Abstract
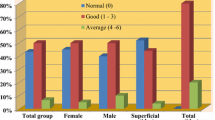
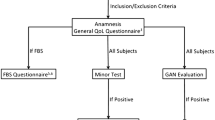
The present study investigated the long-term complications of parotidectomy, the differences in these complications in regard to the pathological diagnosis and type of surgery. The patients were questioned regarding the presence of facial paresis–paralysis, pain, loss of sensation, scarring, collapse, and mouth dryness in the area of operation. Complaints of pain (p = 0.287), scarring (p = 0.456), and mouth dryness (p = 0.136) did not show statistically significant differences between the cases with benign or malignant pathological outcomes. However, complaints of loss of sensation (p < 0.001), collapse in the area of operation (p = 0.025), paresis-paralysis (p < 0.001), and fear of repeated surgery (p = 0.032) were present at significantly higher rates. Complaints of pain (p = 0.258), scarring (p = 0.665), mouth dryness (p = 0.113) and fear of repeated surgery (p = 0.053) did not show statistically significant differences between the cases who underwent superficial or total parotidectomy. However, complaints of loss of sensation (p = 0.002), paresis (p < 0.001), and collapse in the area of operation (p = 0.019) were present at significantly higher rates. The type of tumor and surgical approach significantly affect the quality of life; however, parotidectomy generally does not lead to serious long-term complications that would disturb the patients.
Similar content being viewed by others
References
Leverstein H, van der Wal JE, Tiwari RM, van der Waal I, Snow GB (1997) Surgical management of 246 previously untreated pleomorphic adenomas of the parotid gland. Br J Surg 84:399–403
Bron LP, O’Brien CJ (1997) Facial nerve function after parotidectomy. Arch Otolaryngol Head Neck Surg 123:1091–1096
Dell’aversana Orabona G, Salzano G, Petrocelli M, Iaconetta G, Califano L (2014) Reconstructive techniques of the parotid region. J Craniofac Surg 5(3):998–1002
Arad- Cohen A, Blitzer A (2000) Botulinum toxin treatment for symptomatic Frey’s syndrome. Otollaryngol Head Neck Surg 122(2):237–240
Ciuman RR, Oels W, Jaussi R, Dost P (2012) Outcome, general, and symptom-specific quality of life after various types of parotid resection. Laryngoscope 122(6):1254–1261
Yla-Kotola T, Goldstein DP, Hofer SO, Patel SN, Brown DH, Irish JC, Gullane PJ, Gilbert R (2015) Facial nerve reconstruction and facial disfigurement after radical parotidectomy. J Reconstr Microsurg 31(4):313–318
Chaushu G, Dori S, Sela BA, Taicher S, Kronenberg J, Talmi YP (2001) Salivary flow dynamics after parotid surgery: a preliminary report. Otollaryngol Head Neck Surg 124(3):270–273
Smith SL, Komisar A (2007) Limited parotidectomy: the role ofextracapsular dissection in parotid gland neoplasms. Laryngoscope 117:1163–1167
Cummins CW, Flint PW, Harker LA (2007) Malignant tumors of the salivary glands. In: Koç C (ed) Cummings otolaryngology head and neck surgery, 2nd edn. Oncu Basimevi, Istanbul, pp 1400–1401
Nitzan D, Kronenberg J, Horowitz Z, Wolf M, Bedrin L, Chaushu G, Talmi YP (2004) Quality of life following parotidectomy for malignant and benign disease. Plast Reconstr Surg 114(5):1060–1067
Gaillard C, Périé S, Susini B, Guily S, Lacau J (2005) Facial nerve dysfunction after parotidectomy: the role of local factors. Laryngoscope 115:287–291
Mehle ME, Kraus DH, Wood BG et al (1993) Facial nerve morbidity following parotid surgery for benign disease: the Cleveland Clinic Foundation experience. Laryngoscope 103:386–388
Brennan J, Moore EJ, Shuler KJ (2001) Prospective analysis of the efficacy of continuous intraoperative nerve monitoring during thyroidectomy, parathyroidectomy, and parotidectomy. Otolaryngol Head Neck Surg 124:537–543
Spiro RH, Huvos AG, Strong EW (1982) Adenocarcinoma of salivary origin: clinicopathologic study of 204 patients. Am J Surg 44:423–431
De Oliveira FA, Duarte EC, Taveira CT, Máximo AA, de Aquino EC, Alencar Rde C et al (2009) Salivary gland tumor: a review of 599 cases in a Brazilian population. Head Neck Pathol 3:271–275
Patel N, Har-El G, Rosenfeld R (2001) Quality of life after great auricular nerve sacrifice during parotidectomy. Arch Otolaryngol Head Neck Surg 127:884–888
Chan LS, Barakate MS, Havas TE (2014) Free fat grafting in superficial parotid surgery to prevent Frey’s syndrome and improve aesthetic outcome. J Laryngol Otol 128(Suppl 1):S44–S49
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
In the article, there is no conflict of interest.
All patients are allowed to participate in the study and informed consent was obtained verbally.
Financial disclosure
We did not receive financial support for this article.
Rights and permissions
About this article
Cite this article
Kaya, B.V., Kılıç, C., Özlügedik, S. et al. Long-term effects of parotidectomy. Eur Arch Otorhinolaryngol 273, 4579–4583 (2016). https://doi.org/10.1007/s00405-016-4173-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4173-4