led to a higher estimated relative reduction in awake cough frequency among participants with longer baseline cough duration. Both active treatment and placebo effects may have played a role in comparisons of estimated relative reductions in awake cough frequency between baseline cough frequency subgroups [i.e., those with < 20 coughs/h had a more moderate reduction from baseline than those with ≥ 20 coughs/h (54% vs 68% reductions) but also had a smaller placebo response (48% vs 59% reductions)]. The relative differences between these subgroups would therefore have been even more marked had the placebo responses been more comparable.
As a single-item assessment, the cough severity VAS is a relevant cough measure for clinical practice and was recently validated as a reliable and responsive measure in patients with chronic cough [12]. In the cough severity VAS subgroups, placebo responses were comparable (55% and 54% for < 60 and ≥ 60 mm, respectively), and those with more severe cough demonstrated a greater response to gefapixant compared with those with less severe cough; however, the numbers of participants in the subgroups were not well balanced and the confidence intervals were wide. Ultimately, all prespecified subgroups receiving gefapixant 45 mg experienced a ≥ 50% reduction from baseline in awake cough frequency, supporting a general improvement in cough regardless of baseline characteristics (Table 1).
Similar to awake cough frequency, improvements in LCQ with gefapixant 45 mg were generally consistent across subgroups, including LCQ response rates between 70% and 81% (Table 2). Just as those with higher cough frequency at baseline (≥ 20 coughs/h) had greater reductions in awake cough frequency compared with those with lower cough frequency (< 20 coughs/h), there were greater proportions of LCQ responders in those with higher vs lower baseline cough frequency. Additionally, in some subgroups, there were apparent differences between objective efficacy (i.e., awake cough frequency) and subjective efficacy (i.e., LCQ). The following considerations may explain this pattern of results. First, awake cough frequency and LCQ in this analysis were studied at different time points (i.e., Week 12 vs Week 24, respectively). Second, cough frequency is measured over 24-h, compared with a 2-week recall period for the LCQ, so these two endpoints may differ in sensitivity to change. Third, each outcome measures a different construct, and it is therefore not expected that the changes in LCQ and awake cough frequency would strongly correlate [13, 14]. Because no single measure can capture the full dimensions of the impact of chronic cough on patients, the use of both objective and subjective endpoints can provide richer detail regarding cough improvement and its effect on patients’ subjective experiences [15].
To conclude, data collected in the largest sample of individuals with RCC or UCC to date support the objective and subjective efficacy of gefapixant 45 mg, with relatively consistent improvements across sociodemographic and clinical-feature subgroups. Gefapixant, which is currently only approved in Japan for the treatment of RCC or UCC, may address a large unmet need.
Data Availability
The data sharing policy, including restrictions, of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA is available at http://engagezone.msd.com/ds_documentation.php. Requests for access to the clinical study data can be submitted through the Engage Zone site or via email to dataaccess@merck.com.
Code Availability
Not applicable.
References
Chamberlain SA, Garrod R, Douiri A et al (2015) The impact of chronic cough: a cross-sectional European survey. Lung 193:401–408
Çolak Y, Nordestgaard BG, Laursen LC et al (2017) Risk factors for chronic cough among 14,669 individuals from the general population. Chest 152:563–573
Satia I, Mayhew AJ, Sohel N et al (2021) Prevalence, incidence and characteristics of chronic cough among adults from the Canadian Longitudinal Study on Aging. ERJ Open Res 7:00160–02021
Morice AH, Millqvist E, Bieksiene K et al (2020) ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 55:1901136
Irwin RS, Baumann MH, Bolser DC et al (2006) Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest 129(1 suppl):1S–23S
Song W-J, Chung KF (2020) Pharmacotherapeutic options for chronic refractory cough. Expert Opin Pharmacother 21:1345–1358
Ryan NM, Birring SS, Gibson PG (2012) Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet 380:1583–1589
Slovarp L, Loomis BK, Glaspey A (2018) Assessing referral and practice patterns of patients with chronic cough referred for behavioral cough suppression therapy. Chron Respir Dis 15:296–305
Richards D, Gever JR, Ford AP et al (2019) Action of MK-7264 (gefapixant) at human P2X3 and P2X2/3 receptors and in vivo efficacy in models of sensitisation. Br J Pharmacol 176:2279–2291
McGarvey LP, Birring SS, Morice AH et al (2022) Efficacy and safety of gefapixant, a P2X3 receptor antagonist, in refractory chronic cough and unexplained chronic cough (COUGH-1 and COUGH-2): results from two double-blind, randomised, parallel-group, placebo-controlled, phase 3 trials. Lancet 399:909–923
Muccino DR, Morice AH, Birring SS et al (2020) Design and rationale of two phase 3 randomised controlled trials (COUGH-1 and COUGH-2) of gefapixant, a P2X3 receptor antagonist, in refractory or unexplained chronic cough. ERJ Open Res 6:00284–02020
Martin Nguyen A, Bacci ED, Vernon M et al (2021) Validation of a visual analog scale for assessing cough severity in patients with chronic cough. Ther Adv Respir Dis 15:17534666211049744
Decalmer SC, Webster D, Kelsall AA et al (2007) Chronic cough: how do cough reflex sensitivity and subjective assessments correlate with objective cough counts during ambulatory monitoring? Thorax 62:329–334
Kelsall A, Houghton LA, Jones H et al (2011) A novel approach to studying the relationship between subjective and objective measures of cough. Chest 139:569–575
Vernon M, Leidy NK, Nacson A et al (2009) Measuring cough severity: perspectives from the literature and from patients with chronic cough. Cough 5(1):5
Acknowledgements
Funding for this research was provided by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. Medical writing and editorial assistance were provided under the direction of the authors by Alexandra Kennedy, PhD, and Jenna Lewis, MA, ELS, of MedThink SciCom. This assistance was funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Funding
This study, including the analysis and manuscript writing/editorial assistance, was supported by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Author information
Authors and Affiliations
Contributions
JAS, SSB, PVD, AHM, SG, BI, AMN, JS, and DM: substantially contributed to conception, design, or planning of the study. JAS, SSB, LPM, AHM and JS: substantially contributed to acquisition of the data. AHM, IDP, SG, QL and JS: substantially contributed to analysis of the data. JAS, SSB, PVD, LPM, AHM, IDP, IS, SG, CLR, QL, AMN, JS and DM: substantially contributed to interpretation of the results. IDP and JS: substantially contributed to drafting of the manuscript. SSB, PVD, LPM, AHM, IS, SG, BI, CLR, QL, AMN, JS and DM: substantially contributed to critically reviewing or revising the manuscript for important intellectual content. All authors reviewed the final version of the manuscript and are in agreement with its content and submission; have access to all relevant study data and related analyses and vouch for the completeness/accuracy of the presented data; and agree to be accountable for all aspects of the work and ensure that any questions related to the accuracy or integrity of any part of the work will be appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
JAS has received personal fees from Bayer, Bellus Healthcare, Boehringer Ingelheim, GlaxoSmithKline, Menlo, NeRRe Pharmaceuticals, and Shionogi; nonfinancial support from Vitalograph; grant support and personal fees related to the submitted work from Afferent Pharmaceuticals/Merck & Co., Inc.; and grant support from Bayer, Bellus, GlaxoSmithKline, Menlo, and NeRRe Pharmaceuticals. The VitaloJAK algorithm is owned by Manchester University NHS Foundation Trust (MFT) and licensed to Vitalograph Ltd; MFT receives royalties from Vitalograph that may be shared with the department in which JAS works. JAS is also funded by the NIHR Manchester Biomedical Research Centre and a Wellcome Investigator Award and is an NIHR Senior Investigator. SSB has received advisory board/consultancy fees from Bayer, Menlo, Merck & Co., Inc., Patara, Pfizer, and Sanofi; speaker fees from Roche; and grant support from Boehringer Ingelheim and Merck & Co., Inc. PVD has received advisory board/consultancy fees from Bayer HealthCare Pharmaceuticals, Bellus Health Inc, Chiesi, Merck & Co., Inc., and Shionogi. PVD is editor-in-chief of Lung. LPM has received advisory board/consultancy fees from Applied Clinical Intelligence, Bayer, Bellus Health, Bionorica, Chiesi, Merck & Co., Inc., Nocion Therapeutics, and Shionogi. AHM has received consulting fees from Bayer, Bellus, Boehringer Ingelheim, Merck & Co., Inc., Pfizer, Proctor & Gamble, and Shionogi; lecture fees from AstraZeneca and Boehringer Ingelheim; and grant support from Afferent, Infirst, Merck & Co., Inc., and Proctor & Gamble. IDP has received personal fees from Aerocrine, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Genentech, GlaxoSmithKline, Knopp, Novartis, Regeneron, Sanofi, and Teva; and grant support from NIHR. IS has received personal fees from educational talks for general practitioners from AstraZeneca and GlaxoSmithKline; grants and personal fees from Merck Canada; consulting fees from Genentech; a European Respiratory Society Respire 3 Marie Curie Fellowship; and an E.J. Moran Campbell Early Career Award from the Department of Medicine, McMaster University (outside the submitted work). SG, BI, CLR, QL, AMN, JS, and DM are employees of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ USA, who may own stock and/or hold stock options in the Company.
Ethical Approval
The COUGH-1/COUGH-2 trials were performed in accordance with applicable federal regulations. All sites received approval from institutional review boards or independent ethics committees.
Consent to Participate
For the COUGH-1/COUGH-2 trials, all patients provided written informed consent before enrollment.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smith, J.A., Birring, S.S., Dicpinigaitis, P.V. et al. Improvements in Objective and Subjective Measures of Chronic Cough with Gefapixant: A Pooled Phase 3 Efficacy Analysis of Predefined Subgroups. Lung 200, 423–429 (2022). https://doi.org/10.1007/s00408-022-00553-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00553-y