Abstract
Purpose
To evaluate postoperative pain and discomfort after parotid surgery with regard to different surgical approaches.
Methods
This clinical study was carried out at a single tertiary referral center (2021–2022) and included 2 groups of adult patients (mean age 56.6 ± 12.7 vs. 53.4 ± 14.1 years) following elective parotid surgery due to a parotid tumor of any entity. The first group (SP/TP group) consisted of 31 patients after superficial parotidectomy (SP) or total parotidectomy (TP) (n = 31). The second group (ECD group) included all patients who had undergone extracapsular dissection (ECD) (n = 51). Primary endpoints comprised pain on ambulation as well as maximum and minimum pain (NRS 0–10) on the first three postoperative days (PODs). A neuropathic pain component (evaluated on POD 1 and 3), the analgesic score (collected from the patient file on POD 1–3), treatment-related side-effects/pain-associated impairments, and patient satisfaction (all measured on the 1st POD) were defined as secondary endpoints.
Patients were surveyed using the standardized and validated “Quality Improvement in Postoperative Pain Treatment” (QUIPS) questionnaire and the painDETECT® questionnaire. Comparisons were performed using independent t tests, Wilcoxon tests, and χ2 tests, and the respective effect sizes were calculated.
Results
Looking at the first postoperative day, patients of both groups (SP/TP vs. ECD) reported comparable pain on ambulation (2.8 ± 2.0 vs. 2.6 ± 1.8; p = 0.628, r = 0.063), maximum (3.5 ± 2.2 vs. 3.5 ± 2.3; p = 0.992, r = 0.002) and minimum pain (1.1 ± 1.04 vs. 1.0 ± 1.2; p = 0.206, r = 0.157). Furthermore, there were no significant differences in pain-related restrictions or pain medication requirement. The patients in both groups were equally satisfied with their pain therapy (p = 0.282, R = 0.135). The sum score of the painDETECT® questionnaire delivered clearly negative (< 12) results on average (POD1: 6.81; POD3: 6.59); no significant difference between the groups was found (p = 0.991, R2 < .001).
Conclusion
Neither surgical technique on the parotid gland was significantly superior to the other in terms of postoperative pain perception. Overall, postoperative pain can be classified as mild to moderate following parotid surgery. A neuropathic pain component could be excluded for the acute postoperative phase.
Trial registration
The study was registered in the German Registry for Clinical Studies (DRKS) (application No.: DRKS00016520).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Salivary gland tumors are tumors that arise from various entities of salivary gland cells and in most cases affect the parotid gland [1]. 80% of tumors are benign and in recent years, there has been a shift from pleomorphic adenomas to Warthin tumors as the most common underlying entity [2].
The treatment of choice is the removal of the tumor. The surgical options range from minimally invasive extracapsular dissection (ECD) to superficial parotidectomy (SP) and total parotidectomies (TP) and even radical removal of the parotid gland, depending on the tumor entity being treated and the extent of the resection [3].
Partial parotidectomy is the most frequently performed surgical procedure and is mainly used to resect benign tumors. This, in turn, can be performed and classified as SP or ECD. The main difference between these surgical techniques is that in SP the main trunk of the facial nerve is visualized intraoperatively. In contrast, in ECD the main trunk is not visualized at any time. However, during many ECDs short parts of certain branches of the facial nerve can be visualized during dissection through the parotid tissue [3]. This means that less glandular tissue is removed during ECD, making it a potentially gentler and less risky procedure, and continuing the trend towards minimally invasive surgery [3,4,5,6,7,8] with no drawbacks regarding oncologic safety [4, 9].
Despite great efforts to standardize the surgical procedures in parotid surgery, the extent of acute postoperative pain and an evaluation of analgesic therapy comparing different surgical approaches have hardly been investigated to date. Standards have not yet been established and the implementation of existing recommendations is insufficient [10, 11].
Moreover, postoperative pain therapy in general is often inadequate at present [12,13,14,15,16].
According to the German S3-consensus guideline “Treatment of acute perioperative and post-traumatic pain”, the postoperative pain intensity after surgery on the parotid glands is expected to be "moderate" [17]. We hypothesize that the minimally invasive technique (ECD) is beneficial in terms of postoperative pain levels.
Therefore, the aim of this planned study was to examine and compare the postoperative pain and actual symptom burden of patients after ECD and SP/TP. Furthermore, we intended to evaluate a potential neuropathic pain component and investigate the analgesic medication within a standardized acute pain therapy plan.
Material and methods
This prospective clinical study was approved by the Ethics Committee of the xxx (approval number 374_18 B). It was conducted according to the Declaration of Helsinki and followed the STROBES guidelines [18] as well as the guidelines of the “Quality Improvement in Postoperative Pain Treatment” (QUIPS) registry [19]. The study was registered in the German Clinical Trial Register (DRKS00016520). A total of 82 patients, who presented for elective salivary gland surgery at the xxx between March 29, 2021, and March 18, 2022, were included.
Inclusion criteria were defined as follows: surgery on the parotid gland due to a parotid mass irrespective of the clinically suspected dignity, written consent to data collection and processing, minimum age of 18 years, sufficient cognitive and verbal ability to understand the content of the questionnaires, an American Society of Anesthesiologists (ASA) status of I–III. and a body mass index (BMI) ≥ 19 kg/m2.
Patients were excluded who were undergoing revision surgery or radical parotidectomy, who did not provide written informed consent or who had undergone major skin resections with subsequent flap reconstruction or concomitant resections of the auditory canal or temporal bone. In addition, all patients who had not been treated postoperatively according to the standardized pain protocol of the Department of Otolaryngology were excluded from the statistical analysis.
The patient collective was divided into two groups. The first group (referred to below as SP/TP group) consisted of patients in whom the trunk of the facial nerve had been primarily exposed during surgery, i.e. superficial or total parotidectomy (n = 31). The second group (referred to below as ECD group) included all patients who had undergone extracapsular dissection (ECD) (n = 51). Assignment to the respective group was based on the surgical report. As the surgeons did not know before or during the operation whether the patient was a study participant, the choice of surgical technique was left to the surgeon’s discretion.
In all patients, anesthesia was induced according to the current department standard (fentanyl 1–2 µg/kg bodyweight (bw), propofol [TCI (target-controlled infusion) plasma level 4–8 ng/ml, Orchestra® Base Primea, Fresenius Kabi, Bad Homburg, Germany, plasma mode, Marsh mode), and rocuronium 0.3–0.5 mg/kg bw, intravenously (IV)]. To maintain anesthesia, plasma propofol TCI was reduced to levels between 2.5 and 4.0 ng/ml, and the strong intraoperative pain stimulus was treated with remifentanil 0.2–0.5 µg/kg/min run rate combined with fentanyl (1 µg × kg−1 bolus as required). To attenuate propofol injection pain, all patients received 40 mg lidocaine 2% IV before propofol administration.
Pain in the recovery room was treated with ibuprofen, acetaminophen, and metamizole as well as intravenous piritramide (0.05–0.2 mg × kg−1) as required up to a pain intensity of NRS (Numeric Rating Scale) < 3 to be transferred to a normal ward.
Patients on the ward were treated according to the standardized pain protocol of the Department of Otorhinolaryngology-Head and Neck Surgery, according to the WHO (World Health Organization) step-by-step scheme, if required and desired (see Supplement 1).
The standardized and validated QUIPS questionnaire ("Quality Improvement in Postoperative Pain Therapy") was used once a day during the first three postoperative days (PODs) to survey patients with regard to their pain, physical impairments, side effects of pain therapy and their general condition (so-called outcome parameters) [20]. This was supplemented by the so-called process parameters, filled out by the investigator, containing patient-relevant information, details on anesthesia and surgery, and analgesic consumption.
Moreover, all patients were screened for a neuropathic pain component using the validated 12-item painDETECT® questionnaire (PD-Q) (Pfizer Germany) on days 1 and 3. In this questionnaire, an overall score is calculated from all the patient's answers, resulting in a negative (0–12), indeterminate (13–18), or positive (19–38) screening result[21, 22].
During the daily visit patients were asked to fill out the questionnaires by themselves and were given assistance if desired. The same person performed the study inclusion, patient education, and the postoperative visits.
The documentation of demographic data as well as the completion of the QUIPS process parameter data sheet was performed by the same individual during and after the inpatient stay based on the digital and paper patient files. The data on the size of the resected tissue, measured in all 3 room levels, and the results of the histologic examination were taken from the histologic findings prepared by the Department of Pathology at the University Hospital Erlangen.
Primary endpoints were maximum and minimum pain as well as pain on ambulation (NRS 0 (“no pain”) – 10 (“worst pain imaginable”) on the first three postoperative days. Our main hypothesis was that the maximum pain on the first postoperative day would be greater in the SP/TP group. Secondary endpoints comprised a neuropathic pain component measured on POD 1 and 3 and analgesic consumption, measured on POD 1,2 and 3. Further secondary endpoints were perioperative and postoperative complications, treatment-related side-effects/pain-associated impairments, wish for more pain medication, and satisfaction with the pain therapy, measured on POD 1.
Statistical analysis
Metric variables were first checked for normal distribution using their histograms, QQ plots and Shapiro-Wilks tests.
To ensure good comparability, all metric variables were presented as median and 25th/75th percentile (Md [25th; 75th percentile]) and additionally as mean ± standard deviation (SD). Nominal variables were reported as absolute and relative frequencies [n (%)].
Independent t tests were calculated for normally distributed metric variables and Wilcoxon tests for non-normally distributed metric variables to compare the types of disaggregation. Nominal variables were tested for group differences using χ2 tests.
To test metric variables for group differences over time, robust mixed ANOVAs were performed with a 10% trim on both sides of the distribution with the between-subjects factor 'dissection type' and the within-subjects factor 'time'. This leads to the main effects (ME) "dissection type", "time" and the interaction "dissection type x time".
In the case of a significant interaction/a significant main effect, these were further differentiated in the follow-up using a robust t-test with a 10% cut-off on both sides.
For the independent t test, Cohen's d was calculated as the effect size, with d = 0.2 representing a small, 0.5 a medium and 0.8 a large effect. For the Wilcoxon test, rank-order correlation r and for the χ2 test phi/Cramer's V were reported, with r/phi/V of 0.1 representing a small, 0.3 a medium and 0.5 a large effect.
The effect size ξ2 is still reported for the effects of the robust ANOVA and for pairwise comparisons. This corresponds to the classical R2, with small, medium, and large effects, where 0.01 corresponds to a small, 0.09 to a medium and 0.25 to a large effect.
A priori power-analysis showed that a power of 0.80 could be achieved with 37 patients per group when a group difference of 1.0 and a standard deviation of 1.5 was assumed (alpha = 0.05). The actual sample size slightly differs due to practical circumstances.
The present analyses were conducted using R and the packages effectsize, effsize and WRS2 [23, 24].
Results
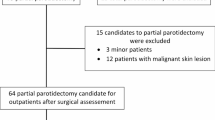
A total of 102 patients were initially included in the study. Six patients had to be excluded because of incorrectly completed questionnaires (n = 2), questionnaires not returned (n = 3), and lack of consent (n = 1). The CONSORT flowchart[25] is depicted in Fig. 1.
The statistical analysis included 31 patients in the SP/TP group and 51 patients in the ECD group.
The demographic, clinical and surgical data of all patients included are presented in Table 1. Patients of the SP/TP group had a significantly higher body mass index (BMI) (PAR vs. ECD) (29.76 kg/m2 vs. ECD 26.64 kg/m2; p = 0.015, r = 0.322), had significantly longer surgery with an incision-suture time of 216 ± 73 min vs. 88 ± 33 min (p < 0.001, d = 2.464), and resection of a significantly larger specimen (60 cm3 vs. 12 cm3; p < 0.001, r = 0.719).
The outcome measures of the QUIPS questionnaire are presented in Table 2. The analysis of the data showed no significant group differences as patients of both study groups SP/TP vs. ECD) suffered from comparable mild to moderate postoperative pain intensities on the 1st POD regarding pain on ambulation (2.81 ± 2.02 vs. 2.55 ± 1.84; p = 0.628, r = 0.063), maximum (3.45 ± 2.22 vs. 3.51 ± 2.34; p = 0.992, r = 0.002) and minimum pain (1.10 ± 1.04 vs. 0.86 ± 1.15; p = 0.206, r = 0.157). This remained stable over all three PODs (see Fig. 2).
Looking at all patients included and irrespective of the surgical technique, a significant decrease in pain on ambulation (ME time: F(2, 30.67) = 12.37, p < 0.001, ξ2 = 0.446), maximum pain (ME time: F(2, 30.96) = 3.39, p = 0.047, ξ2 = 0.180) and minimum pain (ME time: F(2, 23.59) = 7.57, p = 0.003, ξ2 = 0.391) was detected over the postoperative period surveyed. There was always a significant drop from POD 1 to 3 or POD 2 to 3. The peak of the median documented pain intensities for pain on ambulation (3 [2;4.75]), maximum pain (3 [2;4.75]) and minimum pain (2 [1;4]) was on POD 2.
Patients were equally affected by pain-associated impairments. Patients of the SP/TP group most frequently complained about painful coughing or deep inhalation (8/25.8%), while patients in the ECD group most frequently woke up from pain at night (14/27.4%).
Only 2 (6.5%) patients in the SP/TP group and 3 (5.9%) patients in the ECD group would have liked more pain medication (p = 1, V < 0.001).
Overall, patient satisfaction was high in both groups with no statistically significant difference ( SP/TP group vs. EDC-group: 8.87 ± 1.93 vs. 8.43 ± 2.28; p = 0.282, R = 0.135).
Both groups received similar medications before, during and after surgery (see Table 3). In the SP/TP group, 3.2% reported taking opioids for chronic pain prior to hospitalization, but this was not significantly different from the ECD group (0%; p = 0.800, V = 0.091). On the ward, the administration of non-opioid analgesics was sufficient for adequate pain relief. No patient required opioids. In both groups, there was a relevant but not significantly different proportion of patients who did not want any pain therapy after surgery at all (48.4% vs. 35.3%; p = 0.347, phi = 0.069).
The evaluation of the painDETECT® questionnaire to detect a neuropathic pain component resulted in a sum score of 7.23 ± 4.11 for the PAR group and 6.55 ± 4.89 for the ECD group on POD 1 (t(47.93) = 0.71, p = 0.480, ξ = 0.12). On POD 3, the mean sum score was 6.26 ± 3.86 for the SP/TP group and 6.78 ± 5.23 for the ECD group (t(47.91) = 0.70, p = 0.488, ξ = 0.11). The results are depicted in Table 4. There was no significant main effect within the ANOVA, either for type of dissection (F(1, 33.92) = < 0.01, p = 0.991, ξ2 < 0.001) or for the main effect time (F(1, 35.77) = 1.39, p = 0.245, ξ2 = 0.038). The evaluation of the sum score over time showed a significantly different development between the two groups (interaction type of dissection x time: F(1, 35.77) = 4.38, p = 0.044, ξ2 = 0.109).
The post hoc comparison showed that there was a significant decrease in symptoms for the SP/TP group (trobust = 2.23, p = 0.039, ξ2 = 0.20). In contrast, the values in the ECD group remained almost unchanged (trobust = 0.67, p = 0.506, ξ2 = 0.04) over the surveyed postoperative period.
Discussion
Depending on the cutoff point, pain after elective surgery on the parotid gland, can be classified as mild (< 4) [26] to moderate (≥ 3) [17]. In our study, the severity of postoperative pain on all three postoperative days was independent of the surgical method, although the incision-suture time was significantly longer and the extent of resection was significantly greater in the SP/TP group.
By using the painDETECT® questionnaire, we were able to rule out a neuropathic pain component in both patient groups, at least in the acute postoperative phase. We were also unable to detect any significant differences in any other outcome measures. Postoperative pain could be very well treated with non-opioid analgesics. It is of note that in the SP/TP group almost half of all patients and in the ECD group over one-third of the patients did not need any pain treatment at all.
Comparable studies on postoperative pain after parotidectomy differentiating between existing surgical techniques are rare.
Inhestern et al. were able to show in their study of 145 patients after head and neck cancer surgery that they reported a maximal pain score of 3.18 ± 2.86 (NRS) on the first postoperative day. The QUIPS questionnaire was also used for the patient survey. In the study group, however, there were only 5 patients (3%) with tumors of the salivary glands (without further differentiation). Nevertheless, the reported maximum pain levels are in good agreement with our values [27].
In 2006, Foghsgaard et al. examined 29 patients after superficial parotidectomy regarding their postoperative morbidity and showed that 3/4 of the patients complained of paresthesia in the innervation area of the auricular nerve and needed an average of 12 and 16 days to be able to resume their normal everyday activities or work. Postoperative pain levels reached their maximum with a median pain score of 3 on the visual analog scale (VAS) on postoperative day 1 and then showed a continuous decline. The analgesic medication was not further classified [28].
This is consistent with the results of our study. Although we were able to recognize a maximum pain level for all three pain categories on the second postoperative day, a decrease in the median pain values was always recorded from the 1st to the 3rd and from the 2nd to the 3rd postoperative days.
In the German S3-consensus guideline "Treatment of acute perioperative and post-traumatic pain", the expected pain intensity after parotidectomy is also classified as "moderate", as confirmed in our two study groups[17].
The only study known to us that recorded postoperative pain intensities and differentiated between different surgical techniques is a study published in 2010 by Koch et al. Instead of ECD, partial superficial parotidectomy (PSP) was compared with superficial and total parotidectomy as a less invasive procedure. The study included 429 patients. 34.3% of the patients showed medium pain intensities of 4–7 and 3% showed high pain scores (8–10) on the VAS. The mean score value was 3, as in our patient cohort. Pain was significantly higher after SP/TP compared to PSP. In contrast to our study, there were more patients who also complained of more severe pain. Summarizing the data of our entire patient population and considering the most painful second postoperative day, the evaluation of the survey shows a median pain of 3 with a range between 2 and 4.75 (VAS). The advantage of ECD/PSP over SP/TP regarding postoperative pain could also not be confirmed in our study group. However, in the study of Koch et al. patients were examined purely retrospectively (surgery was performed between 1990 and 2002) and postoperative pain was not the primary endpoint examined[29].
There is a prospective study that investigated pain and other long-term complications after primary superficial parotidectomy for benign tumors in the long-term course (6, 12 and 24 months postoperatively). Wolber et al. demonstrated that pain, which still affected 53% of patients six months postoperatively, decreased significantly after 12 and 24 months. The main subjective problem of the 61 patients examined was sensation loss, followed by the appearance of the scar and fear of revision surgery[30].
In general, pain can be divided pathophysiologically into neuropathic and nociceptive pain. However, both types of pain often occur together and are referred to as “mixed pain”. It has been shown in some clinical pictures that mixed pain phenomena can already occur in the early phase of the disease[31].
Although injury to the facial or auricular nerves is one of the most common complications of parotid surgery[32,33,34] and can lead to neuropathic pain, our data collected immediately postoperatively did not reveal any increase in neuropathic pain with more invasive surgical techniques or, therefore, any difference between the groups.
There are some limitations to our study: initially, of course, not all outcome measures after parotidectomy were investigated. It is important to emphasize that several studies have shown an advantage of ECD regarding the occurrence of other complications during and after parotidectomy [1, 5, 28, 29, 32, 35,36,37].
Moreover, it should be noted that resection and ligation of the greater auricular nerve (GAN) during surgery were not considered in this study. A recent study has shown that damage to the GAN can lead to hypoesthesia and thus also to discomfort [38].
Random allocation of patients to the two study groups or blinding of the treatment was not practicable or feasible in our study, as the therapy had been strictly based on the previous findings and the clinical situation. Nevertheless, both patient groups were comparable in terms of demographic, clinical, and surgical data. Differences in the duration of surgery and the resectate size can be explained by the fundamentally different surgical techniques and were unavoidable.
Psychological factors that have a positive influence on postoperative pain, such as preoperative information about surgical techniques or postoperative pain treatment, are known to distort patient-reported outcome measures [39]. The fact that most patients received postoperative visits or help with filling out forms may also have positively influenced variables such as patient satisfaction with pain therapy. This was also confirmed in a study by Suffeda et al. for patients undergoing otolaryngology surgery. Here, a higher expected pain intensity, a higher depression score and higher anxiety were significantly associated with more pain in the univariate analysis [40]. In our study, patients were not screened for psychiatric comorbidities, which represents a possible bias.
Furthermore, it is possible that our study population was too small to detect slight but significant differences between the different surgical methods. Further studies with larger cohorts are needed to investigate this further.
Conclusion
In summary, it can be stated that the interventions examined in our patient population resulted in mild to moderate pain, a low actual symptom burden and a moderate need for patient care. We can exclude a neuropathic pain component as the main underlying pain quality after elective surgery on the parotid gland. In our study, we also found no superiority of the minimally invasive technique over superficial/total parotidectomy regarding postoperative pain perception immediately after surgery. These results should be confirmed in larger studies.
Data availability
The data is available upon request.
References
Marchese-Ragona R, De Filippis C, Marioni G, Staffieri A (2005) Treatment of complications of parotid gland surgery. Acta Otorhinolaryngol Ital 25(3): 174–8. http://www.ncbi.nlm.nih.gov/pubmed/16450773. Accessed 7 May 2017
Psychogios G, Vlastos I, Thölken R, Zenk J (2020) Warthin’s tumour seems to be the most common benign neoplasm of the parotid gland in Germany. Eur Arch Otorhinolaryngol 277(7):2081–2084. https://doi.org/10.1007/S00405-020-05894-Z
Mantsopoulos K, Iro H (2022) Extracapsular dissection versus conventional parotidectomy: comparing ‘apples with oranges’? Int J Oral Maxillofac Surg 51(4):576–577. https://doi.org/10.1016/J.IJOM.2021.08.005
Mantsopoulos K, Koch M, Iro H (2017) Extracapsular dissection as sole therapy for small low-grade malignant tumors of the parotid gland. Laryngoscope 127(8):1804–1807. https://doi.org/10.1002/lary.26482
Mantsopoulos K, Koch M, Klintworth N, Zenk J, Iro H (2015) Evolution and changing trends in surgery for benign Parotid tumors. Laryngoscope 125(1):122–127. https://doi.org/10.1002/lary.24837
Mashrah MA, Al-Sharani HM, Al-Aroomi MA, Abdelrehem A, Aldhohrah T, Wang L (2021) Surgical interventions for management of benign parotid tumors: systematic review and network meta-analysis. Head Neck 43(11):3631–3645. https://doi.org/10.1002/HED.26813
Laskaris S et al (2022) Partial superficial parotidectomy versus extracapsular anatomical dissection for the treatment of benign parotid tumors. Acta Med Acad 51(2):85–91. https://doi.org/10.5644/AMA2006-124.376
Martin H, Jayasinghe J, Lowe T (2020) Superficial parotidectomy versus extracapsular dissection: literature review and search for a gold standard technique. Int J Oral Maxillofac Surg 49(2):192–199. https://doi.org/10.1016/J.IJOM.2019.06.006
Schapher M, Koch M, Goncalves M, Mantsopoulos K, Iro H (2021) Extracapsular dissection in pleomorphic adenomas of the parotid gland: results after 13 years of follow-up. Laryngoscope 131(2):E445–E451. https://doi.org/10.1002/lary.28696
Apfelbaum JL, Chen C, Mehta SS, Gan TJ (2003) Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 97(2): 534–40, table of contents. http://www.ncbi.nlm.nih.gov/pubmed/12873949. Accessed 28 Nov 2016
Dolin SJ, Cashman JN, Bland JM (2002) Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth 89(3): 409–23. http://www.ncbi.nlm.nih.gov/pubmed/12402719. Accessed 28 Nov 2016
Kehlet H, Wilkinson RC, Fischer HBJ, Camu F and Prospect Working Group (2007) PROSPECT: evidence-based, procedure-specific postoperative pain management. Best Pract Res Clin Anaesthesiol 21(1): 149–59. http://www.ncbi.nlm.nih.gov/pubmed/17489225, Accessed 15 Apr 2017
Neugebauer E, Sauerland S, Keck V, Simanski C, Witte J (2003) Surgical pain management. A Germany-wide survey including the effect of clinical guidelines. Chirurg 74(3):235–238. https://doi.org/10.1007/s00104-003-0615-9
Pschowski R, Motsch J (2008) Die postoperative Schmerztherapie. Wien Med Wochenschr 158(21–22):603–609. https://doi.org/10.1007/s10354-008-0608-x
Rathmell JP et al (2006) Acute post-surgical pain management: a critical appraisal of current practice, December 2–4, 2005. Reg Anesth Pain Med 31(4 Suppl 1):1–42. https://doi.org/10.1016/j.rapm.2006.05.002
Gerbershagen HJ, Aduckathil S, van Wijck AJM, Peelen LM, Kalkman CJ, Meissner W (2013) Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 118(4):934–944. https://doi.org/10.1097/ALN.0b013e31828866b3
Laubenthal H, Neugebauer E (2009) S3-Leitlinie „Behandlung akuter perioperativer und posttraumatischer Schmerzen. AWMF-Leitlinien-Register 041(001): 74–88. http://www.awmf.org/uploads/tx_szleitlinien/001-025l_S3_Behandlung_akuter_perioperativer_und_posttraumatischer_Schmerzen_abgelaufen.pdf. Accessed 3 May 2017
Cuschieri S (2019) The STROBE guidelines. Saudi J Anaesth 13(Suppl 1):S31–S34. https://doi.org/10.4103/SJA.SJA_543_18
Meissner W, Ullrich K, Zwacka S (2006) Benchmarking as a tool of continuous quality improvement in postoperative pain management. Eur J Anaesthesiol 23(2):142–148. https://doi.org/10.1017/S026502150500205X
Poller K, Volk GF, Wittekindt C, Meissner W, Guntinas-Lichius O (2011) Estimation of postoperative pain after tonsillectomy in adults using QUIPS: an instrument to improve postoperative pain management. Laryngorhinootologie 90(2):82–89. https://doi.org/10.1055/s-0030-1269848
Freynhagen R, Baron R, Gockel U, Tölle TR (2006) pain DETECT : a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 22(10):1911–1920. https://doi.org/10.1185/030079906X132488
FR, TTR, GU, BR (2016) The painDETECT project-far more than a screening tool on neuropathic pain. Curr Med Res Opin 32(6): 1033–1057. https://doi.org/10.1185/03007995.2016.1157460.
Ben-Shachar M, Lüdecke D, Makowski D (2020) effectsize: estimation of effect size indices and standardized parameters. J Open Source Softw 5(56):2815. https://doi.org/10.21105/JOSS.02815
Mair P, Wilcox R (2020) Robust statistical methods in R using the WRS2 package. Behav Res Methods 52(2):464–488. https://doi.org/10.3758/S13428-019-01246-W
Eldridge SM et al (2010) CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. https://doi.org/10.1186/S40814-016-0105-8
Gerbershagen HJ, Rothaug J, Kalkman CJ, Meissner W (2011) Determination of moderate-to-severe postoperative pain on the numeric rating scale: a cut-off point analysis applying four different methods. Br J Anaesth 107(4):619–626. https://doi.org/10.1093/bja/aer195
Inhestern J et al (2015) Pain on the first postoperative day after head and neck cancer surgery. Eur Arch Otorhinolaryngol 272(11):3401–3409. https://doi.org/10.1007/S00405-014-3307-9
Foghsgaard S, Foghsgaard J, Homøe P (2007) Early post-operative morbidity after superficial parotidectomy: a prospective study concerning pain and resumption of normal activity. Clin Otolaryngol 32(1):54–57. https://doi.org/10.1111/j.1365-2273.2007.01315.x
Koch M, Zenk J, Iro H (2010) Long-term results of morbidity after parotid gland surgery in benign disease. Laryngoscope 120(4):724–730. https://doi.org/10.1002/lary.20822
Wolber P et al (2018) Patient’s perspective on long-term complications after superficial parotidectomy for benign lesions: Prospective analysis of a 2-year follow-up. Clin Otolaryngol 43(4):1073–1079. https://doi.org/10.1111/COA.13104
“Chronische Schmerzen: Das „mixed pain concept“ als neue Rationale.” https://www.aerzteblatt.de/archiv/41906/Chronische-Schmerzen-Das-mixed-pain-concept-als-neue-Rationale. Accessed 20 Aug 2024
Hancock BD (1999) Clinically benign parotid tumours: local dissection as an alternative to superficial parotidectomy in selected cases. Ann R Coll Surg Eng 81(5): 299–301. http://www.ncbi.nlm.nih.gov/pubmed/10645170. Accessed 31 May 2017
Rehberg E, Schroeder H-G, Kleinsasser O (1998) Chirurgie bei gutartigen Parotistumoren: Individuell angepaßte oder standardisierte radikale Eingriffe? Laryngorhinootologie 77(05):283–288. https://doi.org/10.1055/s-2007-996975
Witt RL (2002) The significance of the margin in parotid surgery for pleomorphic adenoma. Laryngoscope 112(12):2141–2154. https://doi.org/10.1097/00005537-200212000-00004
McGurk M, Renehan A, Gleave EN, Hancock BD (1996) Clinical significance of the tumour capsule in the treatment of parotid pleomorphic adenomas. Br J Surg 83(12): 1747–9. http://www.ncbi.nlm.nih.gov/pubmed/9038558. Accessed 30 May 2017
Prichard AJ, Barton RP, Narula AA (1992) Complications of superficial parotidectomy versus extracapsular lumpectomy in the treatment of benign parotid lesions. J R Coll Surg Edinb 37(3) 155–8. http://www.ncbi.nlm.nih.gov/pubmed/1328626. Accessed 31 May 2017
Klintworth N, Zenk J, Koch M, Iro H (2010) Postoperative complications after extracapsular dissection of benign parotid lesions with particular reference to facial nerve function. Laryngoscope 120(3):484–490. https://doi.org/10.1002/lary.20801
Plath M, Sand M, Cavaliere C, Plinkert PK, Baumann I, Zaoui K (2022) Long-term outcomes and quality of life following parotidectomy for benign disease. Acta Otorhinolaryngol Ital 42(3):215–222. https://doi.org/10.14639/0392-100X-N1728
Gritsenko K, Khelemsky Y, Kaye AD, Vadivelu N, Urman RD (2014) Multimodal therapy in perioperative analgesia. Best Pract Res Clin Anaesthesiol 28(1):59–79. https://doi.org/10.1016/j.bpa.2014.03.001
Suffeda A, Meissner W, Rosendahl J, Guntinas-Lichius O (2016) Influence of depression, catastrophizing, anxiety, and resilience on postoperative pain at the first day after otolaryngological surgery: a prospective single center cohort observational study. Medicine. https://doi.org/10.1097/MD.0000000000004256
Acknowledgements
The present work was performed in fulfillment of the requirements for obtaining the degree of „Dr. med. dent.”. Dr. Magdalene Ortmann, Dr. Bjarne Schmalbach, Ortmann–Statistik, https://ortmann-statistik.de/.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jansen, V., Gostian, AO., Allner, M. et al. Postoperative pain after parotid surgery—comparison between superficial/total parotidectomy and extracapsular dissection: a prospective observational study. Eur Arch Otorhinolaryngol (2024). https://doi.org/10.1007/s00405-024-08991-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00405-024-08991-5