Abstract
The coronavirus disease 2019 (COVID-19) pandemic was accompanied by an increase in mental health challenges including depression, stress, loneliness, and anxiety. Common genetic variants can contribute to the risk for psychiatric disorders and may present a risk factor in times of crises. However, it is unclear to what extent polygenic risk played a role in the mental health response to the COVID-19 pandemic. In this study, we investigate whether polygenic scores (PGSs) for mental health-related traits can distinguish between four resilience-vulnerability trajectories identified during the COVID-19 pandemic and associated lockdowns in 2020/21. We used multinomial regression in a genotyped subsample (n = 1316) of the CovSocial project. The most resilient trajectory characterized by the lowest mental health burden and the highest recovery rates served as the reference group. Compared to this most resilient trajectory, a higher value on the PGS for the well-being spectrum decreased the odds for individuals to be in one of the more vulnerable trajectories (adjusted R-square = 0.3%). Conversely, a higher value on the PGS for neuroticism increased the odds for individuals to be in one of the more vulnerable trajectories (adjusted R-square = 0.2%). Latent change in mental health burden extracted from the resilience-vulnerability trajectories was not associated with any PGS. Although our findings support an influence of PGS on mental health during COVID-19, the small added explained variance suggests limited utility of such genetic markers for the identification of vulnerable individuals in the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic and societal measures imposed to contain its spread have been accompanied by severe socio-economic and health-related burdens worldwide [1,2,3]. A large body of literature on the pandemic’s initial effects, declared a global pandemic accompanied by recommendations for social isolation in March 2020 [4], shows an increase in population-level anxiety, depression, psychological distress, suicidal ideation, and loneliness [5,6,7,8,9,10,11], with most severe and enduring impairments in individuals of younger age, female sex, and lower socio-economic status (SES) [7, 10, 12,13,14,15,16,17,18,19,20,21,22]. The majority of these studies has focused on identifying the role of demographic characteristics and socioeconomic living conditions as risk factors for mental health challenges. However, individual differences in mental health impairment may also be influenced by genetic predisposition. Genome-wide association studies (GWAS) have identified a wide range of common genetic variants and biological pathways contributing to an increased risk of major depressive [23] and anxiety disorders [24], loneliness [25], and suicidal ideation [26]. Moreover, some studies suggest that the risk of experiencing adverse exposures [27,28,29] or the impact of an adverse exposure on mental health can differ depending on the genetic predisposition for psychiatric disorders such as major depressive disorder (MDD) [30,31,32,33]. In the context of the COVID-19 pandemic, polygenic risk for psychiatric disorders has been associated with increased risk of any COVID-19 and severe COVID-19 infection [34], greater COVID-19-related threat and crisis perception [35], and greater physical and mental health impairments [35, 36], suggesting polygenic predisposition for psychiatric disorders as a risk factor for worse health outcomes in times of such collective crises.
However, not all studies support the role of polygenic risk in the mental health response to the COVID-19 pandemic [37]. Polygenic risk on the individual level can be assessed using polygenic scores (PGSs) which are computed as the weighted sum of an individual’s genetic risk variants previously associated with a given trait of interest in genome-wide association analyses [38]. PGSs thus represent an individual’s additive genetic predisposition for a given common trait in a single score. Previous studies addressing mental health during Covid-19 differ in the selected PGS, COVID-19-related timing, and mental health outcome. When adjusting for pre-pandemic baseline symptoms, Taylor et al. [37], for example, show that the PGSs for MDD, anxiety and loneliness were not associated with the corresponding phenotype observed in June-July and November–December 2020. Warmerdam et al. [35], on the other hand, report a positive effect of the life satisfaction PGS on perceived quality of life over a 10-month period along with significant associations of several PGS including MDD and educational attainment with mental health at baseline in March 2020. Taking genetic correlations between PGS into account, Ahrens et al. [36] found a significant positive association between a pleiotropic neurodevelopmental genetic factor (consisting of two PGSs), but no other genetic factor, and a more acute mental dysfunction trajectory during the first COVID-19 lockdown. Pleiotropic mechanisms between psychiatric disorders have been demonstrated in a growing number of studies [39,40,41,42,43]. Lee et al., for instance, identified three correlated genetic factors, which together explained 51% of the genetic variation in eight combined neuropsychiatric disorders [43]. Moreover, Grotzinger et al. [39] found four genetic factors (neurodevelopmental, compulsive, psychotic, and internalizing) with, in part, distinct biobehavioral correlates. PGS based on these broad genetic factors may better represent a genetic vulnerability to the cumulative burden of complex stressors such as the COVID-19 pandemic and may account for more phenotypic variation in mental health outcomes compared to individual PGS. Yet, most previous studies have focused on individual PGSs.
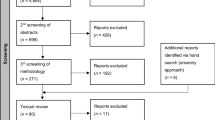
The present study was embedded in the CovSocial project, which is a longitudinal study of the effects of COVID-19 pandemic in 2020 and 2021 on various biopsychological outcomes in n = 3522 individual living in Berlin [44]. Repeated assessments of mental burdens took place over 7 measurement time points covering two lock-downs: T1 (before the lockdown in January 2020), T2 (during the first lockdown from mid-March to mid-April 2020), T3 (in June 2020 when restrictions were eased), T4 (November 2020), T5 (December 2020), T6 (January 2021), and T7 (mid-March to mid-April 2021, see Online Resource 2, Fig. 1). Building on prior frameworks, the recent Wither or Thrive Model of Resilience[45] conceptualized resilience during the COVID-19 pandemic as a dynamic process evolving over time in response to recurring stressors, manifesting as distinct resilience-vulnerability trajectories. To assess differential resilience-vulnerability trajectories in the CovSocial project[13] first a latent factor summarizing many different vulnerability indicators (e.g., depression, loneliness, stress, covid burden, etc.) and resilience indicators (e.g., optimism, coping, resistance) was built (see Online Resource S2, Fig. 2). Then, using growth mixture models, study participants were categorized into four resilience-vulnerability trajectories covering the entire time span from 2020 to 2021 including two lock-downs: a most vulnerable group (12.8%) with greatest mental health challenges reflected not only in more mental health challenges at baseline but also slower recovery rates and stronger pandemic fatigue effects during lock-downs, a more vulnerable group (16.7%), a more resilient group (46%), and a most resilient group (24.5%) with least mental health challenges at baseline, recovery to baseline after the first lockdown and lowest pandemic fatigue effect during the long second lock-down [13].
In the present investigation, we test whether individual PGS and PGS derived from latent phenotypes are associated with differences in these resilience-vulnerability trajectories and whether PGS derived from latent phenotypes explain greater phenotypic variation in mental health burden compared to individual PGS. Moreover, we explore the associations of the PGS with baseline and baseline independent change scores of latent mental health burden during the first and second COVID-19 lockdown in Germany.
Methods
Sample
Recruitment and inclusion criteria of the multi-phase CovSocial project are described in Godara et al. [13] and the Online Resource S1. This study is based on a genotyped subsample of the first phase of the CovSocial project which focuses on the impact of pandemic-related lockdowns in Germany on various biopsychological domains including mental health burden and vulnerability (n = 3522, age 18–65 years, 65.11% female). Characteristics of the analytic sample of this study (n = 1316) are reported in Table 1. Compared to the full Phase 1 CovSocial sample, participants in the analytic sample were significantly older, more often in the above-average income group, more often diagnosed with a lifetime mental disorder, less often in the most vulnerable group, and scored on average lower in latent vulnerability at T4 (see Online Resource S3, Table 1).
The study was approved by the Ethics Committee of Charité—Universitätsmedizin Berlin (#EA4/172/20 and #EA1/345/20) and was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent prior to participation.
Longitudinal measures and study design
Mental health burden and vulnerability measures consisted of both validated scales and self-generated questions. Stress perception, self-efficacy beliefs, and depressive and anxiety symptoms were assessed using the Perceived Stress Scale (PSS-4 [46]), the General Self-Efficacy Short Scale (ASKU [47]), the Patient Health Questionnaire-2 (PHQ-2 [48]), and the Generalized Anxiety Disorder Scale (GAD-2 [49]), respectively. Self-generated questions were developed for capturing aspects of resilience vulnerability that are specific to the given pandemic and its dynamic nature (e.g., pandemic-related burdens, loneliness, life satisfaction). A full list of these questions and detailed study design can be found in the Online Resource S2. As shown in Online Resource S2, Fig. 1, data were collected with repeated online surveys at seven timepoints: T1 (before the lockdown in January 2020), T2 (during the first lockdown from mid-March to mid-April 2020), T3 (in June 2020 when restrictions were eased), T4 (November 2020), T5 (December 2020), T6 (January 2021), and T7 (mid-March to mid-April 2021). The first three timepoints were assessed retrospectively, in three separate blocks of questionnaires, from 11 September 2020 to 7 December 2020. For the last four time points (T4–T7), participants answered the blocks of 11 questionnaires at the end of each month and rated their feelings, perceptions, and behavior for the last 4 weeks.
As previously described [13] and illustrated in Online Resource 2, Fig. 2, at each of the seven timepoints a latent resilience-vulnerability factor was derived from all measures. Change in the seven extracted factor scores over time was then modelled using latent change score (LCS) and growth curve mixture modelling techniques in Mplus. Changes in resilience-vulnerability from T1 to T2 (acute lockdown effect) and from T2 to T3 (effect of re-opening) were assessed by modeling the differences between the respective time points as latent variables and are referred to as LCS1 (T1–T2) and LCS2 (T2–T3). A linear growth function was specified for T4–T7 with the latent intercept factor positioned at T4. Change from T4 to T7 is referred to as Slope T4–T7 in the following. To identify subpopulations with different mean growth trajectories, mixture analysis was applied to the growth model, resulting in four groups: the most vulnerable (12.8%) with the highest mental health burden, more vulnerable (16.7%), more resilient (46%), and most resilient group (24.5%) with the lowest mental health burden (see Table 1 for group sizes of the analytic sample used in this study).
Genotype data
DNA was isolated from saliva samples for n = 1535 participants and genome-wide SNP genotyping performed using Illumina Genome Screening arrays (GSA) version 3 according to the manufacturer’s guidelines (Illumina Inc., San Diego, CA). Quality control was performed in Plink 1.9 [50]. SNPs with a minor allele frequency below 1%, a call rate below 98%, or with deviation from Hardy–Weinberg-Equilibrium with a p value < 1 × 10–05 were excluded. Furthermore, SNPs mapping to multiple locations as well as duplicated variants were removed.
Individuals with a genotype call rate below 98% (n = 48) and technical replicates (n = 12) were excluded. Any pair of samples with IBD estimates > 0.125 was checked for relatedness and for n = 6 confirmed. One sample of each pair was removed. Furthermore, individuals showing discrepancies between phenotypic and genotypic sex (n = 4) were removed. To retrieve ancestry-related information, we performed multi-dimensional scaling (MDS) analysis on the IBS matrix of quality-controlled genotypes [51]. Outliers, defined as samples presenting with a position on any of the first ten axes of variation deviating more than four standard deviations from the respective axis’ mean, were iteratively removed until no more outliers were detected (n = 55). Afterwards, individuals presenting with heterozygosity values more than four standard deviations away from the mean heterozygosity were also iteratively removed (n = 3). The first two MDS components (38.5% variance explained) were extracted and included as covariates in the following analyses to account for population structure.
Quality-controlled genotypes were then phased using SHAPEIT [52] and SNPs imputed using impute v2 [53] using the European 1,000 Genomes build 37 phase 3 sample as reference panel [54]. Imputed SNPs with a low information content metric (< 0.6), significant deviation from HWE (p < 10−05), or low MAF (< 1%) were excluded. Imputed genotype probabilities were converted into best-guessed genotypes using a threshold of 0.90. After quality control, genotype data were available for 1,407 subjects. Of these, n = 1316 samples with complete phenotypic information on resilience-vulnerability class and covariates were included in the following analyses.
Polygenic scores
Fifteen individual and four PGS derived from latent phenotypes were computed based on publicly available GWAS summary statistics (see Table 2). A PGS for height (based on Yengo et al. [55]) was added as a negative control. PGS were generated using PRS-CS [56] and PLINK 1.9 [50]. PRS-CS was applied to infer posterior mean effects by chromosome for autosomal single nucleotide polymorphisms (SNPs) that overlap between the given discovery genome-wide association study (GWAS) and the European 1000 Genomes linkage disequilibrium (LD) panel [54]. To ensure convergence of the underlying Gibbs sampler algorithm, we set Markov chain Monte Carlo (MCMC) iterations to 10,000 and the first 5000 MCMC iterations as burn-in [57]. For all other PRS-CS parameter the default settings were used. Using the PLINK 1.9 score function, raw PGSs were then calculated for each participant as the average risk allele count weighted by the posterior means effects returned by PRS-CS, and then standardized to cohort mean = 0 and SD = 1 in R [58] (4.1.3 (2022-03-10).
Covariates
As shown by Godara et al. [13], and also valid for this subsample, see Table 1, younger age, female sex, and lower than average household income, were associated with more vulnerable resilience-vulnerability trajectories, and thus controlled for in our analyses. Self-reported history of lifetime mental disorder was not included as a covariate because we theorize that both a diagnosis and a more vulnerable trajectory would be an outcome of polygenic risk instead of a confounding factor.
Statistical analyses
All statistical analyses were conducted in R [58] (version 4.1.3, 2022-03-10). Statistical significance was tested at a 5% level and multiple testing accounted for using the false discovery rate (FDR) for the 20 (correlated) predictors. The analysis code is publicly available at https://github.com/aschowe/CovSocial_PGS_Analysis_2023.git.
PGS validity and specificity
For PGS with available corresponding phenotype (e.g., life satisfaction PGS and trait life satisfaction item), we assessed validity using linear regression with the given phenotype as dependent and PGS as independent variable, controlling for the first two ancestral components. For each phenotype, we repeated these analyses using all computed PGS individually and ranked the explained phenotypic variance (in the form of adjusted R squared) to assess PGS specificity.
Polygenic scores and mental health burden during the COVID-19 lockdowns
To identify PGS that are associated with the resilience-vulnerability trajectories, we first tested for mean differences using one-way analysis of variance (ANOVA). We then further examined which specific resilience-vulnerability trajectory the identified PGS can distinguish using multinomial regression (nnet R-package (version 7.3-17) [59]). In this analysis, resilience-vulnerability trajectory was used as a dependent and PGS separately as an independent variable, controlling for the two ancestry principal components, age, sex, and income. The most resilient resilience-vulnerability trajectory served as the reference. To obtain an estimate of the added variance explained by PGS, we compared the adjusted R-squared between the model including the PGS to a model including only the phenotypic covariates. We repeated these analyses using linear regression (stats R-package, version 4.1.3 [58] with latent mental health burden at T1, T4, and latent change slopes between T1–T2, T2–T3, and T4–T7 (see Fig. 1) as the dependent variable to disentangle the association of PGS with latent baseline and change scores.
Average latent resilience-vulnerability factor scores are plotted for the analytic sample at each of the seven-time points for the four identified resilience-vulnerability trajectories from most vulnerable (top red line) to most resilient (bottom purple line). Further information on the resilience-vulnerability trajectories in the full CovSocial sample are provided in Godara et al. [13]. Error bars indicate standard error.
Results
Table 1 shows the demographic background of the analytic sample. Previously reported demographic differences among the four latent resilience-vulnerability trajectories were also seen in our subsample and thus accounted for using covariates in all analyses (see methods).
Correlation coefficients between all PGS can be found in the Online Resource S3, Table 2 and ranged from − 0.83 to − 0.01 and 0.01–0.89, in line with previous reports [39, 40, 60, 61]. We tested 15 individual PGS and 4 PGS derived from latent phenotypes, listed in Table 2. These included individual PGS derived from GWAS for psychiatric disorders, personality traits but also loneliness and well-being. The PGS derived from latent phenotypes were derived from GWAS of subjective well-being as well as a GWAS describing a general psychopathology, neurodevelopmental and internalizing factor.
We first tested how much variance the individual as well as PGS derived from latent phenotypes explained for the different phenotypes and observed explained variances from 0 to 5.6% in trait and mean symptom outcomes across all measurement occasions (see Online Resource, Figs. 1–6). Except for the anxiety disorder PGS (b = 0.33, adj. R-square = 0.001, p = 0.25), each individual PGS was significantly associated with their respective phenotype (i.e., depressiveness PGS—mean depressive symptoms (b = 0.07, adj. R-square = 0.016, p < 0.001), life satisfaction PGS—trait life satisfaction (b = 0.45, adj. R-square = 0.006, p = 0.007), loneliness PGS—trait loneliness (b = 0.07, adj. R-square = 0.009, p < 0.001,), anxiety-tension PGS—trait anxiety (b = 0.90, adj. R-square = 0.007, p = 0.002), neuroticism PGS—trait neuroticism (b = 1.32, adj. R-square = 0.023, p < 0.001,), general factor neuroticism PGS—trait neuroticism (b = 1.27, adj. R-square = 0.021, p < 0.001), educational attainment PGS—educational years (b = 0.88, adj. R-square = 0.056, p < 0.001,). The well-being spectrum PGS explained the largest amount of variance compared to all other PGS in mean depressive symptoms (b = − 0.09, adj. R-square = 0.027, p < 0.001), trait anxiety (b = − 2.09, adj. R-square = 0.038, p < 0.001), trait neuroticism (b = − 1.55, adj. R-square = 0.031, p < 0.001), and trait life satisfaction (b = 0.85, adj. R-square = 0.021, p < 0.001).
We next tested the associations of the PGS levels with the four resilience-vulnerability trajectories. We found that of the 20 individual PGS and PGS derived from latent phenotypes (see Table 3), the PGS for well-being (F(3) = 6.76, p = 0.0002), general neuroticism factor (F(3) = 5.21, p = 0.001), neuroticism (F(3) = 4.76, p = 0.003), MDD (F(3) = 3.39, p = 0.017), Tourette syndrome (F(3) = 3.35, p = 0.018), general psychopathy factors (F(3) = 3.23, p = 0.022), depressiveness (F(3) = 3.19, p = 0.023), and internalizing (F(3) = 2.72, p = 0.043) significantly differed between the four resilience-vulnerability trajectories. However, only associations with the well-being (FDR = 0.003) and general neuroticism factor PGS (p adj. = 0.02) remain significant after multiple testing correction (see Table 3 for an overview of all PGS results). Following up on these mean differences in PGS, we observe that individuals with lower well-being were less likely to be in the most vulnerable (OR = 0.63, p < 0.001), more vulnerable (OR = 0.78, p = 0.004), and more resilient (OR = 0.86, p = 0.039) trajectory compared to the most resilient group (adj. R-square = 0.3%, see Fig. 2a). Conversely, individuals with a higher factor neuroticism PGS were significantly more likely to be in the most vulnerable (OR = 1.48, p < 0.001), more vulnerable (OR = 1.29, p = 0.003), and more resilient (OR = 1.21, p = 0.009) trajectory compared to the most resilient group (adjusted R-square = 0.2%, see Fig. 2b). Both the well-being (added adj. R-square = 0.21%, p = 0.008) and the general neuroticism PGS (added adj. R-square = 0.2%, p = 0.023) significantly explained additional variance compared to the covariate-only model. The height PGS as a negative control did not differ between the resilience-vulnerability trajectories (see Tables 3 and 4).
Association between well-being PGS and resilience-vulnerability trajectory. Boxplots of the well-being PGS (a) and neuroticism PGS (b) are shown by resilience-vulnerability trajectory from the most vulnerable (left) to the most resilient (right) trajectory. Individuals with a higher value on the well-being PGS or a lower value on the General neuroticism PGS were more likely to be in the most resilient group compared to all other groups. PGS Polygenic Score, WBS well-being spectrum, NEU neuroticism. * < 0.05, **p < 0.01, ***p < 0.001
We then also investigated associations at the level of individual latent resilience-vulnerability scores that define the latent resilience-vulnerability trajectories. At T1 and T4, higher latent resilience-vulnerability factor score (indicating greater vulnerability characterized by higher mental health burden) was negatively associated with the well-being PGS (T1: b = − 0.13, p < 0.001, added adj R-square = 2.1%, T4: b = − 0.19, p < 0.001, added adj. R-square = 2.1%) and positively associated with the general neuroticism PGS (T1: b = 0.10 p < 0.001, added adj R-square = 1.3%; T4: b = 0.18, p < 0.001; added adj R-square = 1.9%). Latent change from T1 to T2, T2–T3, and T4–T7 was not associated with any PGS (see Table 5).
Discussion
The present study investigated whether genetic predisposition for mental health-related traits is associated with a more vulnerable resilience-vulnerability trajectory and higher mental health burden during the COVID-19 pandemic. We find that higher values on the general neuroticism PGS and lower values on the well-being spectrum PGS resulted in an increased likelihood to be assigned to a more vulnerable compared to the most resilient trajectory. The largest amount of variance (with an adj. R-square of 0.3%) in the resilience-vulnerability response trajectories as well as in baseline latent resilience-vulnerability was explained by the well-being spectrum PGS (with an adj. R-square of 2.1% at T1 and T4). Baseline-independent latent change in from T1 to T2, T2–T3, and T4–T7 was not associated with any PGS.
Our findings support the role of genetic predisposition in risk and resilience to mental health problems during the COVID-19 pandemic. Specifically, we find that PGS for emotional well-being-related traits are associated with a more vulnerable resilience-vulnerability trajectory characterized by a higher baseline, higher acute lockdown response, and less recovery. However, the small added variance explained by PGS consistent with previous studies [62,63,63] suggests still limited utility for the identification of individuals at risk for mental health impairment beyond socioeconomic predictors in the general population. The well-being PGS slightly outperformed all other PGS in predicting the resilience-vulnerability trajectories and baseline mental health burden, supporting that increased GWAS sample size and advances in multivariate methods can improve predictive performance for complex traits [64]. Yet, the latent general psychopathology, neurodevelopmental and internalizing disorder PGS were not associated with the resilience-vulnerability trajectory after multiple testing correction. The improved performance of PGS derived from latent phenotypes may thus only apply when it matches the outcome of interest well (e.g., here a combination of dimensional resilience and psychological vulnerability questionnaires summarized in Fig. S2 assessed in the general population). Differences in mental health outcomes may also explain why we did not find an effect of the neurodevelopmental PGS opposed to Ahrens et al.[36] who focused on mental dysfunction. Finally, none of the PGS was associated with baseline-independent change. These isolated change slopes may not capture well the higher-order mental health responses represented by the latent resilience-vulnerability profiles including global patterns of baseline and longitudinal change over seven timepoints. Yet, the finding is consistent with Taylor et al.’s [37] report of a lack of association between pre-pandemic controlled mental health and MDD, loneliness, and anxiety. The large majority of GWAS to date identify genetic variants based on main effects on a given cross-sectional trait or case–control status and may thus not be designed to predict change in response to specific stressors. Expanding efforts such as genome-by-trauma exposure association studies [65, 66] in terms of sample size and environmental exposures (e.g., socioeconomic hardship) may be promising approaches to improve the predictive power of PGS in the context of stressful life events in the future.
While the CovSocial study included longitudinal assessments, it is important to note that the first three timepoints were assessed retrospectively so that (lack of) association with acute change in mental health should be interpreted with caution. Bias of these retrospective reports was minimized through priming participants at the beginning of each questionnaire using news specific to the occasion of interest and separate assessment of the retrospective reports across three occasions. Another limitation is the small variability in the isolated latent change scores which restricted the statistical analysis. Moreover, mechanistically this study cannot disentangle whether associations with PGS are due to predisposition to lower mood itself or gene-environment correlation in which genetic predisposition, for example, is associated with an environment characterized by greater exposure to Covid-19-related burdens and is therefore associated with a more vulnerable trajectory. Nevertheless, this study could support the role of genetic predisposition in relation to the global resilience-vulnerability response to the COVID-19 pandemic.
Conclusion
The present study showed that a lower PGS for the well-being spectrum and a higher PGS for neuroticism are associated with more vulnerable mental health profiles in response to the recurring stressors associated with the COVID-19 pandemic in Germany in 2020 and 2021. Despite the overall low predictive power of common genetic markers, we may conclude that methodological advances in GWAS based on latent phenotypes present promising tools to increase explained phenotypic variation when the mental health outcome and genetic predictors match well.
Data availability
Data will be made available upon request.
References
Richards F, Kodjamanova P, Chen X, Li N, Atanasov P, Bennetts L et al (2022) Economic burden of COVID-19: a systematic review. Clin Outcomes Res 14:293–307. https://doi.org/10.2147/CEOR.S338225
Miyah Y, Benjelloun M, Lairini S, Lahrichi A (2022) COVID-19 impact on public health, environment, human psychology, global socioeconomy, and education. Sci World J 2022:5578284. https://doi.org/10.1155/2022/5578284
Kawohl W, Nordt C (2020) COVID-19, unemployment, and suicide. Lancet Psychiatry 7:389–390. https://doi.org/10.1016/S2215-0366(20)30141-3
Cucinotta D, Vanelli M (2020) WHO declares COVID-19 a pandemic. Acta Bio Medica Atenei Parm 91:157–160. https://doi.org/10.23750/abm.v91i1.9397
Jia R, Ayling K, Chalder T, Massey A, Broadbent E, Coupland C et al (2020) Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open 10:e040620. https://doi.org/10.1136/bmjopen-2020-040620
Fancourt D, Steptoe A, Bu F (2021) Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8:141–149. https://doi.org/10.1016/S2215-0366(20)30482-X
Chandola T, Kumari M, Booker CL, Benzeval M (2022) The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol Med 52:2997–3006. https://doi.org/10.1017/S0033291720005048
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A et al (2020) Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7:883–892. https://doi.org/10.1016/S2215-0366(20)30308-4
O’Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL et al (2021) Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 218:326–333. https://doi.org/10.1192/bjp.2020.212
Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E et al (2021) Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. J Epidemiol Community Health 75:224–231. https://doi.org/10.1136/jech-2020-215060
Silveira S, Hecht M, Matthaeus H, Adli M, Voelkle MC, Singer T (2022) Coping with the COVID-19 pandemic: perceived changes in psychological vulnerability, resilience and social cohesion before, during and after lockdown. Int J Environ Res Public Health 19:3290. https://doi.org/10.3390/ijerph19063290
Oberndorfer M, Dorner TE, Brunnmayr M, Berger K, Dugandzic B, Bach M (2022) Health-related and socio-economic burden of the COVID-19 pandemic in Vienna. Health Soc Care Community 30:1550–1561. https://doi.org/10.1111/hsc.13485
Godara M, Rademacher J, Hecht M, Silveira S, Voelkle MC, Singer T (2023) Heterogeneous mental health responses to the COVID-19 pandemic in Germany: an examination of long-term trajectories, risk factors, and vulnerable groups. Healthc Basel Switz 11:1305. https://doi.org/10.3390/healthcare11091305
Witteveen D, Velthorst E (2020) Economic hardship and mental health complaints during COVID-19. Proc Natl Acad Sci 117:27277–27284. https://doi.org/10.1073/pnas.2009609117
Wright L, Steptoe A, Fancourt D (2020) Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J Epidemiol Community Health 74:683–688. https://doi.org/10.1136/jech-2020-214475
Plümper T, Neumayer E (2020) The pandemic predominantly hits poor neighbourhoods? SARS-CoV-2 infections and COVID-19 fatalities in German districts. Eur J Public Health 30:1176–1180. https://doi.org/10.1093/eurpub/ckaa168
Pieh C, Budimir S, Probst T (2020) The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res 136:110186. https://doi.org/10.1016/j.jpsychores.2020.110186
Iob E, Frank P, Steptoe A, Fancourt D (2020) Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Netw Open 3:e2026064. https://doi.org/10.1001/jamanetworkopen.2020.26064
Chen JT, Krieger N (2021) Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US County versus zip code analyses. J Public Health Manag Pract 27:S43-56. https://doi.org/10.1097/PHH.0000000000001263
Bu F, Steptoe A, Fancourt D (2020) Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med 265:113521. https://doi.org/10.1016/j.socscimed.2020.113521
Labib SM, Browning MHEM, Rigolon A, Helbich M, James P (2022) Nature’s contributions in coping with a pandemic in the 21st century: a narrative review of evidence during COVID-19. Sci Total Environ 833:155095. https://doi.org/10.1016/j.scitotenv.2022.155095
Bustamante G, Guzman V, Kobayashi LC, Finlay J (2022) Mental health and well-being in times of COVID-19: a mixed-methods study of the role of neighborhood parks, outdoor spaces, and nature among US older adults. Health Place 76:102813. https://doi.org/10.1016/j.healthplace.2022.102813
Howard DM, Adams MJ, Clarke T-K, Hafferty JD, Gibson J, Shirali M et al (2019) Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci 22:343–352. https://doi.org/10.1038/s41593-018-0326-7
Otowa T, Hek K, Lee M, Byrne EM, Mirza SS, Nivard MG et al (2016) Meta-analysis of genome-wide association studies of anxiety disorders. Mol Psychiatry 21:1391–1399. https://doi.org/10.1038/mp.2015.197
Day FR, Ong KK, Perry JRB (2018) Elucidating the genetic basis of social interaction and isolation. Nat Commun 9:2457. https://doi.org/10.1038/s41467-018-04930-1
Li QS, Shabalin AA, DiBlasi E, Gopal S, Canuso CM, Palotie A et al (2023) Genome-wide association study meta-analysis of suicide death and suicidal behavior. Mol Psychiatry 28:891–900. https://doi.org/10.1038/s41380-022-01828-9
Schoeler T, Choi SW, Dudbridge F, Baldwin J, Duncan L, Cecil CM et al (2019) Multi-polygenic score approach to identifying individual vulnerabilities associated with the risk of exposure to bullying. JAMA Psychiat 76:730–738. https://doi.org/10.1001/jamapsychiatry.2019.0310
Feurer C, McGeary JE, Brick LA, Knopik VS, Carper MM, Palmer RHC et al (2022) Associations between depression-relevant genetic risk and youth stress exposure: Evidence of gene-environment correlations. J Psychopathol Clin Sci 131:457–466. https://doi.org/10.1037/abn0000757
Sallis HM, Croft J, Havdahl A, Jones HJ, Dunn EC, Smith GD et al (2021) Genetic liability to schizophrenia is associated with exposure to traumatic events in childhood. Psychol Med 51:1814–1821. https://doi.org/10.1017/S0033291720000537
Musliner KL, Andersen KK, Agerbo E, Albinana C, Vilhjalmsson BJ, Rajagopal VM et al (2023) Polygenic liability, stressful life events and risk for secondary-treated depression in early life: a nationwide register-based case-cohort study. Psychol Med 53:217–226. https://doi.org/10.1017/S0033291721001410
Iob E, Ajnakina O, Steptoe A (2023) The interactive association of adverse childhood experiences and polygenic susceptibility with depressive symptoms and chronic inflammation in older adults: a prospective cohort study. Psychol Med 53:1426–1436. https://doi.org/10.1017/S0033291721003007
Mullins N, Power RA, Fisher HL, Hanscombe KB, Euesden J, Iniesta R et al (2016) Polygenic interactions with environmental adversity in the aetiology of major depressive disorder. Psychol Med 46:759–770. https://doi.org/10.1017/S0033291715002172
Peyrot WJ, Milaneschi Y, Abdellaoui A, Sullivan PF, Hottenga JJ, Boomsma DI et al (2014) Effect of polygenic risk scores on depression in childhood trauma. Br J Psychiatry 205:113–119. https://doi.org/10.1192/bjp.bp.113.143081
Chen W, Zeng Y, Suo C, Yang H, Chen Y, Hou C et al (2022) Genetic predispositions to psychiatric disorders and the risk of COVID-19. BMC Med 20:314. https://doi.org/10.1186/s12916-022-02520-z
Warmerdam CAR, Wiersma HH, Lanting P, Ani A, Initiative LCR, Study LC et al (2022) Increased genetic contribution to wellbeing during the COVID-19 pandemic. PLOS Genet 18:e1010135. https://doi.org/10.1371/journal.pgen.1010135
Ahrens KF, Neumann RJ, von Werthern NM, Kranz TM, Kollmann B, Mattes B et al (2022) Association of polygenic risk scores and hair cortisol with mental health trajectories during COVID lockdown. Transl Psychiatry 12:1–10. https://doi.org/10.1038/s41398-022-02165-9
Taylor KS, Steptoe A, Iob E (2022) The relationship of adverse childhood experiences, hair cortisol, C-reactive protein, and polygenic susceptibility with older adults’ psychological distress during the COVID-19 pandemic. Mol Psychiatry 27:5038–5048. https://doi.org/10.1038/s41380-022-01805-2
Choi SW, Mak TS-H, O’Reilly PF (2020) Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc 15:2759–2772. https://doi.org/10.1038/s41596-020-0353-1
Grotzinger AD, Mallard TT, Akingbuwa WA, Ip HF, Adams MJ, Lewis CM et al (2022) Genetic architecture of 11 major psychiatric disorders at biobehavioral, functional genomic, and molecular genetic levels of analysis. Nat Genet 54:548–559. https://doi.org/10.1038/s41588-022-01057-4
Abdellaoui A, Verweij KJH (2021) Dissecting polygenic signals from genome-wide association studies on human behaviour. Nat Hum Behav 5:686–694. https://doi.org/10.1038/s41562-021-01110-y
Abdellaoui A, Sanchez-Roige S, Sealock J, Treur JL, Dennis J, Fontanillas P et al (2019) Phenome-wide investigation of health outcomes associated with genetic predisposition to loneliness. Hum Mol Genet 28:3853–3865. https://doi.org/10.1093/hmg/ddz219
Cross-Disorder Group of the Psychiatric Genomics Consortium, Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM et al (2013) Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet 45:984–994. https://doi.org/10.1038/ng.2711
Cross-Disorder Group of the Psychiatric Genomics Consortium (2019) Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell 179:1469-1482.e11. https://doi.org/10.1016/j.cell.2019.11.020
Singer T, Koop S, Godara M (2021) The CovSocial Project: how did berliners feel and react during the COVID-19 pandemic in 2020/21? Changes in aspects of mental health, resilience and social cohesion. CovSocial Proj, pp 1–107
Godara M, Silveira S, Matthäus H, Singer T (2022) The wither or thrive model of resilience: an integrative framework of dynamic vulnerability and resilience in the face of repeated stressors during the COVID-19 pandemic. Advers Resil Sci 3:261–282. https://doi.org/10.1007/s42844-022-00069-7
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Beierlein C, Kemper C, Kovaleva A, Rammstedt B (2013) Short scale for measuring general self-efficacy beliefs (ASKU). https://doi.org/10.12758/mda.2013.014
Löwe B, Kroenke K, Gräfe K (2005) Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res 58:163–171. https://doi.org/10.1016/j.jpsychores.2004.09.006
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K et al (2010) A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 122:86–95. https://doi.org/10.1016/j.jad.2009.06.019
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MAR, Bender D et al (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81:559–575
Barfield RT, Almli LM, Kilaru V, Smith AK, Mercer KB, Duncan R et al (2014) Accounting for population stratification in DNA methylation studies. Genet Epidemiol 38:231–241. https://doi.org/10.1002/gepi.21789
Delaneau O, Marchini J, Zagury J-F (2011) A linear complexity phasing method for thousands of genomes. Nat Methods 9:179–181. https://doi.org/10.1038/nmeth.1785
Howie BN, Donnelly P, Marchini J (2009) A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLOS Genet 5:e1000529. https://doi.org/10.1371/journal.pgen.1000529
Auton A, Abecasis GR, Altshuler DM, Durbin RM, Abecasis GR, Bentley DR et al (2015) A global reference for human genetic variation. Nature 526:68–74. https://doi.org/10.1038/nature15393
Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN et al (2018) Meta-analysis of genome-wide association studies for height and body mass index in ∼700,000 individuals of European ancestry. Hum Mol Genet 27:3641–3649. https://doi.org/10.1093/hmg/ddy271
Ge T, Chen C-Y, Ni Y, Feng Y-CA, Smoller JW (2019) Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat Commun 10:1776. https://doi.org/10.1038/s41467-019-09718-5
Schultz LM, Merikangas AK, Ruparel K, Jacquemont S, Glahn DC, Gur RE et al (2022) Stability of polygenic scores across discovery genome-wide association studies. Hum Genet Genomics Adv 3:100091. https://doi.org/10.1016/j.xhgg.2022.100091
R Core Team (2020) R: a language and environment for statistical computing
Venables WN, Ripley BD (2002) Modern applied statistics with S, 4th edn. Springer, New York
Hill WD, Weiss A, Liewald DC, Davies G, Porteous DJ, Hayward C et al (2020) Genetic contributions to two special factors of neuroticism are associated with affluence, higher intelligence, better health, and longer life. Mol Psychiatry 25:3034–3052. https://doi.org/10.1038/s41380-019-0387-3
Baselmans BML, van de Weijer MP, Abdellaoui A, Vink JM, Hottenga JJ, Willemsen G et al (2019) A genetic investigation of the well-being spectrum. Behav Genet 49:286–297. https://doi.org/10.1007/s10519-019-09951-0
Jamshidi J, Williams LM, Schofield PR, Park HRP, Montalto A, Chilver MR et al (2020) Diverse phenotypic measurements of wellbeing: heritability, temporal stability and the variance explained by polygenic scores. Genes Brain Behav 19:e12694. https://doi.org/10.1111/gbb.12694
Lewis CM, Vassos E (2020) Polygenic risk scores: from research tools to clinical instruments. Genome Med 12:44. https://doi.org/10.1186/s13073-020-00742-5
Grotzinger AD, Rhemtulla M, de Vlaming R, Ritchie SJ, Mallard TT, Hill WD et al (2019) Genomic SEM provides insights into the multivariate genetic architecture of complex traits. Nat Hum Behav 3:513–525. https://doi.org/10.1038/s41562-019-0566-x
Coleman JRI, Peyrot WJ, Purves KL, Davis KAS, Rayner C, Choi SW et al (2020) Genome-wide gene-environment analyses of major depressive disorder and reported lifetime traumatic experiences in UK Biobank. Mol Psychiatry 25:1430–1446. https://doi.org/10.1038/s41380-019-0546-6
Chuong M, Adams MJ, Kwong ASF, Haley CS, Amador C, McIntosh AM (2022) Genome-by-trauma exposure interactions in adults with depression in the UK biobank. JAMA Psychiat 79:1110–1117. https://doi.org/10.1001/jamapsychiatry.2022.2983
Okbay A, Wu Y, Wang N, Jayashankar H, Bennett M, Nehzati SM et al (2022) Polygenic prediction of educational attainment within and between families from genome-wide association analyses in 3 million individuals. Nat Genet 54:437–449. https://doi.org/10.1038/s41588-022-01016-z
Baselmans BML, Jansen R, Ip HF, van Dongen J, Abdellaoui A, van de Weijer MP et al (2019) Multivariate genome-wide analyses of the well-being spectrum. Nat Genet 51:445–451. https://doi.org/10.1038/s41588-018-0320-8
Grove J, Ripke S, Als TD, Mattheisen M, Walters RK, Won H et al (2019) Identification of common genetic risk variants for autism spectrum disorder. Nat Genet 51:431–444. https://doi.org/10.1038/s41588-019-0344-8
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E et al (2019) Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet 51:63–75. https://doi.org/10.1038/s41588-018-0269-7
Nievergelt CM, Maihofer AX, Klengel T, Atkinson EG, Chen C-Y, Choi KW et al (2019) International meta-analysis of PTSD genome-wide association studies identifies sex- and ancestry-specific genetic risk loci. Nat Commun 10:4558. https://doi.org/10.1038/s41467-019-12576-w
Yu D, Sul JH, Tsetsos F, Nawaz MS, Huang AY, Zelaya I et al (2019) Interrogating the genetic determinants of tourette’s syndrome and other tic disorders through genome-wide association studies. Am J Psychiatry 176:217–227. https://doi.org/10.1176/appi.ajp.2018.18070857
Grotzinger AD, Singh K, Miller-Fleming TW, Lam M, Mallard TT, Chen Y et al (2023) Transcriptome-wide structural equation modeling of 13 major psychiatric disorders for cross-disorder risk and drug repurposing. JAMA Psychiat 80:811–821. https://doi.org/10.1001/jamapsychiatry.2023.1808
Acknowledgements
We extend our gratitude to Sarita Silveira, Hannah Matthaeus, Juliane Domke, Noemi Duroux, Ella Heinz, Karen Joachim, Alina Panzel, Eva Kellmann, Sarah Koop, Carmen Martinez Moura and the entire team at Social Neuroscience Lab for their help in organizing, preparing and collecting the data for this project.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study forms part of the CovSocial Project, headed by T.S. (principal investigator) and funded in majority by funds from the Social Neuroscience Lab of the Max Planck Society. Data for this project were collected between 2020 and 2021 at the Max Planck Social Neuroscience Lab in Berlin. T.S., together with five other cooperation partners, received a kickoff grant for the CovSocial Project in 2020, funded through the Berlin University Alliance (BUA) as part of the Excellence Strategy of the German federal and state governments [Grant agreement number 114_GC_Pandemie_23]. Genotyping has been supported by funds from the Dept. Genes and Environment, MPI Psychiatry (EBB) and was performed by the Core Facility Genomics of the Helmholtz Center Munich.
Author information
Authors and Affiliations
Contributions
Conceptualization: all authors; Coordination of data assessment and curation: Malvika Godara, Tania Singer; Formal analysis and investigation: Alicia Schowe, Malvika Godara; Methodology: Alicia Schowe, Malvika Godara; Supervision: Tania Singer, Darina Czamara, Elisabeth Binder; Writing—original draft: Alicia Schowe; Writing—review and editing: all authors; Funding acquisition: Tania Singer, Elisabeth Binder. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Institutional review board statement
The study was approved by the Ethics Committee of Charité—Universitätsmedizin Berlin (#EA4/172/20 and #EA1/345/20) and was conducted in accordance with the Declaration of Helsinki.
Informed consent
All participants provided written informed consent prior to participation.
Supplementary Information
Below is the link to the electronic supplementary material.
406_2024_1795_MOESM2_ESM.docx
Online Resource 2: CovSocial study design, questionnaire items, and generation of the resilience-vulnerability trajectories (DOCX 224 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schowe, A.M., Godara, M., Czamara, D. et al. Genetic predisposition for negative affect predicts mental health burden during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci (2024). https://doi.org/10.1007/s00406-024-01795-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00406-024-01795-y