Abstract
Introduction
Driving pressure (DP) while on ECMO has been studied in acute respiratory distress syndrome (ARDS) but no studies exist in those on ECMO without ARDS. We aimed to study association of mortality with DP in all patients on ECMO and compare change in DP before and after initiation of ECMO.
Methods
Consecutive patients placed on ECMO either veno-arterial ECMO or veno-venous ECMO between August 2010 and February 2017 were reviewed. The outcomes were compared based on DP before and after ECMO initiation.
Results
A total of 192 patients were included: 68 (35%) had ARDS while 124 (65%) did not. There were 70 individuals for whom DP was available, 33 (47%) had a decrease in DP, whereas 32 (46%) had an increase in DP and 5 (7%) had no change in DP after ECMO initiation. Those with an increase in DP had a higher initial PEEP (14 vs 9 cm H2O, p < 0.001) and a higher PEEP decrease after ECMO (6.4 cm H2O vs by 2.5 cm H2O, p < 0.001). Those with an increase in DP had a significantly longer stay on ECMO than those without (p = 0.022). On multivariable analysis, higher DP 24 h after ECMO initiation was associated with an increase in 30-day mortality (OR 1.15, 75% CI 1.07–1.24, p ≤ 0.001).
Conclusion
A significant proportion of patients experienced an increase in driving pressure and decrease in compliance after initiation of ECMO. Higher driving pressure after initiation of ECMO is associated with increased adjusted 30-day mortality. Individualized ventilator strategies are needed to reduce mechanical stress while on ECMO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The past decade has seen an increased utilization of extracorporeal membrane oxygenation (ECMO) as a life sustaining strategy for respiratory and/or cardiac failure [1]. Veno-venous (VV)-ECMO is used to provide temporary gas exchange support in patients with primary respiratory failure and preserved cardiac function. However, veno-arterial (VA)-ECMO is used for temporary circulatory assistance in patients with cardiogenic shock or refractory cardiac arrest. Despite the increasing use, optimal management of mechanical ventilation on ECMO is not well established [2]. Research has focused on indications, timing, and outcomes in patients requiring ECMO; however, there are no large randomized control trials focusing on a preferred mechanical ventilatory strategy during ECMO.
ECMO support theoretically allows for a reduction in intensity of mechanical ventilation. The resultant decrease in lung stress and strain permits lung rest with potentially improvement in outcomes. Ultra-low tidal volume ventilation for lung protection is well accepted as best practice during ECMO [3]. However, how best to achieve this remains unclear. An international survey of all ELSO-registered ECMO centers showed a huge variability in the approach to mechanical ventilation during ECMO for acute respiratory distress syndrome (ARDS) [4]. The majority of these centers (77%) reported “lung rest” to be the primary goal of mechanical ventilation, whereas 9% reported “lung recruitment” to be their ventilation strategy. Various trials of ECMO have also used variable settings in both the treatment and control arms. This variability may impact outcomes in ECMO-supported patients.
There has been mounting evidence of the direct relationship of mechanical power applied to the lung and worsening injury [5]. However, a safety limit or the ideal titration method is unclear. In ARDS, driving pressure (DP) has emerged as a target to adjust tidal volume and PEEP to limit cyclic and dynamic strain during mechanical ventilation. Several retrospective studies following the initial analysis by Amato et al. have found DP as the variable that is most associated with mortality in ARDS [6]. Even though there are no prospective studies for DP as a target for ventilator management, it has consistently been replicated, is physiologically sound and easily measured at the bedside, making DP an increasingly accepted target for monitoring during mechanical ventilation in ARDS. However, DP while on ECMO has not been well studied. One retrospective study of ARDS patients by Cheu et al. has shown that DP during first 3 days of ECMO initiation was an independent predictor of mortality [7].
Also, even though DP is a term defined for ARDS, individuals requiring VA-ECMO support for cardiac failure are also at risk for atelectrauma and barotrauma, and DP may play a role in the ventilation in the setting of pulmonary edema due to acute cardiac failure. Prolonged mechanical ventilation while on ECMO support makes this group highly susceptible to ventilator-induced lung injury. There are no studies evaluating role of driving pressure in this subset of ECMO patients.
We aimed to study driving pressures before and after initiation of ECMO to compare groups with increase and decrease in driving pressure and their outcomes. We also aimed to study association of DP with mortality in patients on both VA- and VV-ECMO.
We hypothesized that a shift to ECMO would lead to a decrease in driving pressure as it allows for ultra-lung protective ventilation. In conjunction, higher driving pressure while on ECMO would be associated with higher mortality.
Methods
Patients
A retrospective study was performed including all the patients placed on either VA- or VV-ECMO between August 2010 and February 2017 at our tertiary care referral center. Patients who were cannulated at an outside facility and transferred to our hospital were also included. Those who had ECMO duration shorter than 24 h from cannulation were excluded in this study. The local Institutional Review Board for Human Research approved this study (IRB # 11D185) and the need for informed consent was waived due to the retrospective nature of the study.
Ventilator
Before consideration of ECMO initiation, all patients were sedated and ventilated with lung protective ventilation based on the mechanism of their disease process, arterial blood gas, and ventilator mechanics. The decision to initiate ECMO was made by the treating intensive care specialist [9]. Majority of patients received the Rotaflow pump (n = 164, 85%), whereas 5 (2.6%) received Biomedicus and 23 (11.9%) received the Cardiohelp pump for ECMO cannulation. Initial mechanical ventilator setting protocol after ECMO support was as follows: tidal volume 4–5 ml/kg PBW; PEEP 5–10 cm H2O; peak inspiratory pressure 25–30 cm H2O; respiratory rate 10–12 breaths per minute; and FiO2 adjusted to maintain arterial oxygen saturation above 90%.
Respiratory Data
Plateau pressure was measured by performing an end inspiratory hold maneuver on the ventilator. DP was calculated as the plateau pressure minus PEEP. Static respiratory system compliance was measured by tidal volume divided by DP. Murray score was calculated before and after ECMO initiation to stratify severity of acute lung injury [8].
Data Collection
Data were collected retrospectively on baseline characteristics, comorbidities, ARDS status, severity of illness score like APACHE II score among all included ECMO patients. Information regarding the ECMO circuit and ventilation parameters before and after initiation of ECMO was also recorded.
Endpoints
Data collected included duration on ECMO, death on ECMO, status at hospital discharge, and status at 30 days after termination of ECMO.
Grouping
All individuals who had DP measured both before and after initiation of ECMO were identified. Among those individuals, change in driving pressure was calculated as DP after ECMO minus DP before ECMO. Group A was defined as those who had an increase in DP and Group B was defined those who had a decrease in DP 24 h after initiation of ECMO. Those with no change in driving pressure were not included in this analysis.
Statistics
We described baseline characteristics of all patients on ECMO by ARDS status. Categorical variables were reported as numbers (percentages) and continuous variables as means ± standard deviation. Single-variable comparison was performed by student t test for continuous variables and chi-square or Fisher exact tests for categorical variables. We then compared ventilatory parameters 24 before and after initiation of ECMO by ARDS status. We performed single-variable and multivariable logistic regression analyses to evaluate association of driving pressure on ECMO with 30-day mortality in all patients. Known risk factors for mortality were included in the regression model for adjustment. We adjusted for age, sex, VA/VV-ECMO, days in the hospital before ECMO initiation, steroid use before ECMO, and cardiac arrest. Odd’s ratio (OR) was expressed with 95% confidence interval (CI) and p value less than 0.05 was considered to be significant. We also performed comparative analyses of characteristics and outcomes between groups A and B. Analyses were conducted in Stata 12.1 (Stat Corp, College Station, Texas).
Results
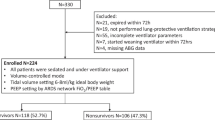
A total of 192 patients including 68 (35.4%) with ARDS and 124 (64.4%) with no ARDS were reviewed. A majority of ARDS patients (n = 53, 77.9%) were on VV-ECMO and a majority of non-ARDS patients (n = 115, 92.7%) were on VA-ECMO. A schematic distribution of the study population is shown in Fig. 1. The indication for ECMO initiation is listed in Table 1 for both VA- and VV-ECMO. The patient’s characteristics are shown in Table 2 based on the presence or absence of ARDS. Patients with ARDS were younger and had a higher BMI. No difference seen in APACHE II score between those with ARDS and without ARDS.
Before staring ECMO, individuals were ventilated with an average PEEP of 10.5 cm H2O and average plateau pressure of 27.4 cm H2O. Both plateau pressure and PEEP were higher in those with ARDS than those without ARDS before initiation of ECMO as shown in Table 3. Plateau pressure and PEEP decreased significantly after initiation of ECMO in both ARDS (p < 0.001) and non-ARDS individuals (p = 0.001). However, DP showed no change in both ARDS and non-ARDS after initiation of ECMO. Murray score among those without ARDS was 1.7 ± 0.9 before ECMO and 2.1 ± 0.5 after ECMO indicating a mild/moderate lung injury. Further comparisons of ventilatory parameters before initiation of ECMO and 24 h after ECMO among ARDS and non-ARDS patients are shown in Table 3.
Overall outcomes in the entire cohort of ECMO patients comparing those with ARDS and those without ARDS are shown in Table 4. The overall 30-day mortality of the entire study cohort was 47%. The 30-day mortality was higher in those without ARDS as compared to those with ARDS (54% vs 33%, p = 0.008).
In single-variable analysis, higher DP on ECMO was associated with an increase in odds of 30-day mortality (OR 1.09, 95% CI 1.03–1.16, p = 0.002) among all ECMO patients. This association was significant among those with ARDS (OR 1.10, 95% CI 1.00–1.21, p = 0.034) and those without ARDS (OR 1.04, 95% CI 1.04–1.24, p = 0.004). On multivariable analysis, higher DP on ECMO was significantly associated with an increase in mortality after adjusting for age, sex, VA/VV-ECMO, days in the hospital before ECMO initiation, steroid use before ECMO, cardiac arrest (OR 1.15, 75% CI 1.07–1.24, p ≤ 0.001).
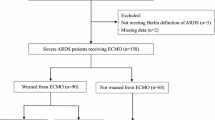
Among the 70 individuals for whom DP was available both before and after ECMO, Group A (those with increase in DP) consisted of 32 patients (46%), Group B (those with decrease in DP) consisted of 33 patients (47%), and the rest 5 (7%) had no change in DP after ECMO initiation. Table 5 shows comparisons of the 2 groups of the patients. Group A had 19 (59%) patients with ARDS and 13 (41%) without ARDS as compared to 13 (39%) with ARDS and 20 (61%) without ARDS in Group B. In Group A, average initial PEEP was higher than in Group B (14 ± 5 cm H2O in Group A vs. in 9 ± 4 cm H2O Group B, p < 0.001). Group A also had a more significant decrease in PEEP (p < 0.001) after ECMO initiation. PEEP decreased by 6.4 cm H2O in Group A while by 2.5 cm H2O on average in Group B after ECMO initiation. Even though both the groups started with a comparable compliance, the compliance greatly decreased in Group A as compared to Group B (change in compliance: − 7.8 in Group A vs 0.5 in Group B, p = 0.012).
Group A had a significantly longer stay on ECMO than Group B (13 ± 8 days in Group A vs 9 ± 4.9 days in Group B, p = 0.022). This trend was similar among those with ARDS (13 ± 7 days in Group A vs 9 ± 4.9 days in Group B, p = 0.125) and those without ARDS (14 ± 9 days in Group A vs 9 ± 4.9 days in Group B, p = 0.097). Death on ECMO and 30-day mortality was not significantly different between the two groups (Table 5).
Discussion
In this study, 46% of patients had an increase in driving pressure (Group A) after initiation of ECMO. These patients were more likely to be on VV-ECMO as compared to VA-ECMO. They also had a significantly higher drop in PEEP as compared to those in Group B (p < 0.001).
All patients on ECMO in our institution were ventilated at a tidal volume of 4 cc/kg IBW. The increase in driving pressure after ECMO is likely related to a protocolized application of ventilator settings including lower PEEP after initiation of ECMO. This implies that those maintained on high PEEP setting before ECMO were also ventilated with PEEP between 5 and 10 cm H2O leading to decrease in compliance and increase in driving pressure.
Both groups had a similar initial static compliance, but Group A had a lower compliance after ECMO. This decrease in compliance is likely due to an increase in atelectasis and decrease in lung recruitment. Even though ultra-lung protective ventilation while on ECMO is protective against barotrauma, there may be an increased risk of atelectrauma due to under-recruitment. Alveolar O2 tension decreases rapidly in an atelectatic lungs [9] leading to alveolar hypoxia, a potent inducer of lung inflammation [10]. Atelectasis can therefore lead to worsening of ventilator-associated lung injury.
These factors apply to patients on VV- or VA-ECMO. In our study, those without ARDS were also noted to have a decreased compliance and an elevated Murray Score. Patients on VA-ECMO have risk factors including cardiogenic pulmonary edema, postoperative lung damage, and thoracic compliance reduction after cardiac surgery making them susceptible to worsening lung injury and ARDS. Hence, atelectrauma can have deleterious consequences in both ARDS and non-ARDS patients.
In this study, those with an increase in driving pressure after ECMO had a significantly longer length of ECMO stay as compared to those with a decrease in driving pressure. Along with the mechanisms of lung injury and atelectrauma described above, it is also possible that those with under-recruitment have slower weaning due to worse oxygenation on weaning trials and also worse appearance of radiological abnormalities due to atelectasis impacting decision to wean by physicians. Although this group had higher initial PEEP which could represent higher severity of illness, initial compliance was similar in both groups and decreased after ECMO in this group with an increase in driving pressure. This highlights the importance of individualizing PEEP for adequate recruitment especially for those with severe disease requiring high initial levels of PEEP.
Some patients especially those on VA-ECMO and right heart failure can be adversely affected by high PEEP [11, 12]. Caution must be experienced in these patients and merits of high PEEP must be balanced with deleterious effects of positive pressure on right heart. On the other hand, patients with left heart failure on VA-ECMO who have a propensity for pulmonary edema may benefit from higher PEEP [13].
This further supports the fact that if ultra-lung protective ventilation is applied it should be applied with higher PEEP [14]. A recent study showed that near apneic ventilation in a pig model of acute lung injury supported by ECMO when compared to conventional protective ventilation decreased driving pressure by 40% and reduced mechanical power 10 times [5]. This resulted in less histologic lung injury and metalloproteinases activity as compared to conventional protective ventilation or non-protective ventilation. Therefore, reducing intensity of mechanical ventilation by reducing mechanical power and driving pressure is essential for prevention of ventilator-induced lung injury [15, 16].
In our study, a higher driving pressure on ECMO was an independent predictor of 30-day mortality in both unadjusted and adjusted analysis among all patients on ECMO. Driving pressure has previously been shown to be an independent predictor of mortality in ARDS patients [7], however, has not been evaluated in non-ARDS patients. Pham and colleagues also showed, in a cohort of 123 patients with influenza A(H1N1)-induced ARDS, that a higher plateau pressure on the first day of VV-ECMO for acute respiratory failure was significantly associated with ICU death (odds ratio = 1.33, 95% confidence interval = 1.14 to 1.59, p < 0.01) [17]. Our study further demonstrates that ventilation during ECMO may have an impact on mortality in both ARDS and non-ARDS patients.
Overall mortality among all patients with ECMO was 29%, higher among non-ARDS (33%) than those with ARDS (22%). This is because the non-ARDS patients include patients on VA-ECMO due to post-cardiotomy failure, acute myocardial infarction, and post-cardiac arrest including those who received cardiopulmonary resuscitation (23%) before ECMO.
We acknowledge the limitations of this study. The retrospective nature of analysis lends itself to misclassification and bias. Also, we only collected mortality information at 30 days after ECMO termination and no long-term outcomes were assessed, although we consider this short-term mortality as relevant and more directly related to the variable of interest, i.e., mechanical ventilation on ECMO. Secondly, we acknowledge that this is a very heterogenous group of patients as this includes all patients on ECMO including ARDS and non-ARDS patients. These groups have differences in their lung mechanics and different pathophysiological risks for lung injury. We note ventilatory parameters and Murray scores before and after initiation of ECMO but lack serial measurements of volume status or wedge pressures among those without ARDS. However, we showed that driving pressure was associated with mortality in both the subgroups of ARDS and non-ARDS patients. Third, we did not have direct information on the tidal volumes used in these patients. Our institution protocol mandated tidal volume of 4–5 ml/kg IBW for patients on ECMO; however, we are unable to evaluate protocol deviations in this cohort. Also, initial driving pressure before ECMO initiation is not available for all patients. This is due to the high volume of patients transferred from outside hospitals for ECMO or cannulated at an outside facility for ECMO. These patients did not have full ventilator mechanics recorded before ECMO. In spite of these shortcomings, this study is unique in evaluating driving pressures in both VA- and VV-ECMO population and one of the first studies to compare at driving pressure before and after initiation of ECMO.
Current ELSO guidelines published in 2017 now recommend using PEEP as high as tolerated in the first 24 h of ECMO [3]. This is a change from the 2013 guidelines when no PEEP recommendations were provided. However, protocol and practices continue to vary. Also, there are no set guidelines on driving pressures on ECMO. This study points towards targeting low driving pressure on ECMO in both ARDS and non-ARDS patients. More controlled studies are needed to establish exact targets while on ECMO. At our institution, we have now moved away from a uniform application of PEEP in patients on ECMO and focus on titrating PEEP based on lung compliance, adequate recruitment, and driving pressure.
Conclusion
A significant proportion of the patients had an increase in driving pressure and decrease in compliance after initiation of ECMO despite ultraprotective ventilation. This may be due to inadequate recruitment while on ECMO. Those with increase in driving pressure had a longer length of stay on ECMO. Elevated driving pressure after ECMO initiation was associated with increased adjusted 30-day mortality among both VA- and VV-ECMO. Adequate recruitment with individualized application of PEEP along with ultraprotective ventilation may improve outcome while on ECMO.
Data Availability
Raw data can be made available on request.
Change history
20 August 2020
The original version of this article unfortunately contained a mistake. The spelling of the Hitoshi Hirose name was incorrect. It was corrected in this erratum.
References
McCarthy FH, McDermott KM, Kini V, Gutsche JT, Wald JW, Xie D, Szeto WY, Bermudez CA, Atluri P, Acker MA, Desai ND (2015) Trends in U.S. extracorporeal membrane oxygenation use and outcomes: 2002–2012. Semin Thorac Cardiovasc Surg 27(2):81–88. https://doi.org/10.1053/j.semtcvs.2015.07.005
Zhang Z, Gu WJ, Chen K, Ni H (2017) Mechanical ventilation during extracorporeal membrane oxygenation in patients with acute severe respiratory failure. Can Respir J 2017:1783857. https://doi.org/10.1155/2017/1783857
A Extracorporeal Life Support Organization: ELSO Guidelines for Cardiopulmonary Extracorporeal Life Support and Patient Specific Supplements to the ELSO General Guidelines (August 2017). Version 1.4
Marhong JD, Telesnicki T, Munshi L, Del Sorbo L, Detsky M, Fan E (2014) Mechanical ventilation during extracorporeal membrane oxygenation. An international survey. Ann Am Thorac Soc 11(6):956–961. https://doi.org/10.1513/AnnalsATS.201403-100BC
Araos J, Alegria L, Garcia P, Cruces P, Soto D, Erranz B, Amthauer M, Salomon T, Medina T, Rodriguez F, Ayala P, Borzone GR, Meneses M, Damiani F, Retamal J, Cornejo R, Bugedo G, Bruhn A (2019) Near-apneic ventilation decreases lung injury and fibroproliferation in an acute respiratory distress syndrome model with extracorporeal membrane oxygenation. Am J Respir Crit Care Med 199(5):603–612. https://doi.org/10.1164/rccm.201805-0869OC
Aoyama H, Pettenuzzo T, Aoyama K, Pinto R, Englesakis M, Fan E (2018) Association of driving pressure with mortality among ventilated patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care Med 46(2):300–306. https://doi.org/10.1097/ccm.0000000000002838
Chiu LC, Hu HC, Hung CY, Chang CH, Tsai FC, Yang CT, Huang CC, Wu HP, Kao KC (2017) Dynamic driving pressure associated mortality in acute respiratory distress syndrome with extracorporeal membrane oxygenation. Ann Intensive care 7(1):12. https://doi.org/10.1186/s13613-017-0236-y
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138(3):720–723. https://doi.org/10.1164/ajrccm/138.3.720
Morrell NW, Nijran KS, Biggs T, Seed WA (1995) Magnitude and time course of acute hypoxic pulmonary vasoconstriction in man. Respir Physiol 100(3):271–281
Frohlich S, Boylan J, McLoughlin P (2013) Hypoxia-induced inflammation in the lung: a potential therapeutic target in acute lung injury? Am J Respir Cell Mol Biol 48(3):271–279. https://doi.org/10.1165/rcmb.2012-0137TR
Jardin F (2005) Acute leftward septal shift by lung recruitment maneuver. Intensive Care Med 31(9):1148–1149. https://doi.org/10.1007/s00134-005-2733-y
Jardin F, Vieillard-Baron A (2005) Monitoring of right-sided heart function. Curr Opin Crit Care 11(3):271–279
Dreyfuss D, Soler P, Basset G, Saumon G (1988) High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 137(5):1159–1164. https://doi.org/10.1164/ajrccm/137.5.1159
Schmidt M, Pellegrino V, Combes A, Scheinkestel C, Cooper DJ, Hodgson C (2014) Mechanical ventilation during extracorporeal membrane oxygenation. Crit Care 18(1):203. https://doi.org/10.1186/cc13702
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard J-CM, Carvalho CRR, Brower RG (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372(8):747–755. https://doi.org/10.1056/NEJMsa1410639
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, Protti A, Gotti M, Chiurazzi C, Carlesso E, Chiumello D, Quintel M (2016) Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 42(10):1567–1575. https://doi.org/10.1007/s00134-016-4505-2
Pham T, Combes A, Roze H, Chevret S, Mercat A, Roch A, Mourvillier B, Ara-Somohano C, Bastien O, Zogheib E, Clavel M, Constan A, Marie Richard JC, Brun-Buisson C, Brochard L (2013) Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med 187(3):276–285. https://doi.org/10.1164/rccm.201205-0815OC
Author information
Authors and Affiliations
Contributions
All authors listed have contributed sufficiently to the project to be included as authors, and all those who are qualified to be authors are listed in the author by-line.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupta, E., Awsare, B., Hiroshi, H. et al. Don’t Drive Blind: Driving Pressure to Optimize Ventilator Management in ECMO. Lung 198, 785–792 (2020). https://doi.org/10.1007/s00408-020-00381-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-020-00381-y