Abstract
Vitamin deficiency syndromes and blood–brain barrier (BBB) dysfunction are frequent phenomena in psychiatric conditions. We analysed the largest available first-episode schizophrenia-spectrum psychosis (FEP) cohort to date regarding routine cerebrospinal fluid (CSF) and blood parameters to investigate the association between vitamin deficiencies (vitamin B12 and folate) and BBB impairments in FEP. We report a retrospective analysis of clinical data from all inpatients that were admitted to our tertiary care hospital with an ICD-10 diagnosis of a first-episode F2x (schizophrenia-spectrum) between January 1, 2008 and August 1, 2018 and underwent a lumbar puncture, blood-based vitamin status diagnostics and neuroimaging within the clinical routine. 222 FEP patients were included in our analyses. We report an increased CSF/serum albumin quotient (Qalb) as a sign of BBB dysfunction in 17.1% (38/222) of patients. White matter lesions (WML) were present in 29.3% of patients (62/212). 17.6% of patients (39/222) showed either decreased vitamin B12 levels or decreased folate levels. No statistically significant association was found between vitamin deficiencies and altered Qalb. This retrospective analysis contributes to the discussion on the impact of vitamin deficiency syndromes in FEP. Although decreased vitamin B12 or folate levels were found in approximately 17% of our cohort, we found no evidence for significant associations between BBB dysfunction and vitamin deficiencies. To strengthen the evidence regarding the clinical implications of vitamin deficiencies in FEP, prospective studies with standardized measurements of vitamin levels together with follow-up measurements and assessment of symptom severity in addition to CSF diagnostics are needed.
Similar content being viewed by others
Background
Schizophrenia represents a broad clinical entity that is currently operationalized by symptoms and patterns of course. An increasing body of scientific evidence suggests that routine cerebrospinal fluid (CSF) analyses in patients with psychosis not only serve to detect a possible diagnosis of autoimmune encephalitis, but could also reveal underlying inflammatory or infectious processes [1]. Accordingly, a recommendation for a lumbar puncture in first-episode schizophrenia-spectrum psychosis (FEP) patients when an underlying somatic condition is suspected, is being implemented by national schizophrenia guidelines [2]. A more thorough CSF-based screening including neuronal autoantibodies of all patients with FEP has been suggested in light of recent findings [3]. Neurodegenerative processes or processes of failed neuronal regeneration [4] develop at least partially as a consequence of inflammatory responses [5]. In this specific context, a recent meta-analysis reported a higher rate of blood–brain barrier (BBB) disruption in schizophrenia than in healthy controls [6]. However, the role of BBB dysfunctions in schizophrenia’s aetiological process remains elusive [7]. Nonetheless, given the association between BBB dysfunctions and pathomechanisms implicated in the development of schizophrenia, such as disrupted glutamatergic signalling or inflammation, it can be speculated that BBB integrity, or lack thereof, might play an important role in the pathogenesis of schizophrenia and potentially psychotic disorders in general. [7, 8]. CSF is a secretion that may contain key information regarding inflammatory processes of the brain and BBB integrity. The CSF/serum albumin quotient (Qalb) is usually used as an indicator of BBB integrity [9], although it has limited differential power since it can be affected in both neuroinflammatory and cerebrovascular diseases. However, an increased Qalb is generally discussed to be a reliable sign of an active pathological process [10]. Increased levels of Qalb have been reported in psychotic disorders, indicating an impairment of BBB in these conditions [7]. Previous studies with a high number of individuals found an increased Qalb in about 16% of all FEP patients [11, 12]. In this context, vitamins might play a salient role since they are implicated in the biosynthesis of proteins which promote neuronal growth and repair. Deficiency of vitamin B12 leads to an inactivation of methionine synthase and mitochondrial methylmalonyl-CoA mutase and subsequently to the accumulation of homocysteine (Hcy) and methylmalonic acid (MMA) [13]. Hcy is a pro-inflammatory endogenous amino acid formed by the demethylation of nutritional methionine and is mostly re-methylated to methionine which requires folate as a methyl donor and vitamin B12 as a cofactor [13]. Hcy is an agonist of the neuronal N-methyl-D-aspartate receptor (NMDAr) [14]. It has been suggested that an NMDAr-dependent mechanism is involved in reducing the expression of the tight junction protein claudin-5 in brain microvascular endothelial cells, consequently promoting BBB disruption [15]. In summary, decreased levels of both vitamin B12 and folate increase levels of Hcy, which in turn could promote BBB alterations. From a pathophysiological perspective, there is evidence that certain vitamin and mineral deficiencies might be associated with an increased risk of developing schizophrenia [16,17,18,19], which might in part be related to compromise BBB integrity. Notably, the Prenatal Determinants of Schizophrenia (PDS) study analysed banked sera from a US cohort of mothers during pregnancy and could demonstrate that an elevated third-trimester Hcy level (which is inversely related to folate) was associated with a twofold increase in schizophrenia risk in offspring [20]. Moreover, serum indicators of reduced vitamin D and B in patients with schizophrenia have been found to hold significant associations with illness severity and in particular with regard to negative symptoms [17, 21]. Furthermore, these vitamin deficiencies relate to neuropsychological abnormalities observed in schizophrenia, such as hippocampal volume loss and cognitive impairments [21, 22]. The association between vitamin deficiencies (folate, B12) and the integrity of the BBB in schizophrenia remains to be investigated, especially in the light of a small study (n = 30) among patients with mild cognitive impairment and hyperhomocysteinemia, in which a vitamin B12-B6-folate combination appeared to improve BBB function [23]. In line with this finding, a recent randomized clinical trial among FEP patients (n = 120), showed that a 12-week B-vitamin supplementation may protect from cognitive decline especially in the attention and vigilance domains, particularly in patients with elevated homocysteine levels, patients with affective psychosis, and female patients [24]. Taken together, these findings show that a personalized medicine approach that considers vitamin supplementation in FEP might be beneficial [24]. With regard to patients with chronic schizophrenia, folate plus vitamin B12 supplementation improved negative symptoms in a randomized clinical trial (n = 140), even though treatment response was influenced by genetic variation in folate absorption [25]. In a recent meta-analysis, pooled effects showed that vitamin B supplementation (including B6, B8 and B12) reduced psychiatric symptoms significantly more than control conditions [26]. In summary, BBB abnormalities are present in at least a subgroup of FEP patients and there is evidence that vitamin deficiencies could result in BBB disruption. Therefore, we aimed to investigate the association between BBB alterations, using Qalb as a proxy, and serum vitamin B12 and folate deficiencies in a cohort of FEP patients.
Methods
Data extraction
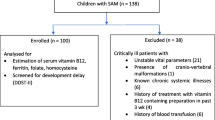
In this retrospective study, we extracted data collected between 01/01/2008 and 01/08/2018 from our digital and physical medical records at the Department of Psychiatry and Psychotherapy (LMU University Hospital, Munich, Germany). Records were individually screened and data were manually extracted by two authors independently (MC, EW) using the following inclusion criteria:
-
Inpatients
-
At least one admission in our tertiary care hospital
-
ICD-10 diagnosis of a first-episode F2x (schizophrenia-spectrum). In this context, patients admitted with a diagnosis of drug-induced FEP, which subsequently received a schizophrenia-spectrum diagnosis within the above mentioned time period for the analyses, were also included
-
Available data for CSF/serum albumin quotients and at least one assessment of vitamin levels (folate or vitamin B12) within 60 days around the time point of the lumbar puncture
Medical records of patients suggesting clinical signs of a possible underlying autoimmune encephalitis (based on careful screening of all available data on clinical and physical examinations) were excluded from our analysis. This retrospective study was approved and informed consent was waived by the Ethics committee of the Faculty of Medicine (Ludwig-Maximilian University, Munich, Germany, registration number: 18–570). The study was performed in accordance with all applicable regulatory and ethical requirements.
CSF and blood-based vitamin levels
Included patients received CSF and blood diagnostics within the clinical routine in the Department of Psychiatry and Psychotherapy. All CSF and blood analyses were conducted at the Institute of Laboratory Medicine (University Hospital, LMU Munich, Munich, Germany). Laboratory analyses comprised CSF cell counts, albumin levels in both CSF and serum and their ratio (Qalb), IgG levels in CSF and serum and their ratio, total protein in CSF and oligoclonal bands (OCBs) in both CSF and serum. Qalb values were classified as altered when outside the reference values. Reference values were adjusted by age with the following formula: Qalb = (4 + age/15) × 10–3, age indicated as years [27]. In accordance with other publications [12, 28], OCBs were classified in five pattern types as recommended by previous reports [29, 30]. The five patterns are defined as follows: pattern 1: normal CSF, pattern 2: multiple CSF restricted OCBs, pattern 3: identical OCBs in CSF and serum plus CSF restricted OCBs, pattern 4: identical OCBs in both CSF and serum, pattern 5: monoclonal bands in CSF and serum. An intrathecal synthesis of IgG is characterized by OCB patterns 2 or 3. Folate and vitamin B12 were measured according to the manufacturer’s instructions in serum/heparinized plasma samples using electrochemiluminiscent competitive binding assays on a Roche Elecsys 411e analyzer and a Roche Cobas e602 module (Roche Diagnostics GmbH, D-68305 Mannheim, Germany), respectively. The Roche Elecsys Folate and Elecsys vitamin B12 assays make use of a ruthenium labelled folate/intrinsic factor binding protein and biotin labelled folate/vitamin B12 as tracer. Vitamin B12 and folate levels were rated as decreased or not decreased according to cut-offs used by the Institute of Laboratory Medicine (Folate cut-off ≥ 4.6 ng/ml, vitamin B12 cut-off ≥ 250 pg/ml). Vitamin B12 cut-off was not adjusted for age, reference values for folate levels were age-adjusted (see Table 1). Over the selected time period for the analyses reported in this manuscript (01/01/2008 and 01/08/2018), the Institute of Laboratory Medicine used different folate and vitamin B12 reference values. In a pragmatic approach, we applied a single reference cut-off for vitamin B12 (250 pg/ml) as well as for folate (4.6 ng/ml) which are both broadly applied in the literature [31, 32]. In 11 cases, absolute values for vitamin B12 and folate were not specified since minimal and maximal cut-offs were exceeded. In order to provide an estimate of these absolute vitamin B12 and folate values in our cohort, we considered values smaller than the lower cut-offs (n = 2) as being equal in value to the lower cut-off (vitamin B12 < 150 pg/ml and folate < 2 ng/ml) and, similarly, values greater than the upper reference (n = 9) as being equal in value to the upper reference (folate > 20 ng/ml or folate > 24 ng/ml).
Brain magnetic resonance imaging (MRI)
As part of the diagnostic clinical routine, a brain MRI is usually offered to every FEP patient admitted in our Department of Psychiatry and Psychotherapy. We examined the neuroradiological evaluation reported in the patient medical files and recorded brain MRI pathologies if they included any alterations uncommon for the patient’s age group. Recorded brain MRI pathologies included non-specific WML and lesions suggestive of multiple sclerosis (MS). Every routine MRI protocol comprised T1-weighted and T2-weighted sequences (1.5 and 3 Tesla scanners). Furthermore, additional DWI (axial) and FLAIR (coronal) sequences were performed if indicated by an experienced neuroradiologist.
Groups comparison
Patients included in our analyses were divided in two sub-groups based on vitamin status. Both demographic and clinical variables were compared between patients with vitamin B12 OR folate serum levels under the cut-off values and patients with vitamin B12 AND folate serum levels within reference range.
Statistical analyses
Analyses were executed using IBM SPSS version 28.0 for Windows. The significance level was set at α = 0.05. Descriptive statistics included frequencies, sum, mean and standard deviation (SD). All these parameters were applied for continuous variables and frequencies were applied to present dichotomous variables. Chi-square tests were applied to compare differences in categorical variables between groups (two-sided Fisher’s exact test was applied for cell count < 5 for 2 × 2 tables). Cramer’s V tests were adopted to test for possible associations between categorical variables. Continuous variables were tested for normality with Kolmogorov–Smirnov tests, a violation of the normal distribution was defined as p < 0.05. Mann–Whitney-U tests were used to compare differences between continuous non-parametric variables. The following results must be considered exploratory since they include multiple different statistical analyses that were not corrected for multiple testing.
Results
Characterization of our cohort
A total of n = 222 FEP patients were included in our cohort. Mean age was 34.9 years (SD = 15.8), with 53.6% (n = 119) male and 46.4% (n = 103) female patients. All of the included patients received a diagnosis in the schizophrenia-spectrum (F2x according to ICD-10), whereby almost half of the sample (46.4%, n = 103) received a diagnosis of schizophrenia (F20 according to ICD-10). The mean duration of illness between onset of first symptoms and lumbar puncture was 13.4 months (SD = 25.4, n = 140). 69.1% (n = 145) of the patients were treated with one (first- or second generation) antipsychotic and 27.6% (n = 58) received two or more antipsychotics. Half of the cohort (51.5%, n = 105) had a first and/or second-degree relative with a psychiatric condition. 34.4% (n = 74) of the patients were active smokers while 29.2% (n = 64) of the patients showed active drug abuse of at least one substance other than tobacco. Among them, 16.7% (n = 37) consumed cannabis anywhere from sporadically to daily. A small number of patients (9.9%, n = 22) were diagnosed with concurrent neurological disorders, while in 3.6% of cases (n = 8) a gastrointestinal disorder was reported (for further details please refer to Table S1). Less than 5% of patients (4.5%, n = 10) were diagnosed with diabetes type I or II. 15.5% (n = 34) presented a diagnosis of a concomitant cardiovascular condition. Finally, 8.2% (n = 18) of the patients were diagnosed with cancer (active or in remission) and 8.1% (n = 18) were diagnosed with a lung disease (see Table 1).
Vitamin B12, folate and CSF parameters
Among the n = 222 patients who received a vitamin B12 assessment, the mean vitamin B12 serum level was 481.98 pg/ml (SD = 261.9). A total of n = 217 patients received a folate assessment with mean folate serum levels of 9.46 ng/ml (SD = 4.7). n = 23 (10.4%) patients showed decreased vitamin B12 serum levels. Similarly, n = 24 (11.1%) patients presented decreased folate serum levels. For patients younger than 18 years (n = 5), no folate reference values were used by the laboratory. Nevertheless, their mean folate value was 8.78 ng/ml (SD = 5.0) and thus above the adult cut-off value (4.6 ng/ml). Mean albumin CSF level was 0.25 g/l (SD = 0.1) with a mean Qalb of 5.47 (SD = 2.4). 17.1% (n = 38) of the 222 patients showed an altered age-adjusted Qalb. Mean IgG CSF levels were 0.03 g/l (SD = 0.02) with a mean IgG CSF/serum ratio of 2.79 (SD = 2.1). Total CSF protein level was 0.38 g/l (SD = 0.27) whereas the mean number of cells in CSF was 1.58/µL (SD = 1.9). Among patients tested for OCBs both in CSF and serum (n = 171), n = 124 patients (72.5%) showed no OCBs (pattern 1), n = 5 patients (2.9%) showed OCBs pattern 2, OCBs pattern 3 were present in n = 14 patients (8.2%) while OCBs pattern 4 were reported in n = 28 patients (16.4%). No OCBs pattern 5 were found in our cohort (see Table 1).
Brain MRI
Brain MRI data were available for a total of n = 212 patients. Any brain MRI abnormal findings were detected in n = 85 (40.1%) patients. WMLs were present in n = 62 (29.3%) cases, with 1.9% (n = 4) cases having lesions suggestive of MS (see Table 1).
Comparison of demographical and clinical variables according to vitamin status
A detailed comparison of demographical and clinical variables between patients with vitamin B12 or folate serum levels under the cut-off values and patients with vitamin B12 and folate serum levels within reference values can be found in Table 1. Overall, no statistically significant differences were found when comparing the two groups. Of note, there was no significant difference when comparing altered Qalb between groups (df = 1, Cramer’s V = 0.12, p = 0.103). Similarly, no significant difference was found when comparing for WMLs rate between groups (\(\chi_{(1)}^{2}\) = 1.29, Cramer’s V = 0.08, p = 0.256) (see Table 1).
Discussion
To our knowledge, this is the largest FEP cohort with a schizophrenia-spectrum disorder having received CSF diagnostics and vitamin B12 and folate serum assessments. The aim of this investigation was to explore the relationship between BBB dysfunction represented by altered age-adjusted Qalb and vitamin B12 and folate serum levels in FEP patients. The cohort presented here was part of a larger clinical population, that was previously described by our research group [12]. Corresponding to the aforementioned cohort, we report signs of BBB dysfunction (increased Qalb) in 17.1% of the included population. Moreover, a relatively small percentage of the cohort showed decreased vitamin B12 or folate serum levels (10.4% and 11.1% respectively). Put in perspective with data from healthy controls of similar age [33], only 1.0% of omnivores (5.7% of vegetarians and 7.5% of vegans) presented decreased vitamin B12 levels. Nevertheless, in the healthy control cohort a lower vitamin B12 cut-off was applied (150 pg/ml) than in our FEP analyses (250 pg/ml), which could explain the large difference in the prevalence of vitamin B12 deficiency. In the aforementioned study among healthy subjects [33], decreased folate serum levels were reported in 58% of omnivores (30.2% of vegetarians and 13.2% of vegans), a greatly higher level than the 11.1% reported in our cohort, although the cut-off used in the aforementioned publication was set at 6.6 ng/ml and thus higher than the one used in our approach (4.6 ng/ml). As mentioned before, definitions for vitamin B12 and folate deficiency are highly heterogeneous and might explain the heterogeneity in the prevalence of hypovitaminoses across the literature. In this context, it must be noted that confounding factors such as nutritional and lifestyle habits or body-mass-index were not recorded, so that it remains difficult to pinpoint a cause for the higher prevalence of vitamin B12 deficiency and the reduced prevalence of decreased folate levels in our cohort compared to the healthy control cohort. When assessing the relation between BBB dysfunction and vitamin B12 or folate deficiency, no statistically significant association could be found. Nevertheless, a potential causal relationship between BBB disruption and vitamin deficiencies cannot be excluded based on our cross-sectional retrospective data.
In our cohort, the mean duration of illness was 13.4 months, which could imply that not all patients with a vitamin B12 deficiency already had low vitamin B12 serum levels at an early disease stage. It is known that a vitamin B12 deficiency can be preclinical for more than 3–5 years [34], thus the results have to be interpreted with caution. Further investigation is needed to evaluate the course of especially FEP patients and vitamin B12 levels, starting with the prodromal stage of psychosis and following the course of the disease.
When assessing brain MRI data, we found alterations in 40.1% of patients. A much lower rate than the approximately 70% reported in another large cohort which was not restricted to FEP patients [11]. In our cohort we report WMLs in 29.3% of brain MRI scans. As a reference for comparison: WMLs occurred in around 5.3% of healthy controls with a similar mean age [35]. We found no statistically significant association between WMLs occurrence and increased Qalb levels as the pathogenesis of WMLs remains controversial and in need of more appropriate investigations [36].
A major limitation of the present study is its retrospective design. As a consequence, several patients did not receive all assessments included in this analysis. Thus, from a cohort of initially 687 FEP patients, only 222 underwent a lumbar puncture as part of the clinical routine and received an assessment of vitamin B12 and folate levels within 60 days prior or following a lumbar puncture. Hypotheses for the lack of CSF diagnostics in a substantial part of the cohort are difficult to test retrospectively, whereas vitamin B12 and folate deficiencies are rarely examined in general and rather have the status of optional examinations. This is astonishing, since there is evidence that supplementation of certain vitamins may reduce psychiatric symptoms in people with schizophrenia [26]. Of note, the assessment of vitamin B12 and folate serum levels among FEP patients is currently suggested as facultative in some guidelines [37] or completely omitted in others [38]. Moreover, in a few cases absolute values for vitamin B12 and folate were missing in our analyses, since these values were not specified when minimal and maximal cut-offs were exceeded. Since different cut-offs for vitamin B12 and folate levels were used in our tertiary care hospital during the period of interest, we used a pragmatic approach for our analyses. Of note, applying different reference values with lower cut-offs would not have a substantial impact on the results of our comparison analyses. Furthermore, a vitamin B12 deficiency syndrome can be associated with normal vitamin B12 serum levels. Around 80% of the circulating biomarker vitamin B12, determined in the serum is protein-bound to haptocorrin and therefore not bioavailable for cellular uptake [39]. In addition, the serum and cellular levels of vitamin B12 differ, so that the diagnostic value of a serum sample is reduced [39]. Nevertheless, serum B12 remains a valuable biomarker to better characterize the prognosis and status of several diseases [40], but it has a limited diagnostic value as a stand-alone biomarker. Complementing the diagnostics of a vitamin B12 deficiency through assessment of serum holotranscobalamin and MMA can increase the sensitivity in assessing a sub-clinical functional vitamin B12 deficiency [41] and should be considered in future studies. This could be particularly important for FEP cohorts, since a functional B12 deficiency may be present even if it cannot be detected by measuring vitamin B12 serum levels alone. Given the association between reduced vitamin D and illness severity [21], a more thorough assessment of the vitamin status might be recommended for future clinical practice. However, among the selected population only data regarding vitamin B12 and folate were available. For this reason, determining the status of other key vitamins was not possible. Given the retrospective design of this study, it was not possible to determine whether patients presenting a B12 or folate deficiency received any vitamin supplementation. Although lumbar punctures were performed within days of the vitamin assessment, a possible role of supplementation in offsetting a potential BBB dysfunction cannot be ruled out. It is important to mention the relative inhomogeneity regarding characteristics, e.g. age and comorbidities in our cohort. This is due to the retrospective study design with a large sample size, hence a broader and less fine selected patient’s population is assessed which ultimately better represents real world settings. Finally, no information were available regarding symptom severity as measured by standardized questionnaires, limiting the investigation of possible correlations between biological markers and impairments in different symptom domains.
In summary, our study contributes to an increased knowledge about vitamin deficiencies in FEP patients. To draw potential associations between vitamin deficiencies and symptoms severity, prospective studies are needed. We recommend that these studies should employ CSF diagnostics beyond the clinical routine, standardized (follow-up) measurements of vitamin levels as well as assessments of cognitive functioning and symptom severity to further foster the evidence with regard to the prevalence and clinical implications of vitamin deficiency syndromes in FEP. Overall, this study provides epidemiological evidence regarding vitamin deficiencies and BBB dysfunctions in first-episode schizophrenia-spectrum psychosis. We believe this work could raise awareness on this important topic and pave the way for prospective implementation of vitamin assessments in the clinical practice and especially in the diagnostic algorithms of psychosis.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BBB:
-
Blood-brain barrier
- CSF:
-
Cerebrospinal fluid
- FEP:
-
First-episode schizophrenia-spectrum psychosis
- Hcy:
-
Homocysteine
- MMA:
-
Methylmalonic acid
- MRI:
-
Brain magnetic resonance imaging
- MS:
-
Multiple sclerosis
- NMDAr:
-
N-methyl-D-aspartate receptor
- OCBs:
-
Oligoclonal bands
- PDS:
-
Prenatal determinants of schizophrenia
- Qalb:
-
Cerebrospinal fluid /serum albumin quotient
- WML:
-
White matter lesions
References
Pollak TA, Lennox BR (2018) Time for a change of practice: the real-world value of testing for neuronal autoantibodies in acute first-episode psychosis. BJPsych Open 4(4):262–264
Hasan A et al (2020) Schizophrenia. Dtsch Arztebl Int 117(24):412–419
Lennox BR et al (2017) Prevalence and clinical characteristics of serum neuronal cell surface antibodies in first-episode psychosis: a case-control study. Lancet Psychiatry 4(1):42–48
Falkai P et al (2015) Kraepelin revisited: schizophrenia from degeneration to failed regeneration. Mol Psychiatry 20(6):671–676
Ransohoff RM (2016) How neuroinflammation contributes to neurodegeneration. Science 353(6301):777–783
Orlovska-Waast S et al (2019) Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol Psychiatry 24(6):869–887
Pollak TA et al (2018) The blood-brain barrier in psychosis. Lancet Psychiatry 5(1):79–92
The Network and Pathway Analysis Subgroup of Psychiatric Genomics Consortium (2015) Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nat Neurosci 18(2):199–209
Deisenhammer F et al (2006) Guidelines on routine cerebrospinal fluid analysis. Report from an EFNS task force. Eur J Neurol 13(9):913–922
Jesse S et al (2011) Summary of cerebrospinal fluid routine parameters in neurodegenerative diseases. J Neurol 258(6):1034–1041
Endres D et al (2020) Cerebrospinal fluid, antineuronal autoantibody, EEG, and MRI findings from 992 patients with schizophreniform and affective psychosis. Transl Psychiatry 10(1):279
Campana M et al (2021) Cerebrospinal fluid pathologies in schizophrenia-spectrum disorder-A retrospective chart review. Schizophr Bull 48:47–55
Combs GF (2012) Chapter 17—Vitamin B12. In: Combs GF (ed) The Vitamins. Elsevier, The Netherlands, pp 377–394
Lipton SA et al (1997) Neurotoxicity associated with dual actions of homocysteine at the N-methyl-D-aspartate receptor. Proc Natl Acad Sci USA 94(11):5923–5928
Beard RS, Reynolds JJ, Bearden SE (2011) Hyperhomocysteinemia increases permeability of the blood-brain barrier by NMDA receptor-dependent regulation of adherens and tight junctions. Blood 118(7):2007–2014
Yanik M et al (2004) Plasma manganese, selenium, zinc, copper, and iron concentrations in patients with schizophrenia. Biol Trace Elem Res 98(2):109–117
Kale A et al (2010) Reduced folic acid, vitamin B12 and docosahexaenoic acid and increased homocysteine and cortisol in never-medicated schizophrenia patients: implications for altered one-carbon metabolism. Psychiatry Res 175(1–2):47–53
Valipour G, Saneei P, Esmaillzadeh A (2014) Serum vitamin D levels in relation to schizophrenia: a systematic review and meta-analysis of observational studies. J Clin Endocrinol Metab 99(10):3863–3872
Cao B et al (2016) Lower folate levels in schizophrenia: a meta-analysis. Psychiatry Res 245:1–7
Brown AS et al (2007) Elevated prenatal homocysteine levels as a risk factor for schizophrenia. Arch Gen Psychiatry 64(1):31–39
Graham KA et al (2015) Relationship of low vitamin D status with positive, negative and cognitive symptom domains in people with first-episode schizophrenia. Early Interv Psychiatry 9(5):397–405
Shivakumar V et al (2015) Serum vitamin D and hippocampal gray matter volume in schizophrenia. Psychiatry Res 233(2):175–179
Lehmann M et al (2003) Vitamin B12-B6-folate treatment improves blood-brain barrier function in patients with hyperhomocysteinaemia and mild cognitive impairment. Dement Geriatr Cogn Disord 16(3):145–150
Allott K et al (2019) The vitamins in psychosis study: a randomized, double-blind, placebo-controlled trial of the effects of vitamins B(12), B(6), and folic acid on symptoms and neurocognition in first-episode psychosis. Biol Psychiatry 86(1):35–44
Roffman JL et al (2013) Randomized multicenter investigation of folate plus vitamin B12 supplementation in schizophrenia. JAMA Psychiat 70(5):481–489
Firth J et al (2017) The effects of vitamin and mineral supplementation on symptoms of schizophrenia: a systematic review and meta-analysis. Psychol Med 47(9):1515–1527
Trendelenburg C (1994) Labormedizinische Spezialbefundung und ärztliche Verantwortung. Laboratoriumsmedizin 18:545–551
Bernitsas E et al (2017) Cerebrospinal fluid humoral immunity in the differential diagnosis of multiple sclerosis. PLoS ONE 12(7):e0181431
Andersson M et al (1994) Cerebrospinal fluid in the diagnosis of multiple sclerosis: a consensus report. J Neurol Neurosurg Psychiatry 57(8):897–902
Freedman MS et al (2005) Recommended standard of cerebrospinal fluid analysis in the diagnosis of multiple sclerosis: a consensus statement. Arch Neurol 62(6):865–870
Ferraro S, Panzeri A, Panteghini M (2017) Tackling serum folate test in European countries within the health technology assessment paradigm: request appropriateness, assays and health outcomes. Clin Chem Lab Med 55(9):1262–1275
Cobalamin RC (2014) Vitamin B12, in Modern Nutrition in Health and Disease 11th ed., C.B. Ross AC, Cousins RJ, Tucker KL, Ziegler TR, (Editor), Lippincott Williams & Wilkins, Baltimore, 369–89.
Schupbach R et al (2017) Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur J Nutr 56(1):283–293
Johnson, L. Vitamin B12 Deficiency. 2020.
Hopkins RO et al (2006) Prevalence of white matter hyperintensities in a young healthy population. J Neuroimaging 16(3):243–251
Lin J et al (2017) Multiple factors involved in the pathogenesis of white matter lesions. Biomed Res Int 2017:9372050
(DGPPN) Deutsche Gesellschaft für Psychiatrie und Psychotherapie (2019) S3-Leitlinie Schizophrenie. AWMF-Register Nr. 038–009. www.awmf.org/leitlinien/detail/ll/038-009.html.
(2014) Psychosis and Schizophrenia in Adults: Treatment and Management. NICE Clinical Guideline 178, http://www.nice.org.uk/guidance/cg178/evidence/cg178-psychosis-and-schizophrenia-in-adults-full-guideline3, 2014.
Hannibal L et al (2016) Biomarkers and Algorithms for the Diagnosis of Vitamin B12 Deficiency. Front Mol Biosci 3:27
Arendt JF et al (2016) Elevated plasma vitamin B12 levels and cancer prognosis: a population-based cohort study. Cancer Epidemiol 40:158–165
Herrmann W et al (2003) Functional vitamin B12 deficiency and determination of holotranscobalamin in populations at risk. Clin Chem Lab Med 41(11):1478–1488
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed extensively to the work presented in this paper. M. C., L. L., E. W., designed the study, collected and analysed data, wrote the main paper. J. S., P. F., S. M., T. O. collected and analysed data. A. H., P. F., P. E., I. M., F. R., J. M. contributed extensively supervising data analysis and in writing the paper.
Corresponding author
Ethics declarations
Conflict of interest
M. Campana, L. Löhrs, J. Strauß, S. Münz, P. Fernando, T. Oviedo-Salcedo, I. Maurus, F. Raabe, J. Moussiopoulou and P. Eichhorn report no conflicts of interest. E. Wagner has been invited to Recordati advisory board meetings. P. Falkai was honorary speaker for Janssen-Cilag, Astra-Zeneca, Eli Lilly, Bristol Myers-Squibb, Lundbeck, Pfizer, Bayer Vital, SmithKline Beecham, Wyeth, and Essex. During the last 5 years, but not presently, he was a member of the advisory boards of Janssen, AstraZeneca, Eli Lilly, and Lundbeck. A. Hasan has been invited to scientific meetings by Lundbeck, Janssen-Cilag, and Pfizer, and he received paid speakerships from Janssen, Recordati, Otsuka and Lundbeck. He was a member of Roche, Otsuka, Lundbeck, Rovi, Recordati and Janssen advisory boards.
Ethical approval and consent to participate
This retrospective study was approved by the university ethics committee (registration number: 18–570).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Campana, M., Löhrs, L., Strauß, J. et al. Blood–brain barrier dysfunction and folate and vitamin B12 levels in first-episode schizophrenia-spectrum psychosis: a retrospective chart review. Eur Arch Psychiatry Clin Neurosci 273, 1693–1701 (2023). https://doi.org/10.1007/s00406-023-01572-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-023-01572-3