Abstract
Background
We studied the occurrence of intraoperative tidal alveolar recruitment/derecruitment, exhaled nitric oxide (eNO), and lung dysfunction in patients with and without chronic obstructive pulmonary disease (COPD) undergoing coronary artery bypass grafting (CABG).
Methods
We performed a prospective observational physiological study at a university hospital. Respiratory mechanics, shunt, and eNO were assessed in moderate COPD patients undergoing on-pump (n = 12) and off-pump (n = 8) CABG and on-pump controls (n = 8) before sternotomy (baseline), after sternotomy and before cardiopulmonary bypass (CPB), and following CPB before and after chest closure. Respiratory system resistance (R rs), elastance (E rs), and stress index (to quantify tidal recruitment) were estimated using regression analysis. eNO was measured with chemiluminescence.
Results
Mechanical evidence of tidal recruitment/derecruitment (stress index <1.0) was observed in all patients, with stress index <0.8 in 29% of measurements. Rrs in on-pump COPD was larger than in controls (p < 0.05). Ers increased in controls from baseline to end of surgery (19.4 ± 5.5 to 27.0 ± 8.5 ml cm H2O−1, p < 0.01), associated with increased shunt (p < 0.05). Neither Ers nor shunt increased significantly in the COPD on-pump group. eNO was comparable in the control (11.7 ± 7.0 ppb) and COPD on-pump (9.9 ± 6.8 ppb) groups at baseline, and decreased similarly by 29% at end of surgery(p < 0.05). Changes in eNO were not correlated to changes in lung function.
Conclusions
Tidal recruitment/derecruitment occurs frequently during CABG and represents a risk for ventilator-associated lung injury. eNO changes are consistent with small airway injury, including that from tidal recruitment injury. However, those changes are not correlated with respiratory dysfunction. Controls have higher susceptibility to develop complete lung derecruitment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is present in 4–27% of patients undergoing coronary artery bypass grafting (CABG) surgery [1]. The National Center for Health Statistics estimates that a total of 408,000 CABG procedures were performed in the United States in 2007 [2]. COPD is associated with risk for major perioperative complications after CABG such as prolonged mechanical ventilation [3], extubation failure [4], and increased hospital and 30-day mortality [5–7]. Chronic inflammation in COPD patients could compound the acute inflammatory response to surgery and cardiopulmonary bypass (CPB) [8] to produce intraoperative lung collapse and longer postoperative recovery times. Conversely, the increased respiratory resistance and reduced elastic recoil found in COPD could provide a mechanism to retard or even prevent the development of intraoperative atelectasis [9]. Despite these pathophysiological particularities of COPD patients and the significant number of COPD patients undergoing CABG, there is minimal information on perioperative lung dysfunction specifically addressing these patients.
Mechanical ventilation settings influence the magnitude of lung inflammation during cardiac surgery. Protective ventilatory strategies with low tidal volume (V T) and higher positive end-expiratory pressure (PEEP) have been shown to result in less inflammatory markers in both the bronchoalveolar lavage fluid and plasma [10, 11], and less time to extubation and the need for reintubation of cardiac surgical patients [12]. Such findings suggest that limiting maximal lung stretch and low-volume lung injury would reduce lung inflammation and morbidity in patients undergoing cardiac surgery. Minimization of pulmonary morbidity is an important goal because although the incidence of acute respiratory distress syndrome and acute lung injury after CPB is low (<2%), the associated mortality is high (>50%) [13, 14]. Moreover, after CABG surgery, hypoxemia has been reported as the most common cause for prolonged mechanical ventilation [15]. COPD patients present an exacerbated inflammatory response [16, 17] and could be at increased risk for respiratory complications.
It is currently unknown whether perioperative functional changes occur to justify each of the protective ventilatory interventions, i.e., PEEP and low V T, during the intraoperative period of cardiac surgery. If hyperinflation would be the predominant dysfunction, limitation of lung stretch (low V T) would be the relevant intervention. Instead, if tidal alveolar recruitment would be frequent, use of PEEP would be warranted since tidal opening and closing of alveoli and small airways in atelectatic regions during mechanical ventilation could increase the risk of ventilator-induced lung injury. Given that atelectasis is frequently present and the main cause of shunting and hypoxemia during cardiac surgery [18, 19], cyclic lung recruitment and concentration of mechanical forces [20] are likely during mechanical ventilation. The associated low-volume stress has been shown to be injurious in several models of acute lung injury [21, 22]. However, it is unknown to what degree low- and high-lung-volume stresses are present in patients with and without COPD undergoing cardiac surgery.
The “stress index” is a parameter derived from the airway pressure–time curve obtained at bedside during constant flow inflation to detect tidal recruitment and hyperinflation [23]. It was associated with computed tomography findings of tidal recruitment in experimental models of healthy [24] and surfactant-depleted lungs [23, 24]. Exhaled NO (eNO) reduction has been proposed as a marker of lung injury in the setting of CPB [25, 26]. In experimental ventilator-induced lung injury, a decline in eNO has been associated with cyclic opening and closing of peripheral airways during ventilation at low volume [21, 27]. In contrast to those eNO declines as indicators of injury, in COPD patients high eNO has been suggested as a surrogate marker of disease exacerbation [28].
In this study we measured respiratory mechanics, including the stress index, eNO, and gas exchange, in the intraoperative period of CABG surgery with cardiopulmonary bypass to (1) investigate whether tidal recruitment and hyperinflation occur at different surgical phases in patients with and without COPD; (2) evaluate whether eNO changes differ in those patient groups and whether those changes correspond to deterioration in respiratory mechanics and gas exchange; and (3) characterize lung function patterns in patients with moderate COPD in comparison with patients with no previous history of pulmonary disease. Finally, we also studied those variables in a group of COPD patients undergoing off-pump CABG surgery.
Methods
Patients
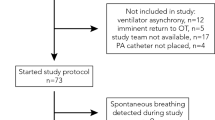
The study was approved by the Institutional Review Board of the Massachusetts General Hospital and written informed consent was obtained from all subjects. We sequentially studied 28 patients: 20 with moderate COPD as defined by GOLD criteria [29] and 8 nonsmokers without a history of pulmonary disease (controls). Exclusion criteria were presence of acute respiratory failure and emergency surgery. From the 20 COPD patients, 12 underwent on-pump CABG (COPD on-pump group) and 8 off-pump CABG (COPD off-pump group). Controls underwent on-pump CABG. Off-pump CABG was performed mainly because of severe ascending aortic atheromatosis.
Regular medication was maintained until surgery. Patients were premedicated with midazolam, induced with fentanyl and propofol, maintained with isoflurane, midazolam, and fentanyl, and had muscle paralysis with cisatracurium or pancuronium. Methylprednisolone 1 g was administered after intubation. Monitoring included a radial artery and a pulmonary artery catheter. Patients were mechanically ventilated with tidal volume (V T) = 8 ml/kg, inspired oxygen fraction (FIO2) = 100%, PEEP = 2.5 cm H2O, with respiratory rate adjusted to normocarbia. Ventilator parameters were kept constant before and after revascularization. A nitroglycerin infusion was used after revascularization at 50 mcg/min.
Procedures
All surgeries were done through a median sternotomy. We maintained the activated clotting time above 480 s. CPB was performed with systemic cooling to 30–33°C, double-stage venous cannula, and ascending aorta cannulation. Cardiac arrest was achieved by cold or warm blood antegrade and retrograde cardioplegia. The flow was maintained at 2.4 L/min/m2, with a mean arterial pressure >50 mmHg. During CPB, the expiratory limb of the breathing circuit was opened to atmosphere with lungs passively deflated. Before weaning from CPB, at least one recruitment maneuver to a peak inspiratory pressure of 20–25 cm H2O with direct visualization of lung expansion was performed. Off-pump CABG surgery was performed using a Genzyme stabilizing system (Genzyme Corporation; Cambridge, MA), Silastic rubber sutures were placed proximal and distal to the anastomotic site as coronary artery occluders, an intraluminal shunt was placed in case of hemodynamic instability, and a blower was used for insufflating humidified CO2 to ensure a bloodless operative field. No conversion to CPB occurred.
Physiological Measurements
Physiological measurements were performed at four time points chosen to represent major interventional phases encompassing the period of initial lung insult: (1) following intubation, before sternotomy; (2) after sternotomy, before revascularization; (3) before chest closure, following revascularization (i.e., after CPB for on-pump CABG); and (4) after chest closure, at the end of surgery. Hemodynamic measurements consisted of heart rate, systemic and pulmonary artery pressure, central venous pressure, and cardiac output. Gas exchange measurements included arterial and mixed venous blood gases and shunt [30]. A respiratory analyzer (NICO, Respironics) was used for intraoperative monitoring of capnography and lung mechanics.
Respiratory Mechanics
The elastance and resistance of the respiratory system (E rs and R rs), and lungs (E L and R L) were estimated from measurements of airway (P aw) and esophageal (P es) pressures and respiratory flow \( \left( {\dot{V}} \right) \) (Ventrak, Novametrix). The equation P = R·\( \dot{V} \) + E·V + EEP was fit to measured data using multiple linear regression, where EEP was the pressure at the end of expiration; the respiratory volume (V) was computed from the integral of \( \dot{V} \); and P = P aw for estimates of Ers and R rs or P = (P aw − P es) for estimates of E L and R L [31].
Tidal recruitment and hyperinflation were assessed through estimation of the stress index [23]. This index was computed by fitting the patient’s P aw versus time (t) curve with the power equation P aw(t) = at bi + c, where t i was the time from the beginning of the constant flow inspiration, and a, b, and c were constants. The coefficient b (stress index) describes the shape of the P aw–t curve: b = 1, straight curve (constant compliance during lung inflation, minimal stress); b < 1, progressive decrease in slope (increasing compliance during lung inflation, tidal recruitment with low-volume stress); and b > 1, progressive increase in slope (decreasing compliance during lung inflation, tidal hyperinflation with high-volume stress). Quality of fitting was assessed with the coefficient of determination (R 2). One-minute epochs were analyzed using the Levenberg–Marquardt method (Mecanica, built in Matlab®, The MathWorks, Inc., Natick, MA). A respiratory cycle was discarded if (1) a constant inspiratory flow portion was not present, (2) the constant flow period was less than one third of the inspiratory time, and (3) R 2 < 0.95.
Exhaled Nitric Oxide
eNO was measured continuously by chemiluminescence (Sievers model NOA 280; Sievers Instruments, Boulder, CO) with response time of 170 ms [32]. The analyzer was calibrated before each case with 0 and 45 ppm NO. The eNO signal was either digitized at 100 Hz or registered on paper. Gas was sampled at a rate of 250 ml/min through a Teflon tube connected to the Y-piece of the breathing circuit. Measurements of inspired NO were always less than 2 ppb. eNO was measured as the mean end-expiratory value of at least five breathing cycles. The mean values were taken from the point corresponding to the plateau of the end exhaled CO2 reading, representing the lower respiratory tract sample.
Statistics
All results are expressed as the mean ± standard deviation (SD) or as median [interquartile range]. We based the sample size calculation on expected shunt and eNO differences between groups, and in the same group from baseline to end of surgery. For shunt, a difference of 8% between at least two of the three groups with SD = 5.5% and a change from baseline to end of surgery of 6% were used. For eNO, values as observed in normals [33] and COPD exacerbation [34] were applied, as well as a within-group (pairwise) expected change in eNO of 4 ppb with a SD = 6 ppb. An ANOVA-based power analysis for a power of 0.80 (p < 0.05) and equal variance led to a minimum sample size of 8 patients per group. Repeated-measures ANOVA with between-subjects factors were used to compare time points and groups. Post-hoc comparisons were performed with the Sidak correction for multiple comparisons. A linear correlation coefficient was used for computation of correlations. χ2 analysis was used to compare proportions. Analysis was performed using SAS statistical software ver. 9 (SAS Institute Inc., Cary, NC). Two-tailed values of p < 0.05 were used to establish statistical significance.
Results
Demographic characteristics were similar in all groups (Table 1). Hemodynamics showed higher central venous pressures in both COPD groups and higher pulmonary artery pressures in COPD on-pump than controls at baseline (Table 2). The increased heart rate after chest closure was due to pacing.
Respiratory Mechanics
R rs in the on-pump COPD group was larger than in controls at all time points (Fig. 1a). Following sternotomy, R rs was significantly decreased in both COPD groups. In all groups, R rs significantly increased after chest closure, returning to values similar to baseline.
Respiratory system resistance and elastance for the three studied groups at four surgical time points. Data are presented (1) following intubation, before sternotomy (Baseline); (2) after sternotomy, before revascularization (Pre-revasc); (3) before chest closure, following revascularization (Post-revasc, i.e., following cardiopulmonary bypass for control and COPD on-pump groups); and (4) after chest closure, at the end of the procedure (Closed chest). a Patients with chronic obstructive pulmonary disease (COPD) had higher resistance than controls throughout the whole intraoperative period (p < 0.05). The resistance decreased in the COPD groups after opening the chest and increased in all groups following chest closure. b There was an increase in elastance after chest closure, more marked for the control group. Values are mean ± standard deviation. *p < 0.05; †p < 0.01
Patients in the control and COPD off-pump groups showed a significant increase in E rs at the end of surgery (Fig. 1b). The increase in E rs relative to baseline was larger in controls than in the COPD groups.
The partitioning of the respiratory system mechanics into lung and chest wall components showed that most of the changes in respiratory system mechanics were due to changes in lung properties. E rs had a high correlation (r = 0.80, p < 0.0001) with E L, and R rs with R L (r = 0.97, p < 0.0001).
The stress index was similar for all groups at baseline. Values were under 1 (=tidal recruitment, low-volume stress) for most measurement points (Fig. 2). In fact, the stress index was under 0.8 (associated with computed tomography findings of tidal recruitment) for 35% of measurements in the on-pump COPD group, 19% in the control group, and 31% in the off-pump COPD group. During open chest conditions in on-pump cases, COPD patients tended to have stress indices below 0.9 (related to histological and inflammatory changes in experimental ventilator-induced lung injury) more frequently than controls (p < 0.1), with 6 of 12 COPD patients having stress indices under 0.9 before CPB and 5 of those 12 after CPB, whereas 1 of 8 control patients had a stress index in that range for the same time points. When all patients were pooled, chest opening led to a significant decrease in the number of stress indices under 1 (p < 0.05), and chest closure had the reverse effect (p < 0.001). In specific groups, the stress index increased after chest opening in the COPD off-pump group and decreased after chest closure in the control and COPD off-pump groups. Measurements at the end of surgery were not significantly different from those at baseline.
Individual measurements of stress indices in the three studied groups at the four surgical time points. The majority of measurements for all groups were below 1, a range compatible with tidal recruitment of alveoli and small airways. A significant percentage of the measurements were under 0.8 and few were above 1.2. There was a significant reduction in the stress index after chest closure in the control and off-pump chronic obstructive pulmonary disease (COPD) groups. Dashes indicate mean values for each group and time point. Time points are described in Fig. 1. *p < 0.05; †p < 0.01
Exhaled NO
eNO was lower at the end of surgery than at baseline for patients undergoing CPB in the control and COPD on-pump groups (Fig. 3). In fact, eNO was already reduced during open chest conditions from before to after CPB in controls (29%, p = 0.04) and on-pump COPD patients (26%, p = 0.01). There was a high correlation between mean eNO before and after sternotomy (r = 0.92, p < 0.001) and before and after chest closure (r = 0.93, p < 0.001), and no change in mean eNO within groups was observed following opening or closure of the chest. Absolute and percent changes in eNO were not correlated to corresponding changes in E rs, R rs, PaO2, or PaCO2 (p = NS for all correlations). The COPD off-pump group had significantly lower eNO than controls at baseline and these did not change at the end of surgery.
Exhaled nitric oxide for the three studied groups at four surgical time points. Exhaled nitric oxide decreased from Baseline to Closed Chest and from before to after revascularization, i.e., cardiopulmonary bypass, in the control and the chronic obstructive pulmonary disease (COPD) on-pump groups. Time points are described in Fig. 1. Values are mean ± standard deviation. *p < 0.05; †p < 0.01
Gas Exchange
Mean PaO2 decreased in all groups at the end of surgery: 51% in controls, 26% in COPD on-pump, and 30% in COPD off-pump patients (Table 2). Right-to-left shunt was similar at baseline for all groups in the patients mechanically ventilated with 100% O2 (Fig. 4). Shunt in controls increased from 19 to 26% from baseline to end of surgery and was larger than that in the COPD on-pump group after chest closure. In contrast, shunt was not significantly changed in COPD patients (Fig. 4). An increase in shunt in controls was already observed in open chest conditions following revascularization.
Right-to-left shunt for the three studied groups at four surgical time points. There was significant increase in shunt in the control group after cardiopulmonary bypass and chest closure, but no significant changes in patients with chronic obstructive pulmonary disease (COPD). Time points are described in Fig. 1. Values are mean ± standard deviation. *p < 0.05; †p < 0.01
Despite the high alveolar-arterial gradient of O2 (AaDO2) in controls at arrival in the intensive care unit (ICU) (328 mmHg), consistent with the higher shunts in controls at the end of surgery, the improvement in AaDO2 per hour until extubation tended to be faster in controls than in on-pump COPD patients (p = 0.08, Fig. 5), a trend confirmed when all COPD patients were included (p < 0.05, Fig. 5). This paralleled the trend for shorter time to extubation in the control group and the longer ICU stay in COPD on-pump patients (Table 1).
Change rates of the alveolar-arterial PaO2 (AaDO2) gradients in mmHg/h for the three studied groups following admission to the intensive care unit. The control group tends to have more negative values than the chronic obstructive pulmonary disease (COPD) groups, representing a faster reduction in AaDO2 following surgery. AaDO2 change rates were also significantly smaller for controls than for the combined COPD groups (p < 0.05). Dashes indicate mean values for each group. §p = 0.08
Discussion
The main findings of this study were as follows: (1) Intraoperative respiratory mechanics in patients with and without COPD undergoing CABG surgery is more frequently consistent with tidal recruitment of alveoli and/or small airways than with hyperinflation when commonly used ventilatory settings are applied. In open chest conditions, tidal recruitment tended to be more marked in COPD patients. (2) eNO is reduced after on-pump CABG in patients with and without COPD, compatible with small airway injury. (3) Moderate-COPD patients appear to be less susceptible to development of shunt immediately after CPB than controls.
Pulmonary complications, including acute lung injury, are important factors in lung morbidity during and after cardiac surgery [35, 36]. In fact, it has been suggested that CPB leads to greater pulmonary than systemic inflammatory response [37]. When ARDS occurs after CPB (<2%), the associated mortality is high (>50%) [13]. After CABG surgery, early extubation failure was reported in 35–40% of patients [15, 38], and hypoxemia was implicated as the most common cause for prolonged mechanical ventilation (>24 h) occurring in 9% of the patients [15]. COPD is associated with increased risk for major morbidity and mortality after cardiac surgery [3–7, 39]. Patients with COPD present a differential and magnified inflammatory response during cardiac surgery, with likely both at the systemic and pulmonary level [16, 17]. At least part of the pulmonary inflammatory response during cardiac surgery could be related to cyclic recruitment or lung hyperinflation, given that lung protective strategies using higher PEEP and lower tidal volumes reduced the inflammatory response following CPB [10, 11]. Atelectasis is an important perioperative pathogenic factor [40] and is frequently present during cardiac surgery [18, 19]. Thus, understanding of the respiratory dysfunction in patients with and without COPD can be important to minimize perioperative respiratory morbidity.
Respiratory Mechanics and Gas Exchange
Our results indicate that lungs of CABG surgery patients with or without COPD frequently undergo tidal recruitment intraoperatively. Stress indices were mostly under 1.0 throughout surgery. A value under 0.8 corresponded in previous studies to the initial low-volume nonlinear portion of their lungs’ pressure–volume curve and to computed tomography findings of tidal recruitment in experimental models of healthy [24] and surfactant-depleted lungs [23, 24]. A value under 0.9 best discriminated experimental histological and inflammatory evidence of ventilator-induced lung injury [41]. A significant percentage of our measurements were under those values, with a trend for a larger percentage in COPD patients during open chest conditions. Thus, our findings suggest that the studied patients were frequently at increased risk for ventilator-associated lung injury.
Our results are compatible with those of former studies that showed less inflammatory response in cardiac surgery when protective modes of ventilation were used [10, 11]. We expand those former findings by suggesting that the effect of those protective modes was likely due to their effects on low-volume stress. Thus, our observations emphasize the importance of ventilation strategies that include the prevention of low-volume injury, such as the use of PEEP, to reduce perioperative lung damage during CABG surgery. Considering the ongoing discussion on “open lung” versus “lung rest” mechanical ventilatory strategies [42], our observations suggest a potential benefit of open lung approaches and justify conducting clinical studies to address minimization of low-volume lung injury during cardiac surgery. This could be particularly important in patients at increased risk for lung injury such as those subject to significant blood transfusion. Finally, we also observed a sizable variability in respiratory parameters in the different patient groups. This indicates that availability of bedside measurements such as the stress index or the more sophisticated electrical impedance tomography could, in the future, facilitate the titration of ventilatory parameters to individual patients [43].
In contrast to the relatively unchanged stress index in on-pump COPD patients from before to after revascularization, there was a significant increase in stress index in the off-pump COPD patients. Overall, average changes in the stress indices between those time points were within the 0.9–1.1 range, i.e., a range within normal values reported in previous studies [41]. Those observed differences likely characterize the mechanical response of the COPD lung to the very distinct set of intraoperative conditions occurring between those two time points: Whereas the on-pump COPD lungs were exposed to the acute inflammatory response to CPB and an average of 102 min of passive lung deflation, the off-pump COPD group was continuously ventilated and not subjected to the inflammatory response to CPB. The correlations of the changes in the stress index and the respiratory mechanics and shunt provide insight on the potential causes for the observations. In the on-pump COPD group, there was a significant correlation between the ratio of the stress index after to before revascularization and the shunt ratio (r = 0.61, p < 0.05), suggesting that changes in stress index were predominantly influenced by lung collapse. In contrast, for the off-pump group the stress index ratio was inversely correlated to the R rs ratio at the same time points (r = −0.90, p < 0.005). The larger the R rs reduction after revascularization, the more inflated the lung conditions. In the patients not subjected to CPB, continuous mechanical ventilation with an open chest could have facilitated progressive airway expansion, with recruitment of collapsed areas and shifting to a more inflated condition of the COPD lung. Controls had an average but nonsignificant increase in the stress index after revascularization. Interestingly, in controls, also exposed to CPB, the stress index ratio correlated with the shunt ratio (r = 0.74, p < 0.05) and tended to correlate with the R rs ratio (r = −0.66, p < 0.08). This could indicate a combination of effects, including increased lung collapsibility associated with CPB and R rs contribution leading to more lung inflation as R rs decreased. Redistribution of regional lung aeration probably occurs in the studied cases and leads to complex effects on the stress index [24]. Studies using measurements of regional perfusion and aeration will be required to provide an accurate explanation for these respiratory mechanics and associated gas exchange findings.
Increases in E rs and R rs during CABG have been described [44, 45]. Less is known about perioperative lung function in specific groups, a relevant point since distinct mechanisms of respiratory dysfunction can imply different management strategies. Baseline measurements of E rs and R rs were consistent with those of previous studies [44, 45], with R rs in COPD patients larger than that in controls. R rs did not increase in COPD patients and controls after CPB, in contrast to most [45, 46] but not all [44] studies.
While COPD patients did not show significant intraoperative worsening of R rs, they had significantly slower improvement in oxygenation in the ICU than controls, indicating a limited capacity to recover postoperatively, which is compatible with their higher risk for complications [3, 6] and their observed longer time to extubation and ICU stay [3, 4, 47]. Such observations may be at least partially explained by the role of absorption atelectasis as the main determinant of AaDO2 in controls. Such regions of derecruited lung would be progressively reduced in the ICU as PEEP and FIO2 < 100% were applied. In contrast, the major determinant of AaDO2 in COPD patients is ventilation-perfusion mismatch associated with the severity of emphysema and small airway and vascular abnormalities, potentially exacerbated perioperatively [48–50]. Indeed, COPD patients have a differential inflammatory response during cardiac surgery with increased release of cysteinyl leukotrienes [16]. This could add to the potential small airway dysfunction discussed above. Additionally, inhibition of the hypoxic pulmonary vasoconstriction due to inflammatory mediators and vasoactive medications [51–53] could contribute to perfusion heterogeneity. Such factors could have combined with the chronic inflammation [54] and lung dysfunction [49, 50] during COPD to produce the trend toward slower improvement in oxygenation observed in our COPD patients.
E rs increased significantly in controls after chest closure, which is consistent with previous studies [44–46]. Shunt increased concurrently in controls, suggesting that at least part of the derecruited lung remained perfused. In contrast, E rs did not increase significantly in the COPD on-pump group. This indicates that the process of perioperative lung derecruitment in moderate COPD patients differs from that in controls. Patients with healthy lungs typically present perioperative atelectasis and shunt [40, 55]. In contrast, Gunnarson et al. [56] observed increased ventilation-perfusion mismatch but no increase in shunt (mean 1%) in COPD patients during enflurane anesthesia. These patients had minor or no atelectasis on computed tomography and minimal reduction of chest dimensions, suggesting minimally affected functional residual capacity [56]. These findings are consistent with the resistance of spontaneously breathing nonintubated COPD patients to develop oxygen absorption atelectasis [49, 56], thought to be additionally associated with increased collateral ventilation, and their more homogeneous vertical distribution of density and ventilation [50]. Our findings expand those observations by suggesting that this reduced propensity to lung derecruitment is also present in intubated, mechanically ventilated COPD patients undergoing cardiac surgery. Thus, the presence of airway obstruction and prolonged expiratory time constants found in COPD, generating a potentially protective auto-PEEP effect, combined with the reduced elastic recoil limiting the perioperative reduction of functional residual capacity likely contributed to the observed maintenance of lung elastance.
Changes in E rs and R rs were smaller than previously reported [44, 45]. A possible explanation is the relatively small number of patients in the studies, with differences due to distinct patient samples and the fact that previous studies did not stratify patients according to their initial pulmonary function. Since the studies were performed years ago, our findings may also represent management improvements such as biocompatibility of the CPB system and cardiac protection techniques resulting in less lung dysfunction.
Exhaled Nitric Oxide
There is limited information on eNO in intubated COPD patients. We found similar baseline eNO in on-pump COPD and control groups, consistent with measurements in nonintubated stable COPD patients and controls [34, 57], but in contrast with increased eNO observed in stable COPD by others [58]. Such discrepancies may be explained by differences in COPD classification, smoking history [58], eNO assessment methods, and use of steroids.
eNO was reduced after on-pump CABG in subjects with and without COPD. This is compatible with observations of decreased eNO induced by CPB in CABG surgery [25, 59, 60]. D’Angelo et al. [21, 27] found a significant relationship between the decrease in eNO and bronchiolar epithelial damage in an experimental model of low-volume lung injury and proposed the use of eNO reduction as a sign of peripheral airway injury. Reduced eNO has also been suggested as reflective of bronchial epithelial dysfunction after hypoxia and reoxygenation on CPB [61]. Low levels of eNO have been associated with lung damage in other conditions such as with impaired function in cystic fibrosis [62] and different forms of smoke inhalation [63–65]. Thus, our findings of reduced eNO after CPB and of a stress index under 0.8 in a significant percentage of patients could suggest decreased endogenous production and/or elimination due to injury to the airway epithelium. This could have resulted from tidal opening–closing of small airways, in addition to perioperative ischemia–reperfusion associated with cardiac surgery [21, 27]. Given that many other factors influence eNO changes [25, 27, 60, 66–68], further studies will be required to clarify the causes of reduced perioperative eNO in patients with and without COPD.
Finally, it is apparent that eNO did not reflect exclusively pulmonary injury. Although reduced after on-pump CABG, eNO was not correlated to any variable related to pulmonary dysfunction. Indeed, whereas eNO changes were similar in on-pump COPD patients and controls, respiratory mechanics and gas exchange were distinct. This is also consistent with the dissociation between lung function and inflammatory markers in COPD outpatients [69]. Consequently, our results suggest that in the intraoperative period of CABG surgery, eNO is not an accurate predictor of acute lung injury.
This study has several limitations. Clinical COPD is significantly heterogeneous. Thus, the limited number of patients in our study does not allow for generalization of our results to all subsets of COPD patients. Computation of the stress index in COPD patients may be influenced by the volume dependence of their airway resistance, which decreases during inspiration [70]. This could result in a downward concavity in the pressure–time curve and lead to overestimation of tidal recruitment. Our analysis of eNO is a significant simplification compared to compartmental models that address airway and alveolar contributions to eNO [71]. Future studies will be necessary to establish whether the similar perioperative changes in eNO in controls and COPD patients are distinct at the compartmental level.
In conclusion, intraoperative respiratory mechanics during CABG surgery were compatible with tidal alveolar recruitment during CABG surgery in patients with and without COPD and are suggestive of risk for ventilator-associated lung injury. Strategies to limit low-volume injury during mechanical ventilation may be particularly relevant in these patients. Changes in respiratory function in the perioperative period showed greater susceptibility to lung derecruitment in controls, with worsening of elastance and development of shunt. Controls and patients with moderate COPD showed an equivalent and significant decrease in eNO after CABG surgery, which is compatible with small-airway injury and likely has a multifactorial mechanism. The decrease in eNO was not uniquely related to perioperative respiratory dysfunction.
References
Leavitt BJ, Ross CS, Spence B, Surgenor SD, Olmstead EM, Clough RA, Charlesworth DC, Kramer RS, O’Connor GT, Northern New England Cardiovascular Disease Study Group (2006) Long-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation 114(1 Suppl):I430–I434
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J, American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2011) Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 123(4):e18–e209
Rady MY, Ryan T (1999) Perioperative predictors of extubation failure and the effect on clinical outcome after cardiac surgery. Crit Care Med 27:340–347
De Santo LS, Bancone C, Santarpino G, Romano G, Della Corte A, Vicchio M, De Pietro A, Galdieri N, Cotrufo M (2009) Noninvasive positive-pressure ventilation for extubation failure after cardiac surgery: pilot safety evaluation. J Thorac Cardiovasc Surg 137:342–346
Soliman Hamad MA, van Straten AH, van Zundert AA, ter Woorst JF, Martens EJ, Penn OC (2011) Preoperative prediction of early mortality in patients with low ejection fraction undergoing coronary artery bypass grafting. J Card Surg 26:9–15
Akins CW, Daggett WM, Vlahakes GJ, Hilgenberg AD, Torchiana DF, Madsen JC, Buckley MJ (1997) Cardiac operations in patients 80 years old and older. Ann Thorac Surg 64:606–614
Ried M, Unger P, Puehler T, Haneya A, Schmid C, Diez C (2010) Mild-to-moderate COPD as a risk factor for increased 30-day mortality in cardiac surgery. Thorac Cardiovasc Surg 7:387–391
Laffey JG, Boylan JF, Cheng DC (2002) The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiology 97:215–252
Pepe PE, Marini JJ (1982) Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction: the auto-PEEP effect. Am Rev Respir Dis 126:166–170
Zupancich E, Paparella D, Turani F, Munch C, Rossi A, Massaccesi S, Ranieri VM (2005) Mechanical ventilation affects inflammatory mediators in patients undergoing cardiopulmonary bypass for cardiac surgery: a randomized clinical trial. J Thorac Cardiovasc Surg 130:378–383
Reis Miranda D, Gommers D, Struijs A, Dekker R, Mekel J, Feelders R, Lachmann B, Bogers AJ (2005) Ventilation according to the open lung concept attenuates pulmonary inflammatory response in cardiac surgery. Eur J Cardiothorac Surg 28:889–895
Sundar S, Novack V, Jervis K, Bender SP, Lerner A, Panzica P, Mahmood F, Malhotra A, Talmor D (2011) Influence of low tidal volume ventilation on time to extubation in cardiac surgical patients. Anesthesiology 114(5):1102–1110
Ng CS, Wan S, Yim AP, Arifi AA (2002) Pulmonary dysfunction after cardiac surgery. Chest 121:1269–1277
Weiss YG, Merin G, Koganov E, Ribo A, Oppenheim-Eden A, Medalion B, Peruanski M, Reider E, Bar-Ziv J, Hanson WC, Pizov R (2000) Postcardiopulmonary bypass hypoxemia: a prospective study on incidence, risk factors, and clinical significance. J Cardiothorac Vasc Anesth 14:506–513
Yende S, Wunderink R (2002) Causes of prolonged mechanical ventilation after coronary artery bypass surgery. Chest 122:245–252
de Prost N, El-Karak C, Avila M, Ichinose F, Vidal Melo MF (2011) Changes in cysteinyl leukotrienes during and after cardiac surgery with cardiopulmonary bypass in patients with and without chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg 141:1496–1502
Onorati F, Santini F, Mariscalco G, Bertolini P, Sala A, Faggian G, Mazzucco A (2011) Leukocyte filtration ameliorates the inflammatory response in patients with mild to moderate lung dysfunction. Ann Thorac Surg 92:111–121
Verheij J, van Lingen A, Raijmakers PG, Spijkstra JJ, Girbes AR, Jansen EK, van den Berg FG, Groeneveld AB (2005) Pulmonary abnormalities after cardiac surgery are better explained by atelectasis than by increased permeability oedema. Acta Anaesthesiol Scand 49:1302–1310
Hachenberg T, Tenling A, Nystrom SO, Tyden H, Hedenstierna G (1994) Ventilation-perfusion inequality in patients undergoing cardiac surgery. Anesthesiology 80:509–519
Mead J, Takishima T, Leith D (1970) Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 28:596–608
D’Angelo E, Koulouris NG, Della Valle P, Gentile G, Pecchiari M (2008) The fall in exhaled nitric oxide with ventilation at low lung volumes in rabbits: an index of small airway injury. Respir Physiol Neurobiol 160:215–223
Otto CM, Markstaller K, Kajikawa O, Karmrodt J, Syring RS, Pfeiffer B, Good VP, Frevert CW, Baumgardner JE (2008) Spatial and temporal heterogeneity of ventilator-associated lung injury after surfactant depletion. J Appl Physiol 104:1485–1494
Grasso S, Terragni P, Mascia L, Fanelli V, Quintel M, Herrmann P, Hedenstierna G, Slutsky AS, Ranieri VM (2004) Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med 32:1018–1027
Carvalho AR, Spieth PM, Pelosi P, Vidal Melo MF, Koch T, Jandre FC, Giannella-Neto A, de Abreu MG (2008) Ability of dynamic airway pressure curve profile and elastance for positive end-expiratory pressure titration. Intensive Care Med 34:2291–2299
Cuthbertson BH, Stott SA, Webster NR (2002) Exhaled nitric oxide as a marker of lung injury in coronary artery bypass surgery. Br J Anaesth 89:247–250
Marczin N, Kovesi T, Royston D (2003) Exhaled nitric oxide as a marker of lung injury in coronary artery bypass surgery. Br J Anaesth 90:101–104
D’Angelo E, Pecchiari M, Della Valle P, Koutsoukou A, Milic-Emili J (2005) Effects of mechanical ventilation at low lung volume on respiratory mechanics and nitric oxide exhalation in normal rabbits. J Appl Physiol 99:433–444
Agusti AG, Villaverde JM, Togores B, Bosch M (1999) Serial measurements of exhaled nitric oxide during exacerbations of chronic obstructive pulmonary disease. Eur Respir J 14:523–528
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J, Global Initiative for Chronic Obstructive Lung Disease (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176:532–555
Berggren S (1942) The oxygen deficit of arterial blood caused by nonventilating parts of the lung. Acta Physiol Scand 11:1–92
Dechman GS, Chartrand DA, Ruiz-Neto PP, Bates JH (1995) The effect of changing end-expiratory pressure on respiratory system mechanics in open- and closed-chest anesthetized, paralyzed patients. Anesth Analg 81:279–286
Imanaka H, Hess D, Kirmse M, Bigatello LM, Kacmarek RM, Steudel W, Hurford WE (1997) Inaccuracies of nitric oxide delivery systems during adult mechanical ventilation. Anesthesiology 86:676–688
Balint B, Kharitonov SA, Hanazawa T, Donnelly LE, Shah PL, Hodson ME, Barnes PJ (2001) Increased nitrotyrosine in exhaled breath condensate in cystic fibrosis. Eur Respir J 17:1201–1207
Maziak W, Loukides S, Culpitt S, Sullivan P, Kharitonov SA, Barnes PJ (1998) Exhaled nitric oxide in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157:998–1002
Fernandez-Perez ER, Sprung J, Afessa B, Warner DO, Vachon CM, Schroeder DR, Brown DR, Hubmayr RD, Gajic O (2009) Intraoperative ventilator settings and acute lung injury after elective surgery: a nested case control study. Thorax 64:121–127
Moller CH, Perko MJ, Lund JT, Andersen LW, Kelbaek H, Madsen JK, Winkel P, Gluud C, Steinbruchel DA (2010) No major differences in 30-day outcomes in high-risk patients randomized to off-pump versus on-pump coronary bypass surgery: the best bypass surgery trial. Circulation 121:498–504
Kotani N, Hashimoto H, Sessler DI, Muraoka M, Wang JS, O’Connor MF, Matsuki A (2000) Cardiopulmonary bypass produces greater pulmonary than systemic proinflammatory cytokines. Anesth Analg 90:1039–1045
Serrano N, Garcia C, Villegas J, Huidobro S, Henry CC, Santacreu R, Mora ML, Epidemiological Project for ICU Research, Evaluation (EPICURE) (2005) Prolonged intubation rates after coronary artery bypass surgery and ICU risk stratification score. Chest 128:595–601
Di Eusanio M, Fortuna D, De Palma R, Dell’Amore A, Lamarra M, Contini GA, Gherli T, Gabbieri D, Ghidoni I, Cristell D, Zussa C, Pigini F, Pugliese P, Pacini D, Di Bartolomeo R (2011) Aortic valve replacement: results and predictors of mortality from a contemporary series of 2256 patients. J Thorac Cardiovasc Surg 141:940–947
Duggan M, Kavanagh BP (2005) Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology 102:838–854
Ranieri VM, Zhang H, Mascia L, Aubin M, Lin CY, Mullen JB, Grasso S, Binnie M, Volgyesi GA, Eng P, Slutsky AS (2000) Pressure-time curve predicts minimally injurious ventilatory strategy in an isolated rat lung model. Anesthesiology 93:1320–1328
Fanelli V, Mascia L, Puntorieri V, Assenzio B, Elia V, Fornaro G, Martin EL, Bosco M, Delsedime L, Fiore T, Grasso S, Ranieri VM (2009) Pulmonary atelectasis during low stretch ventilation: “open lung” versus “lung rest” strategy. Crit Care Med 37:1046–1053
Schultz MJ, Haitsma JJ (2008) How to detect tidal recruitment and/or alveolar hyperinflation—computed tomography, electrical impedance tomography, or stress index? Crit Care Med 36:1020–1021
Auler JO Jr, Zin WA, Caldeira MP, Cardoso WV, Saldiva PH (1987) Pre- and postoperative inspiratory mechanics in ischemic and valvular heart disease. Chest 92:984–990
Babik B, Asztalos T, Petak F, Deak ZI, Hantos Z (2003) Changes in respiratory mechanics during cardiac surgery. Anesth Analg 96:1280–1287
Barnas GM, Watson RJ, Green MD, Sequeira AJ, Gilbert TB, Kent J, Villamater E (1994) Lung and chest wall mechanical properties before and after cardiac surgery with cardiopulmonary bypass. J Appl Physiol 76:166–175
Guler M, Kirali K, Toker ME, Bozbuga N, Omeroglu SN, Akinci E, Yakut C (2001) Different CABG methods in patients with chronic obstructive pulmonary disease. Ann Thorac Surg 71:152–157
Barbera JA, Ramirez J, Roca J, Wagner PD, Sanchez-Lloret J, Rodriguez-Roisin R (1990) Lung structure and gas exchange in mild chronic obstructive pulmonary disease. Am Rev Respir Dis 141:895–901
Wagner PD, Dantzker DR, Dueck R, Clausen JL, West JB (1977) Ventilation-perfusion inequality in chronic obstructive pulmonary disease. J Clin Invest 59:203–216
Vidal Melo MF, Winkler T, Harris RS, Musch G, Greene RE, Venegas JG (2010) Spatial heterogeneity of lung perfusion assessed with (13)N PET as a vascular biomarker in chronic obstructive pulmonary disease. J Nucl Med 51:57–65
Melot C, Naeije R, Rothschild T, Mertens P, Mols P, Hallemans R (1983) Improvement in ventilation-perfusion matching by almitrine in COPD. Chest 83:528–533
Agusti AG, Barbera JA, Roca J, Wagner PD, Guitart R, Rodriguez-Roisin R (1990) Hypoxic pulmonary vasoconstriction and gas exchange during exercise in chronic obstructive pulmonary disease. Chest 97:268–275
Tenling A, Hachenberg T, Tyden H, Wegenius G, Hedenstierna G (1998) Atelectasis and gas exchange after cardiac surgery. Anesthesiology 89:371–378
Saetta M (1999) Airway inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 160:S17–S20
Tokics L, Hedenstierna G, Strandberg A, Brismar B, Lundquist H (1987) Lung collapse and gas exchange during general anesthesia: effects of spontaneous breathing, muscle paralysis, and positive end-expiratory pressure. Anesthesiology 66:157–167
Gunnarsson L, Tokics L, Lundquist H, Brismar B, Strandberg A, Berg B, Hedenstierna G (1991) Chronic obstructive pulmonary disease and anaesthesia: formation of atelectasis and gas exchange impairment. Eur Respir J 4:1106–1116
Robbins RA, Floreani AA, Von Essen SG, Sisson JH, Hill GE, Rubinstein I, Townley RG (1996) Measurement of exhaled nitric oxide by three different techniques. Am J Respir Crit Care Med 153:1631–1635
Corradi M, Majori M, Cacciani GC, Consigli GF, de’Munari E, Pesci A (1999) Increased exhaled nitric oxide in patients with stable chronic obstructive pulmonary disease. Thorax 54:572–575
Ishibe Y, Liu R, Hirosawa J, Kawamura K, Yamasaki K, Saito N (2000) Exhaled nitric oxide level decreases after cardiopulmonary bypass in adult patients. Crit Care Med 28:3823–3827
Beghetti M, Silkoff PE, Caramori M, Holtby HM, Slutsky AS, Adatia I (1998) Decreased exhaled nitric oxide may be a marker of cardiopulmonary bypass-induced injury. Ann Thorac Surg 66:532–534
Pearl JM, Nelson DP, Wellmann SA, Raake JL, Wagner CJ, McNamara JL, Duffy JY (2000) Acute hypoxia and reoxygenation impairs exhaled nitric oxide release and pulmonary mechanics. J Thorac Cardiovasc Surg 119:931–938
Keen C, Gustafsson P, Lindblad A, Wennergren G, Olin AC (2010) Low levels of exhaled nitric oxide are associated with impaired lung function in cystic fibrosis. Pediatr Pulmonol 45:241–248
Kharitonov SA, Robbins RA, Yates D, Keatings V, Barnes PJ (1995) Acute and chronic effects of cigarette smoking on exhaled nitric oxide. Am J Respir Crit Care Med 152:609–612
Schilling J, Holzer P, Guggenbach M, Gyurech D, Marathia K, Geroulanos S (1994) Reduced endogenous nitric oxide in the exhaled air of smokers and hypertensives. Eur Respir J 7:467–471
Yates DH, Breen H, Thomas PS (2001) Passive smoke inhalation decreases exhaled nitric oxide in normal subjects. Am J Respir Crit Care Med 164:1043–1046
Kharitonov SA, Sapienza MM, Chung KF, Barnes PJ (1999) Prostaglandins mediate bradykinin-induced reduction of exhaled nitric oxide in asthma. Eur Respir J 14:1023–1027
Kovesi T, Royston D, Yacoub M, Marczin N (2003) Basal and nitroglycerin-induced exhaled nitric oxide before and after cardiac surgery with cardiopulmonary bypass. Br J Anaesth 90:608–616
Hyde RW, Geigel EJ, Olszowka AJ, Krasney JA, Forster RE 2nd, Utell MJ, Frampton MW (1997) Determination of production of nitric oxide by lower airways of humans-theory. J Appl Physiol 82:1290–1296
Lapperre TS, Snoeck-Stroband JB, Gosman MM, Stolk J, Sont JK, Jansen DF, Kerstjens HA, Postma DS, Sterk PJ, Groningen and Leiden Universities Corticosteroids in Obstructive Lung Disease Study Group (2004) Dissociation of lung function and airway inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 170:499–504
Butler J, Caro CG, Alcala R, Dubois AB (1960) Physiological factors affecting airway resistance in normal subjects and in patients with obstructive respiratory disease. J Clin Invest 39:584–591
Condorelli P, Shin HW, Aledia AS, Silkoff PE, George SC (2007) A simple technique to characterize proximal and peripheral nitric oxide exchange using constant flow exhalations and an axial diffusion model. J Appl Physiol 102:417–425
Acknowledgments
The authors acknowledge Dr. Hui Zheng for reviewing the statistical analysis, and RNs Michelle Curran Cereno, Laura Collier, Cindy Cooney, Rosemary Daggett, Adrianne Diamond, Valerie Buckley, Danielle Faldetta, Barbara Hill, Jennifer Mills, Karen Parmenter, Joann Pellegrino, Valery Petit-Ton, Christine Tetrault Angelini, Sharon Zisk who helped with the intraoperative measurements and blood samples.
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carvalho, A.R., Ichinose, F., Schettino, I.A. et al. Tidal Lung Recruitment and Exhaled Nitric Oxide During Coronary Artery Bypass Grafting in Patients With and Without Chronic Obstructive Pulmonary Disease. Lung 189, 499–509 (2011). https://doi.org/10.1007/s00408-011-9325-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-011-9325-0