Abstract
There have been contradictory reports suggesting that CO2 may constrict, dilate, or have no effect on pulmonary vessels. Permissive hypercapnia has become a widely adopted ventilatory technique used to avoid ventilator-induced lung injury, particularly in patients with acute respiratory distress syndrome (ARDS). On the other hand, respiratory alkalosis produced by mechanically induced hyperventilation is the mainstay of treatment for newborn infants with persistent pulmonary hypertension. It is important to clarify the vasomotor effect of CO2 on pulmonary circulation in order to better evaluate the strategies of mechanical ventilation in intensive care. In the present study, pulmonary vascular responses to CO2 were observed in isolated rat lungs (n = 32) under different levels of pulmonary arterial pressure (PAP) induced by various doses of endothelin-1 (ET-1). The purposes of this study were to investigate (1) the vasodilatory effect of 5% CO2 in either N2 (hypoxic-hypercapnia) or air (normoxic-hypercapnia) at different PAP levels induced by various doses of endothelin-1, and (2) the role of nitric oxide (NO) in mediating the pulmonary vascular response to hypercapnia, hypoxia, and ET-1. The results indicated that (1) CO2 produces pulmonary vasodilatation at high PAP under ET-1 and hypoxic vasoconstriction; (2) the vasodilatory effect of CO2 at different pressure levels varies in accordance with the levels of PAP, the dilatory effect tends to be more evident at higher PAP; and (3) endogenous NO attenuates ET-1 and hypoxic pulmonary vasoconstriction but does not augment the CO2-induced vasodilatation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Permissive hypercapnia with a small tidal volume has become a widely adapted ventilatory technique used to avoid ventilator-induced lung injury in patients with lung injury or acute respiratory distress syndrome (ARDS). Such “protective” ventilator strategies minimize lung stretch and patient mortality but often lead to an elevation in PaCO2. However, the current concepts clearly recognize an independent protective effect of elevated CO2 tension in experimental models of lung injury.
The effect of CO2 on pulmonary vascular tone is controversial, with evidence of both vasoconstriction and vasodilatation effects. Previous investigations have shown that high CO2 tension with elevated hydrogen ion concentration in the blood increases the extracellular Ca2+ influx which accounts for the vasoconstriction property of CO2 in the pulmonary circulation [1–3]. Nonetheless, CO2 also plays a vasodilator role under the condition of high vascular tone, and such a vasodilatory effect is related to the concentration of inhaled CO2, not to the blood pH value [4–6]. Other lines of evidence have also indicated that CO2 may attenuate vasoconstriction induced by drugs or hypoxia [7–10]. More recently, studies have supported the evidence that hypercapnic acidosis attenuates ischemia-reperfusion, endotoxin, and ventilator-induced lung injuries in several animal models [11–15]. The potential beneficial effects of therapeutic hypercapnia by direct improvement of gas exchange and anti-inflammatory events have also been reported in several studies [16–18]. Although these experiments indicate that CO2 exerts beneficial effects in the lungs, the pulmonary vascular response to hypercapnia under various conditions remains to be clarified. Moreover, reports to date of the vasoactive action of CO2 have chiefly concentrated on its vasodilatory and beneficial effects. We know that discrepant vasoactive action of CO2 may arise from differences in pulmonary vascular tone but the pressure–response relationship between the degree of CO2-induced vasodilatation and the level of PAP has not been studied.
It is known that endothelial cells release both vasoconstrictors and vasodilators in modulating pulmonary vascular tone. The balance of vasoconstrictors and vasodilators ultimately determines the pulmonary vascular tone and structure in physiologic and pathologic states [19–23]. Endothelin-1 (ET-1) is a potent vasoconstrictor peptide produced by endothelial cells and has been widely implicated to be critical in the modulation of hypoxic pulmonary vasoconstriction [20, 24, 25]. ETA receptor activation has been shown to be associated with vasoconstriction, whereas ETB receptors, located mainly on the vascular endothelium, are responsible for the release of vasodilator substances such as nitric oxide (NO) upon stimulation [20, 26–29]. It has recently emerged that vasoactive mediators such as NO and ET-1 play an important role in the modulation of pulmonary vessel response to hypoxic stimulation [3, 30–34]. Moreover, hypercapnia and hypoxic pulmonary vasoconstriction usually coexist in ARDS [14, 35, 36]. There has been considerable interest in the effect of hypercapnic acidosis on hypoxic and ET-1-induced pulmonary vasoconstriction.
In the present study we attempted to assess the effect of CO2 on pulmonary vascular tone under various conditions. First, we tested whether the vasodilator effect of CO2 on pulmonary circulation was dependent on the level of pulmonary arterial pressure (PAP) induced by ET-1 and hypoxia stimulation. Second, we attempted to clarify the role of NO in mediating the pulmonary vascular response to hypercapnia, hypoxia, and ET-1 stimulation. Therefore, the pulmonary vascular responses to CO2 inhalation were observed in isolated rat lungs under different levels of PAP induced by various doses of ET-1. The vasodilatory effects of CO2 inhalation on pulmonary hypertension were evaluated with comparisons of the vascular tone at normoxic-hypercapnia (5% CO2 in air) and hypoxic-hypercapnia (5% CO2 in N2) ventilation. To clarify the modulatory role of NO, we investigated the effect of NO and ETB receptor blockade on hypercapnia, hypoxia, and ET-1-induced changes in pulmonary vascular tone.
Materials and Methods
Animals
Adult male Sprague-Dawley (SD) rats weighing 300–350 g were used. The specific pathogen-free animals were purchased from the National Animal Center and housed in a temperature-controlled animal room. The room temperature was maintained at 22 ± 1°C under a 12/12-h light/dark regimen. Food and water were available ad libitum. The use and care of the animals were approved by the Animal Care and Use Committee of Kaohsiung Medical University.
Isolation and Perfusion of Rat Lungs
The rats were deeply anesthetized with an intraperitoneal injection of pentobarbital sodium (50 mg kg−1). The experimental setup was modified from previous studies [21, 27, 37]. After a tracheotomy, the lungs were artificially ventilated with room air. Heparin (1 U/g) was administered into the left ventricle after a midsternal thoracotomy. Ten milliliters of blood was collected from the right ventricle and mixed with 10 ml of Hank’s balanced salt solution (HBSS; in mM: NaCl, 136.9; KCl, 5.4; glucose, 5.6; KH2PO4, 0.4; Na2HPO4, 0.3; and 6% albumin, and pH was adjusted to 7.35–7.40) and subsequently used to perfuse the isolated lungs. In addition, the perfusion medium was gassed with a mixture of 5% CO2 and monitored continuously for pH. During the initial stabilization period, the pH was adjusted to 7.4 ± 0.05 with HCl. A cannula was placed in the pulmonary artery through a puncture into the right ventricle and a tight ligature was placed around the main trunk of the pulmonary artery. A large catheter was inserted into the left atrium through the left ventricle and mitral valve and fixed by ligature at the apex of the heart to divert pulmonary venous outflow into a reservoir. A third ligature was placed above the arterioventricular junction to prevent perfusate flow into the ventricles. Perfusion fluid, maintained at 37 ± 0.5°C, was circulated by use of a roller pump at a flow rate of 10 ml min−1. The PAP and pulmonary venous pressure (PVP) were measured with pressure transducers (Gould Instruments, Cleaned, OH) from a side arm of the inflow and outflow cannula. The PVP was set at 2 mmHg by adjusting the height of the venous reservoir.
After an initial hyperinflation to reverse atelectasis, the lungs were ventilated at 60–70 breaths/min and tidal volume at 2.5–3 ml. The end-expiratory pressure was set to 2 cm H2O. The gas tension in the perfusate was measured at the beginning of each experiment and after changes in ventilatory gas mixtures by collecting perfusion fluid anaerobically and analyzing immediately using a gas analyzer (Stat profile 5). There were three criteria for a satisfactory isolated lung preparation: no leakage at the site of cannula insertion, no evidence of homeostasis or edema, and an isogravimetric state.
Drug Preparation and Delivery
Drug solutions were prepared immediately before use. ET-1, N-nitro-l-arginine methyl ester (L-NAME, NOS blocker), and BQ788 (ETB receptor blocker) were purchased from Sigma Chemical (St. Louis, MO, USA). ET-1 was added into a side way prior to the roller pump. L-NAME and BQ788 were added directly into the venous reservoir.
Experimental Outline
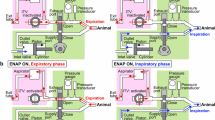
Experiments in isolated perfused lungs were organized into two series. Series A examined the effect of CO2 on ET-1-induced pulmonary vasoconstriction under normoxic-hypercapnia ventilation with and without endogenous NO. To assess the role of NO in mediating the pulmonary vascular response to hypercapnia and ET-1 challenge, ET-1-induced pulmonary vasoconstriction and CO2-induced vasodilatation were compared between Group A1 and Group A2 (pretreated with L-NAME, 400 mM and BQ788, 1 μM).
Experiment series B was carried out to evaluate the effect of CO2 on ET-1-induced pulmonary vasoconstriction under hypoxic-hypercapnia ventilation with and without endogenous NO. To clarify the modulation role of NO in response to hypoxic-hypercapnia and ET-1 challenge, the pulmonary vascular response was compared between Group B1 and Group B2 (pretreated with L-NAME, 400 mM and BQ788, 1 μM).
Experimental Protocol
During the baseline period lungs were ventilated with room air under constant perfusion flow (10 ml min−1). Subsequently, the preparations were randomized into four groups (A1, n = 8; A2, n = 8; B1, n = 8; and B2, n = 8) and sequentially challenged with graded concentrations (5, 50, and 200 pmol) of ET-1. Following each dose of ET-1, the pH, gas tension in the perfusate, and PAP were obtained after steady PAP values were observed over a period of at least 10 min. Thereafter, the inspired gas was switched to the following mixture: (1) Groups A1 and A2: normoxic-hypercapnia gas with 5% CO2 in air, and (2) Groups B1 and B2: hypoxic-hypercapnia gas with 5% CO2 in N2. After 10 min of experimental gas inhalation, the changes in PAP, pH, and gas tension in the perfusate were recorded. The inspired gas was then switched back to room air for 10 min before the next challenge of ET-1 and inhaled gas.
Acetic Acid Group
In this additional experiment (n = 6), we intended to observe the vasoactive effect of acidosis, which may clarify whether the vasodilatory effect of CO2 is pH dependent. ET-1 (200 pmol) was administered to induce pulmonary hypertension. Subsequently, two challenge doses of acetic acid (1.5 M/100 ml) were given 10 min apart to observe the change in PAP and perfusate pH.
Statistical Analysis
Values are expressed as mean ± SEM. Statistical evaluation of the differences among and within groups was performed using paired Student t test. Differences were considered statistically significant at p < 0.05.
Results
Effect of CO2 on ET-1-Induced Pulmonary Vasoconstriction under Normoxic-Hypercapnia Ventilation with and without Endogenous NO
In experiment series A, ventilation with normoxic-hypercapnia gas produced a significant increase in PaCO2 (p < 0.01) and a decrease in pH value (p < 0.01) (Table 1). ET-1 caused a dose-dependent increase in PAP at constant perfusion of the isolated lungs (Table 1, Fig. 1a). In Group A1, ET-1 at doses of 5, 50, and 200 pmol elevated the PAP by 1.9 ± 0.5, 4.2 ± 0.9, and 9.7 ± 2.0 mmHg, respectively. Inhalation of normoxic-hypercapnia gas directly decreased the PAP by 2.6 ± 0.7, 4.7 ± 0.8, and 8.7 ± 1.3 mmHg (p < 0.01) (Fig. 1a, b). However, the PAP rebounded by 2.4 ± 0.6, 3.8 ± 1.4, and 10.0 ± 2.7 mmHg when the inhaled gas was switched back to room air (Fig. 1a).
a Graph representing mean (SEM) PAP at baseline and during the course of the experiment in series A. b, c PAP change in response to normoxic-hypercapnia gas (5% CO2 in air) following with various doses of ET-1 challenge in Group A1 and Group A2. PAP increased significantly in response to each dose of ET-1 († p < 0.05; †† p < 0.01 compared with previous challenge doses). Normoxic-hypercapnia gas challenge (5% CO2 in air) caused vasodilatory effects which tended to be more evident at higher PAP (* p < 0.05; ** p < 0.01 compared with previous course of challenge). d Percent relaxation in response to CO2 showed no significant difference between Group A1 and Group A2. The vasodilatation effect of CO2 was not affected by L-NAME and BQ788
In Group A2, there was no significant influence of L-NAME and BQ788 pretreatment on basal PAP. In this group we observed that the ET-1 vasoconstriction effect was enhanced under endogenous NO inhibition. The increases in PAP were 2.7 ± 0.8, 6.8 ± 1.1, and 14.3 ± 1.5 mmHg with the three sequential ET-1 doses. Normoxic-hypercapnia gas inhalation decreased the PAP by 3.3 ± 1.0, 7.8 ± 0.8, and 12.3 ± 2.1 mmHg (p < 0.01), respectively (Fig. 1a, c). Again, the PAP rebounded by 3.4 ± 1.4, 7.3 ± 0.8, and 9.8 ± 2.4 mmHg when the inhaled gas was changed to room air (Fig. 1a). Comparing the percentages of normoxic-hypercapnia gas-induced relaxation in both groups, the vasodilatory effect of CO2 was not affected by pretreatment with L-NAME and BQ788 (Fig. 1d).
The Effect of CO2 on ET-1-Induced Pulmonary Vasoconstriction under Hypoxic-Hypercapnia Ventilation with and without Endogenous NO
In experiment series B, ventilation with hypoxic-hypercapnia gas produced a significant increase in PaCO2 (p < 0.01) and decrease in pH value (p < 0.01) (Table 1). ET-1 also caused a dose-dependent increase in PAP at constant perfusion of the isolated lungs (Table 1, Fig. 2a). In Group B1, ET-1 at doses of 5, 50, and 200 pmol elevated the PAP by 2.1 ± 0.6, 3.8 ± 0.9, and 6.6 ± 1.3 mmHg, respectively (Fig. 2a). With challenge by ET-1, direct vasodilatation in response to the hypoxic-hypercapnia gas (5% CO2 in N2) was observed. The PAP directly decreased by 3.3 ± 0.8, 4.9 ± 1.2, and 6.2 ± 0.9 mmHg (p < 0.05), and such effects were reversible by changing the inhaled gas to room air (Fig. 2a, b). In Group B2, inhibition of NO synthesis by L-NAME and BQ788 evoked a biphasic response with transient hypoxic vasoconstriction. In this group, the PAP increases by the three sequential doses of ET-1 were 1.8 ± 0.6, 3.5 ± 0.9, and 6.3 ± 1.5 mmHg. In response to hypoxic-hypercapnia gas (5% CO2 + N2), PAP was initially increased by 8.2 ± 1.8, 11.0 ± 2.0, and 16.2 ± 3.5 mmHg (p < 0.01). However, after 4–6 min of gas inhalation, PAP started to drop gradually; after 10 min of gas inhalation, PAP had decreased by 7.0 ± 1.2, 9.8 ± 2.2, and 14.2 ± 2.1 mmHg (p < 0.01) (Fig. 2a, c). Again, inhalation of room air reversed the PAP by 3.0 ± 1.2, 4.8 ± 2.3, and 5.0 ± 3.7 mmHg (Fig. 2a). In these series of experiments, inhibition of endogenous NO tended to preserve the pulmonary vasoconstrictor response to hypoxia, but it did not eliminate the vasodilatory effect of CO2.
a Graph representing mean (SEM) PAP at baseline and during the course of the experiment in series B. b, c PAP change in response to hypoxic-hypercapnia gas (5% CO2 in N2) following with various doses of ET-1 challenge in Group B1 and Group B2. PAP increased significantly in response to each dose of ET-1 († p < 0.05; †† p < 0.01 compared with previous challenge doses). In Group B1, hypoxic-hypercapnia gas challenge (5% CO2 in N2) caused direct vasodilatation (* p < 0.05; ** p < 0.01 compared with previous course of challenge). In Group B2, with pretreatment of L-NAME and BQ788, hypoxic-hypercapnia gas challenge evoked a biphasic response with a transient hypoxic vasoconstriction (first phase) followed by CO2 vasodilatation (second phase) (‡ p < 0.05 and ‡‡ p < 0.01, hypoxic vasoconstriction compared with previous course of challenge; * p < 0.05 and ** p < 0.01, CO2 vasodilatation vs. previous course of challenge)
Effect of Acidosis on ET-1-Induced Pulmonary Hypertension
In the acetic acid group, with institution of ET-1 (200 pmol), PAP was elevated from 15.3 ± 0.7 to 19.7 ± 1.5 mmHg. On the first dose of acetic acid [1.5 M (100 μl)], the pH value dropped to 7.13 ± 0.09 from 7.43 ± 0.03 while PAP was measured as 20.7 ± 1.6 mmHg. On the second dose of acetic acid [1.5 M (100 μl)], the pH value dropped to 6.98 ± 0.3 while PAP was measured as 20.9 ± 3.2 mmHg (Fig. 3).
Discussion
We have obtained several findings in the present study. The CO2-mediated vasodilatory effect on pulmonary vascular tone was more evident with pulmonary hypertension induced by ET-1 or hypoxic challenge. Also, the higher the PAP the stronger the vasodilatory effect observed (Figs. 1a, 2a), which indicates a pressure–response relationship between the degree of CO2-induced vasodilatation and the level of PAP. The results also suggest that CO2 is not a specific antagonist of constrictor stimulus to hypoxia and ET-1. Pretreatment with L-NAME and BQ788 significantly enhanced ET-1 and hypoxic pulmonary vasoconstriction (Figs. 1a, 2a). However, the pulmonary vasodilatory effects of CO2 essentially were not affected by L-NAME or BQ788 (Fig. 1d), suggesting that NO was not involved in the hypercapnic vasodilatation.
A number of factors have been proposed to be involved in the mediation or modulation of hypoxic pulmonary vasoconstriction, including NO, angiotension II, prostaglandin, and endothelin. Several studies have pointed out that an increase in NO production during acute or chronic hypoxia tends to blunt the vasoconstrictor effect induced by hypoxia [9, 22, 32, 38]. ETA receptor activation has been shown to be associated with vasoconstriction, whereas ETB receptors located mainly on the vascular endothelium are responsible for the release of vasodilator substances such as NO upon stimulation [26, 31, 34, 39]. In our study, we observed direct vasodilatation in response to hypoxic-hypercapnia gas inhalation in Group B1 with challenges of various doses of ET-1 (Fig. 2a, b). In contrast, in Group B2 with challenges of ET-1, inhibition of NO evoked a biphasic response of transient hypoxic vasoconstriction followed by CO2-induced vasodilatation in response to hypoxic-hypercapnia (Fig. 2a, c). In Group B experimental conditions, under hypoxia exposure, ET-1 binding with type B receptor enhances NO synthesis which could counterbalance hypoxic vasoconstriction. This phenomenon could explain the different responses to hypoxic gas between Groups B1 and B2. In our additional experiment, we proved that the CO2-induced vasodilatation observed in Group B2 could be aborted with pure N2 inhalation (data not shown). These results also indicate that NO is significantly involved in ET-1 and hypoxic vasoconstriction, while not contributing to hypercapnic ventilation in the face of ET-1 and hypoxic vasoconstriction. In clinical observations, hypoxia and hypercapnia often coexist with ARDS and other forms of acute or chronic lung disease [14]. In the present study we proved that acute hypoxia causes pulmonary vasoconstriction but coexistent hypercapnia eliminates this effect. These findings suggest that coexistent hypercapnia inhibits hypoxia-induced pulmonary vasoconstriction in an isolated lung model.
There is evidence that high CO2 tension with elevated hydrogen ions (low pH) increases calcium influx and is the main cause of vasoconstriction [4, 8, 10]. Early work done by Duke et al. [40] and Shaw and Barer [5] showed that under normal vascular tone, CO2 usually caused weak vasoconstriction; the addition of acid also caused vasoconstriction, while alkali administration caused vasodilatation. Subsequent studies have reported that respiratory acidosis tends to potentiate the pressor response to hypoxia and vasoconstrictors, while respiratory alkalosis exerts the opposite effect [6, 8]. These findings suggest that an increase in hydrogen ion concentration alone causes pulmonary vasoconstriction and that an increase in CO2 tension in the blood could attenuate the vasomotor response to hypoxia or vasoconstrictors without depending on the hydrogen ion concentration. In the present study we also confirmed that the vasodilatory effect of CO2 is pH-independent. In the additional experiment we added acetic acid to alter the pH value close to the value produced by hypercapnia (Fig. 3). The addition of acetic acid decreased the pH but slightly elevated the PAP. In this respect, our observation agrees with that of Viles and Shepherd [4] who also found that CO2 acted as a pulmonary vasodilator independent of hydrogen ion concentration. The action of CO2 on vascular tone was described to be local since it was present after autonomic blockade in isolated perfused lungs and was not abolished in intact animals by vagotomy or atropine [5]. Little is known about the mechanisms of the vasodilator effect of CO2 on the pulmonary circulation. There has been considerable interest in the role of NO in mediating hypercapnic vasodilatation. In the present study, blocking endogenous NO with L-NAME and BQ788 did not eliminate the vasodilatory response to hypercapnia, but it enhanced hypoxic and ET-1 pulmonary vasoconstriction. NO seems to specifically modulate ET-1 and hypoxic pulmonary vasoconstriction while not being involved in CO2-induced vasodilatation. In contrast, Yamaguchi et al. [41] documented that hypercapnic acidosis elevated vascular tone and perfusate nitrite/nitrate in an isolated lung model. Other studies have also reported that hypercapnia acidosis is associated with the upregulation of NOS-mediated NO-dependent effects at vascular and molecular levels [42–44]. Although our results differ from previous studies, it appears that acidification may stimulate unidentified mechanisms in the pretranscriptional phase of eNOS [45, 46]. On the basis of those studies, it has been proposed that the effect of CO2 dilatation is a direct action on smooth muscle while constriction is caused by the increasing intracellular hydrogen ion concentration. Our results also suggest that the dilator action of CO2 is independent of the constrictor stimulus, as CO2 produces a nonspecific antagonism of constriction response to hypoxia and ET-1. According to previous studies [5, 6, 41, 47], there is no significant difference in pulmonary vascular resistance in response to graded CO2 or different concentration of CO2. In the present study we did not titrate the optimum dose of CO2 but simply used a concentration of 5% CO2. This produced a degree of hypercapnia acidosis similar to that commonly observed when using protective ventilatory strategies. Reports to date indicate that the vasoactive action of CO2 is dependent on the initial pulmonary vascular resistance; during basal tone condition, CO2 is a mild vasoconstrictor, while at high pulmonary vascular resistance, it is a potent vasodilator [2, 4–10, 13, 17]. In this connection, our results support the finding that the vasodilator effect of CO2 on pulmonary circulation is dependent on the level of PAP, and they also indicate that the dilatory effect of CO2 tends to be more evident at high PAP. We have demonstrated, for the first time, a pressure–response relationship between the degree of CO2-induced vasodilatation and the level of PAP.
In ARDS patients using mechanical ventilation, permissive hypercapnia with a small tidal volume is viewed to be an undesirable side effect to be tolerated in order to prevent ventilator-induced lung injury. There is now increasing evidence from several experimental models that suggests therapeutic hypercapnia by inspired CO2 exerts a protective effect. Our findings are encouraging in that increased partial pressure of CO2 in arterial blood might be a beneficial adjunct to the strategies of lung protective ventilation in critical illness rather than as an inconvenient side effect. This could have important implications for the clinical management of mechanical ventilation in intensive care settings.
In conclusion, our data provide evidence that (1) CO2 produces pulmonary vasodilatation at high PAP under ET-1 and hypoxic vasoconstriction, (2) the vasodilatory effects of CO2 at different pressure levels vary in accordance with the levels of PAP—the dilatory effect tends to be more evident at higher PAP, and (3) endogenous NO attenuates ET-1 and hypoxic pulmonary vasoconstriction but does not augment CO2-induced vasodilatation.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- ET-1:
-
Endothelin-1
- NO:
-
Nitric oxide
- PAP:
-
Pulmonary arterial pressure
- PVP:
-
Pulmonary venous pressure
References
Green M, Widdicombe JG (1966) The effect of ventilation of dogs with different gas mixtures on airway calibre and lung mechanics. J Physiol 186(2):363–381
Brimioulle S, Lejeune P, Vachiery JL, Leeman M, Melot C, Naeije R (1990) Effects of acidosis and alkalosis on hypoxic pulmonary vasoconstriction in dogs. Am J Physiol 258(2):H347–H353
Cutaia M, Rounds S (1990) Hypoxic pulmonary vasoconstriction: physiologic significance, mechanism and clinical relevance. Chest 97(3):706–718
Viles PH, Shepherd JT (1968) Relationship between pH, PO2, and PCO2 on the pulmonary vascular bed of the cat. Am J Physiol 215(5):1170–1176
Shaw JW, Barer GR (1971) Pulmonary vasodilator and vasoconstrictor actions of carbon dioxide. J Physiol 213(3):633–645
Schreiber MD, Soifer SJ (1998) Respiratory alkalosis attenuates thromboxane-induced pulmonary hypertension. Crit Care Med 16(12):1225–1228
Astin TW, Barer GR, Shaw JW, Warren PM (1973) The action of carbon dioxide on constricted airways. J Physiol 235(3):607–623
Malik AB, Kidd BS (1973) Independent effects of change in H+ and CO2 concentrations on hypoxic pulmonary vasoconstriction. J Appl Physiol 34(3):318–323
Benumof JL, Wahrenbrock EA (1975) Blunted hypoxic pulmonary vasoconstriction by increased lung vascular pressures. J Appl Physiol 38(5):846–850
Baudouin SV, Evans TW (1993) Action of carbon dioxide on hypoxic pulmonary vasoconstriction in the rat lung: evidence against specific endothelium-derived relaxing factor-mediated vasodilation. Crit Care Med 21(5):740–746
Laffey JG, Tanaka M, Engelberts D, Luo X, Yuan S, Keith TA, Post M, Lindsay T, Kavanagh BP (2000) Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med 162(6):2287–2294
Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller MD (2001) Protective effect of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164(5):802–806
Laffey JG, Honan D, Hopkins N, Hyvelin JM, Boylan JF, McLoughlin P (2004) Hypercapnic acidosis attenuates endotoxin-induced acute injury. Am J Respir Crit Care Med 169(1):46–56
Kregenow DA, Rubenfeld GD, Hudson LD, Swenson ER (2006) Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med 34(1):1–7
Chonghaile M, Higgins BD, Costello JF, Laffey JG (2008) Hypercapnic acidosis attenuates severe acute bacterial pneumonia-induced lung injury by a neutrophil-independent mechanism. Crit Care Med 36(12):3135–3144
Kregenow DA, Swenson ER (2002) The lung and carbon dioxide: implications for permissive and therapeutic hypercapnia. Eur Respir J 20(1):6–11
Kantores C, McNamara PJ, Teixeira L, Engelberts D, Murthy P, Kavanagh BP, Jankov RP (2006) Therapeutic hypercapnia prevents chronic hypoxia-induced pulmonary hypertension in the newborn rat. Am J Physiol Lung Cell Mol Physiol 291(5):L912–L922
Sinclair SE, Kregenow DA, Starr IR, Chi EY, Schimmel C, Lamm JE, Hlastala MP, Swenson ER (2006) Therapeutic hypercapnia and ventilation-perfusion matching in acute lung injury: low minute ventilation vs inspired CO2. Chest 130(1):85–92
Palmer RM, Ferrige AG, Moncada S (1987) Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327(6122):524–526
Yanagisawa M, Kurihare H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 323(23):411–415
Wang D, Hsu K, Hwang CP, Chen HI (1995) Measurement of nitric oxide release in the isolated perfused rat lung. Biochem Biophys Res Commun 208(3):1016–1020
Chen HI, Hu CT, Wu CY, Wang D (1997) Nitric oxide in systemic and pulmonary hypertension. J Biomed Sci 4(5):244–248
Kao SJ, Wang D, Yeh DY, Hsu K, Hsu YH, Chen HI (2004) Static inflation attenuated ischemia/reperfusion injury in an isolated rat lung in situ. Chest 126(2):552–558
Mann J, Farrukh IS, Michael JR (1991) Mechanisms by which endothelin 1 induces pulmonary vasoconstriction in the rabbit. J Appl Physiol 71(2):410–416
Kourembanas S, Marsden PA, McQuillan LP, Faller DV (1991) Hypoxia induces endothelin gene expression and secretion in cultured human endothelium. J Clin Invest 88(3):1054–1057
Wong J, Fineman JR, Heymann MA (1994) The role of endothelin and endothelin receptor subtypes in regulation of fetal pulmonary vascular tone. Pediatr Res 35(6):664–670
Uhlig S, von Bethmann AN, Featherstone RL, Wendel A (1995) Pharmacologic characterization of endothelin receptor responses in the isolated perfused rat lung. Am J Respir Crit Care Med 152(5 Pt 1):1449-1460
Markewitz BA, Kohan DE, Michael JR (1995) Endothelin-1 synthesis, receptors and signal transduction in alveolar epithelium: evidence for an autocrine role. Am J Physiol 268(2 Pt 1):L192–L200
Sato K, Oka M, Hasunuma K, Ohnishi M, Sata K, Kira S (1995) Effects of separate and combined ETA and ETB blockade on ET-1-induced constriction in perfused rat lungs. Am J Physiol 269(5 Pt 1):L668–L672
Hasunuma K, Rodman DM, O’Brien RF, McMurtry IF (1990) Endothelin 1 causes pulmonary vasodilation in rats. Am J Physiol 259(1 Pt 2):H48–H54
Liu SF, Crawley DE, Barnes PJ, Evans TW (1991) Endothelium-derived relaxing factor inhibits hypoxic pulmonary vasoconstriction in rats. Am Rev Respir Dis 143(1):32–37
Deleuze PH, Shiiya AN, Thoraval R, Eddahibi S, Braquet P, Chabrier PE, Loisance DY (1992) Endothelin dilates bovine pulmonary circulation and reverses hypoxic pulmonary vasoconstriction. J Cardiovas Pharmacol 19(3):354–360
Kourembanas S, McQuillan LP, Leung GK, Faller DV (1993) Nitric oxide regulates the expression of vasoconstrictors and growth factors by vascular endothelium under both normoxia and hypoxia. J Clin Invest 92(1):99–104
Ahlborg G, Lundberg JM (1997) Nitric oxide–endothelin-1 interaction in humans. J Appl Physiol 82(5):1593–1600
Brimioulle S, Lejeune P, Vachiery JL, Leeman M, Melot C, Naeije R (1990) Effects of acidosis and alkalosis on hypoxic pulmonary vasoconstriction in dogs. Am J Physiol 258(2 Pt 2):H347–H353
Dorrington KL, Talbot NP (2004) Human pulmonary vascular responses to hypoxia and hypercapnia. Eur J Physiol (Pflügers Arch) 449(1):1–15
Baker DG, Toth BR, Goad MEP, Barker SA, Means JC (1999) Establishment and validation of an isolated rat lung model for pulmonary metabolism studies. J Appl Toxicol 19(2):83–91
Hampl V, Archer SL, Nelson DP (1993) Chronic EDRF inhibition and hypoxia: effects on pulmonary circulation and systemic blood pressure. J Appl Physiol 75(4):1748–1757
Wong J, Vanderford PA, Fineman JR, Chang R, Soifer SJ (1993) Endothelin-1 produced pulmonary vasodilation in the intact newborn lamb. Am J Physiol 265(4 Pt 2):H1318–H1325
Duke HN, Killick EM, Marchant JV (1960) Changes in pH of the perfusate during hypoxia in isolated perfused cat lungs. J Physiol 153:413–422
Yamaguchi K, Takasugi T, Fujuta H, Mori M, Suzuk Y (1996) Endothelial modulation of pH-dependent presser response in isolated perfused rabbit lungs. Am J Physiol 270(1 Pt 2):H252–H258
Pedoto A, Caruso JE, Nandi J, Oler A, Hoffman SP, Tassiopoulos AK, McGraw DJ, Camporesi EM, Hakim TS (1999) Acidosis stimulates nitric oxide production and lung damage in rats. Am J Respir Crit Care Med 159(2):397–402
Bellocq A, Suberville S, Philippe C, Bertrand F, Perez J, Fouqueray B, Cherqui G, Baud L (1998) Low environmental pH is responsible for the induction of nitric-oxide synthase in macrophages. J Biol Chem 273(9):5086–5092
Serrano CV Jr, Fraticelli A, Paniccia R, Teti A, Noble B, Corda S, Faraggiana T, Ziegelstein RC, Zweier JL, Capogrossi MC (1996) pH dependence of neutrophil-endothelial cell adhesion and adhesion molecule express. Am J Physiol 271(3 Pt 1):C962–C970
Mizuno S, Demura Y, Ameshima S, Okamura S, Miyamori I, Ishizaki T (2002) Alkalosis stimulates endothelial nitric oxide synthase in cultured human pulmonary arterial endothelial cells. Am J Physiol Lung Cell Mol Physiol 283:L113–L119
Najarian T, Marrache AM, Dumont I, Hardy P, Beauchamp MH, Hou X, Peri K, Gobeil F Jr, Varma DR, Chemtob S (2000) Prolonged hypercapnia-evoked cerebral hyperemia via K+ channel-and prostaglandin E2-dependent endothelial nitric oxide synthase induction. Circ Res 87:1149–1156
Barer GR, Howard P, Shaw JW (1970) Sensitivity of pulmonary vessels to hypoxia and hypercapnia. J Physiol 206(2):25P–26P
Acknowledgments
This study was supported by a grant from Kaohsiung Medical University Research Foundation (KMU-M 097010).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chuang, IC., Dong, HP., Yang, RC. et al. Effect of Carbon Dioxide on Pulmonary Vascular Tone at Various Pulmonary Arterial Pressure Levels Induced by Endothelin-1. Lung 188, 199–207 (2010). https://doi.org/10.1007/s00408-010-9234-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-010-9234-7