Abstract
Objective
To evaluate obstetric and perinatal outcomes among small for gestational age (SGA) infants born to patients diagnosed with Gestational diabetes mellitus (GDM).
Materials and methods
A multicenter retrospective cohort study between 2005 and 2021. The perinatal outcomes of SGA infants born to patients with singleton pregnancy and GDM were compared to SGA infants born to patients without GDM. The primary outcome was a composite adverse neonatal outcome. Infants with known structural/genetic abnormalities or infections were excluded. A univariate analysis was conducted followed by a multivariate analysis (adjusted odds ratio [95% confidence interval]).
Results
During the study period, 11,662 patients with SGA infants met the inclusion and exclusion criteria. Of these, 417 (3.6%) SGA infants were born to patients with GDM, while 11,245 (96.4%) were born to patients without GDM. Overall, the composite adverse neonatal outcome was worse in the GDM group (53.7% vs 17.4%, p < 0.01). Specifically, adverse neonatal outcomes such as a 5 min Apgar score < 7, meconium aspiration, seizures, and hypoglycemia were independently associated with GDM among SGA infants. In addition, patients with GDM and SGA infants had higher rates of overall and spontaneous preterm birth, unplanned cesarean, and postpartum hemorrhage. In a multivariate logistic regression assessing the association between GDM and neonatal outcomes, GDM was found to be independently associated with the composite adverse neonatal outcome (aOR 4.26 [3.43–5.3]), 5 min Apgar score < 7 (aOR 2 [1.16–3.47]), meconium aspiration (aOR 4.62 [1.76–12.13]), seizures (aOR 2.85 [1.51–5.37]) and hypoglycemia (aOR 16.16 [12.79–20.41]).
Conclusions
Our study demonstrates that GDM is an independent risk factor for adverse neonatal outcomes among SGA infants. This finding underscores the imperative for tailored monitoring and management strategies in those pregnancies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM), defined as glucose intolerance first identified during pregnancy [1], affects 14% of pregnancies and is rapidly escalating in prevalence globally [2]. Typically, the hyperglycemic state associated with GDM results in fetal hyperinsulinemia, leading to the development of large for gestational age (LGA) infants with specific associated morbidity [3, 4]. Surprisingly, up to 7% of infants born to patients with GDM exhibit the opposite outcome—being small for gestational age (SGA) [3]. SGA infants, defined as those with a birth weight below the 10th percentile for their gestational age [5] often face a heightened risk of adverse perinatal outcomes [6]. Notably, infants born to patients with GDM or infants that are SGA share similar risks for long-term complications such as obesity, type 2 diabetes, hypertension, and ischemic heart disease, hinting at a potential shared biological pathway between these two conditions [7,8,9].
Despite these insights, the existing literature on the intersection between GDM and SGA infants remains sparse [8, 10].
This study aims to explore the obstetric and perinatal outcomes of SGA infants born to patients with GDM compared to those without.
Materials and methods
A multicenter retrospective cohort study was conducted from 2005 to 2021, utilizing computerized medical records from two university-affiliated medical centers in Jerusalem, Israel: shaare zedek medical center (SZMC) and bikur holim medical center (BHMC). These medical centers collectively account for approximately 16% of all deliveries in Israel, with an average annual volume of 20,000 deliveries.
For the study’s purpose, patients with singleton pregnancies diagnosed with SGA infants were enrolled. Exclusion criteria encompassed patients with unknown glycemic status due to a lack of diagnostic tests, pre-pregnancy diabetes mellitus, multifetal gestation, pre-viable deliveries before 24 + 0 weeks, pre-delivery fetal death, and with known major malformations, genetic disorders, or infection.
GDM was defined either by an appropriate diagnosis in the patient’s medical record or an abnormal result in glucose tolerance test using the “two-step” method; In Israel, all pregnant women receive antenatal care coverage under the National Health Plan and are routinely screened for GDM via a 50 g oral GCT between 24 and 28 gestational weeks. Women with a plasma glucose concentration of ≥ 140 mg/dL at the GCT or with other risk factors for GDM and a result of ≥ 130 mg/dL are referred to OGTT. A diagnosis of GDM is made if the woman meets specific criteria, which include fasting 3 h 100 g OGTT values (two or more of the following values: fasting ≥ 95 mg/dL, 1 h ≥ 180 mg/dL, 2 h ≥ 155 mg/dL, and/or 3 h ≥ 140 mg/dL [11]) or GCT test result ≥ 200 mg/dL [12].
SGA was defined by a birth weight below the 10th percentile for gestational age and gender based on the birth weight curves of the Israeli population [13].
Both medical centers follow similar departmental protocols regarding the antepartum and intrapartum management of SGA and GDM that align with the criteria defined in the guidelines of the Israeli Committee of Obstetrics and Gynecology [14, 15].
Demographic and obstetric characteristics of patients with small-for-gestational age infant with and without Gestational diabetes were evaluated including age, parity, pregnancy HTN disorders, hypertensive disorders of pregnancy and obesity.
‘Pregnancy HTN disorders’ was defined as all hypertensive disorders occurring in pregnant patients, including those with pre-existing chronic hypertension. ‘Hypertensive disorders of pregnancy’ refer specifically to pregnancy-induced hypertension disorders, such as gestational hypertension, preeclampsia, and HELLP syndrome, which manifest during pregnancy and are not present before gestation.
The primary outcome was defined as adverse neonatal outcome including at least one of the following: perinatal mortality, neonatal intensive care unit (NICU) admission, Apgar score less than 7 at 5 min, meconium aspiration, hypoglycemia, neonatal jaundice, convulsions, shoulder dystocia or clavicular fracture, need for mechanical ventilation, respiratory distress syndrome or transient tachypnea of the newborn (TTN), necrotizing enterocolitis, intracranial hemorrhage, or neonatal sepsis [10]. Hypoglycemia is defined in our institution as blood sugar levels below 50 mg/dL before feeding. Monitoring of blood sugar levels in neonates at high risk for hypoglycemia is conducted in accordance with the guidelines of the American Academy of Pediatrics [16]. Regular Monitoring for neonates born to diabetic mothers is conducted for 24 h postpartum while monitoring for small-for-gestational-age neonates is conducted for 12 h.
The secondary outcomes included the individual components of the composite outcome and the following obstetric and maternal outcomes; Gestational age at delivery, Preterm birth (PTB, < 37 + 0 weeks of gestation), postpartum hemorrhage (PPH, Estimated blood loss of over 1000 mL and/or hemoglobin drop > 3 gr/dL and/or transfusion of blood products), placental abruption, maternal intensive care unit (ICU) admission and cesarean delivery (CD) rate.
Both SZMC and BHMC maintain electronic medical record databases. Delivery data are updated in real-time by attending healthcare professionals and audited periodically by trained technical personnel to ensure data validity and eliminate information bias. For this study, we extracted relevant maternal and neonatal records from this database, and personal information for each patient was pseudonymized before analysis, with all identifiable data replaced by unique codes.
The study group consisted of patients with GDM and SGA infants and they were compared to those with SGA infants without GDM (control group).
The study was approved by the SZMC’s institutional ethics committee (IRB: 0253-23-SZMC) that oversees both medical center research activities, adhering to the declaration of Helsinki, and given its retrospective and unidentified nature, informed consent was waived.
Statistical methods
Nominal variables were described using proportions and compared using the appropriate statistical tests, such as the chi-square test or Fisher’s exact test. Continuous variables, which did not follow a normal distribution, were presented as means ± standard deviation (SD) or medians with interquartile ranges (IQR). These continuous variables were analyzed using the unpaired student’s t-test or Mann–Whitney test, depending on the distribution. A p-value of less than 0.05 was considered statistically significant.
The association between GDM and neonatal outcomes was adjusted to maternal age, gravidity, parity, number of previous CDs, fertility Treatments, hypertensive disorders of pregnancy, and gestational age at delivery using a multivariate logistic regression model. Adjusted odds ratios (aOR) with 95% confidence intervals (CIs) were reported to measure the strength of the association. All statistical tests were two-sided. The statistical analyses were performed using SPSS software (version 25, IBM, Armonk, NY).
Results
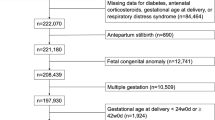
During the study period, there were 292,126 deliveries in our hospitals. Of these, 19,220 (6.6%) involved SGA infants. After applying our inclusion criteria, 11,662 cases were included, with 417 (3.6%) diagnosed with GDM and 11,245 (96.4%) born to patients without GDM (Fig. 1).
In Table 1, we provide an overview of the general demographics and obstetric characteristics of the study population. Patients with GDM were of advanced maternal age, with higher parity and higher rates of obesity, smoking, hypertensive disorders (both chronic and pregnancy-induced), fertility treatment, and previous CDs.
Table 2 presents the neonatal characteristics of both groups.
Primary outcome
The GDM group exhibited worse rates of composite adverse neonatal outcomes (53.7% vs. 17.4%, p < 0.01).
Secondary outcomes
SGA infants born to patients with GDM had lower birth weights (2447.6 vs. 2564.4, p < 0.01) without a difference in weight percentile groups. The GDM group had a significantly higher rate of NICU admission (15.1% vs. 8.3%, p < 0.01), lower 5 min Apgar scores < 7 (3.9% vs. 1.5%, p < 0.01), a higher rate of meconium aspiration (1.4% vs. 0.2%, p < 0.01), and higher rates of TTN, mechanical ventilation, seizures, and hypoglycemia (4.1% vs. 1.8%, 4.1% vs. 1.4%, 2.9% vs. 1%, and 42.4% vs. 3.6%, respectively, p < 0.01). However, other neonatal characteristics, including birth trauma, sepsis, and jaundice, did not differ between the groups.
Table 3 displays the delivery and obstetric outcomes. The GDM group had a higher rate of delivery induction (32.5% vs. 20.4%, p < 0.01), earlier gestational age at delivery (38.5 vs. 39.2 weeks, p < 0.01), a higher rate of PTB < 37 weeks (4.5% vs. 7.9%, p < 0.01), and spontaneous PTB (3.6% vs. 1.7%, p < 0.01). The GDM group showed a significantly higher rate of PPH (11.8% vs. 8.6%, p < 0.03), with no difference in blood product transfusion. Both planned and unplanned cesarean rates were significantly higher in the GDM group (15.8% vs. 8.9% and 19.9% vs. 7.3%, respectively, p < 0.01). Rates of maternal ICU admission and placental abruption did not differ between groups.
Table 4 presents the results of a multivariate logistic regression assessing the association between GDM and neonatal outcomes, after controlling for significant covariates. GDM was independently associated with the composite adverse neonatal outcome (aOR 4.26, 95%CI 3.43–5.3) as well as with 5 min Apgar score < 7 (aOR 2, 95%CI 1.16–3.47), meconium aspiration (aOR 4.62, 95%CI 1.76–12.13), seizures (aOR 2.85, 95%CI 1.51–5.37), and hypoglycemia (aOR 16.16, 95%CI 12.79–20.41). NICU admission, mechanical ventilation, and TTN were no longer significantly increased after adjustment.
Discussion
In this retrospective cohort study, we aimed to evaluate the outcomes of SGA infants born to patients with GDM. Our data revealed that the composite neonatal morbidity was significantly more prevalent among SGA infants born to patients with GDM compared to SGA infants born to patients with no GDM. Specifically, adverse neonatal outcomes such as hypoglycemia, seizures, 5 min Apgar score < 7, and meconium aspiration, were independently associated with GDM among SGA infants. In addition, patients with GDM and SGA infants had higher rates of PTB, PPH, and unplanned CD.
Hypoglycemia is a common metabolic disturbance within the initial hours of an infant's life due to the abrupt cessation of glucose infusion from the placenta, causing a decline in the infant’s blood glucose concentration [17]. For most healthy infants, this transitional phase of neonatal hypoglycemia is brief, transient, and asymptomatic.
However, SGA infants born to patients with GDM face a higher risk of experiencing more severe or prolonged hypoglycemia [18]. This heightened risk is attributed to factors such as insufficient glycogen or fat tissue reserves and increased glucose utilization due to excessive insulin production due to the intra-uterine diabetic environment [19, 20]. Consequently, when blood sugar levels drop too low, the brain doesn’t receive adequate glucose, potentially leading to various neurological symptoms, including a higher rate of seizures observed in these infants [21]. Additionally, The elevated rates of 5 min Apgar score < 7 and meconium aspiration may be associated with the effects of GDM on endothelial dysfunction and the exacerbation of chronic fetal hypoxia [7, 22].
Previous research has primarily focused on outcomes of SGA newborns born to patients with GDM, often comparing them with appropriate for gestational age (AGA) or LGA newborns born to patients with GDM. Garcia-Patterson et al. [3] noted that SGA newborns had significantly higher rates of low 1 min Apgar scores and hypoglycemia compared to their LGA and AGA counterparts, mirroring our observations of increased vulnerability in SGA newborns to such complications. Similarly, Esakoff’s study [23] highlighted an increased risk of respiratory distress syndrome (RDS), intrauterine fetal demise (IUFD), neonatal demise, hypoglycemia, and jaundice in term SGA newborns compared to AGA newborns born to patients with GDM. Furthermore, Barquiel et al. [24] reported an additive effect of SGA status on the occurrence of neonatal complications like hypoglycemia, hyperbilirubinemia, polycythemia, and perinatal death, alongside a higher prevalence of maternal hypertension and preeclampsia in the SGA group in compare to AGA and LGA groups. In a retrospective cohort study conducted by Wang et al. [25] aimed to discern the characteristics of stillbirths within the context of diabetic pregnancies, IUGR was identified in 16% of 37 diabetic patients who encountered stillbirth. Specifically, within the subset of patients diagnosed with GDM and stillbirth, IUGR was identified in 26% of cases, emerging as a prominent characteristic associated with stillbirth in this particular population. Our findings align with the study of Chen et al. [10] which compared SGA newborns born to patients with GDM to those born to patients without GDM and found an increased risk for adverse outcomes, including low Apgar scores, early thrombocytopenia, hypoxic-ischemic encephalopathy, hypoglycemia, and pulmonary hemorrhage among the GDM group. However, this study by Chen et al. included only term infants, thereby excluding severe cases of growth restrictions. In addition, this study included infants with diverse malformations. In contrast, our study intentionally omitted such cases to present a more comprehensive overview of the associated morbidity in this population. In terms of CD rates, our study identified that SGA newborns born to patients with GDM were more likely to be delivered via cesarean, both elective and emergency, diverging from Chen et al. [10], who reported a lower rate of CD among GDM-associated SGA deliveries. This variance may reflect different clinical management approaches or different background clinical characteristics between the studies as a higher prevalence of previous CD was specifically observed in our study population, suggesting a distinct clinical profile that may further predispose these patients to surgical delivery. Notably, our findings of a higher rate of unplanned CD in SGA newborns, particularly those born to patients with GDM, can be attributed to increased fetal distress in this subgroup, and align with previous comprehensive studies and systematic reviews [20, 26].
In addition to the short-term pregnancy outcomes discussed above, numerous studies have demonstrated that SGA and GDM separately pose long-term risks for adverse outcomes in infants [7, 9, 27]. A study by Neimark et al. demonstrated that SGA infants born to patients with GDM exhibited a higher incidence of cardiovascular hospitalizations during childhood compared to SGA children born to patients without GDM [28].
Several studies have sought to characterize the risk factors linked to SGA infants in patients being treated for GDM. Within this specific cohort of patients, elevated incidences of hypertensive disorders, lower body mass index (BMI), inadequate maternal weight gain during pregnancy [29, 30], higher levels of glycemic control [31], and a higher frequency of infants deemed high risk for SGA among patients with GDM [32]. This reinforces our assertion that this subgroup presents unique risk factors and associated complications, which necessitate consideration during pregnancy, delivery, and post-natal care. It is noteworthy that our study exhibited significantly reduced rates of SGA neonates compared to those commonly reported in literature [5]. The lower rates of SGA in our study may be attributed to the unique demographic characteristics of our population, including a high percentage of high-order deliveries. Previous studies in our population have shown that higher parity can influence birth weight and reduce the SGA rate [33,34,35].
Several hypotheses have been posited to elucidate the pathophysiology of GDM and its association with fetal growth restriction [22, 37]. GDM is known to induce endothelial dysfunction, promoting the secretion of vasoactive substances and oxidative stress, which can lead to vascular insufficiencies such as thrombosis, hypertension, and atherosclerosis [22, 38,39,40,41]. The placental microangiopathy, impairs the placenta's capacity to provide sufficient nutrients and oxygen to the fetus, alterations in lipid metabolism, essential amino acids, and elevated inflammatory markers. All these mechanisms ultimately contribute to fetal growth restriction. Moreover, the hyperglycemic intrauterine environment associated with GDM may adversely affect fetal development, potentially increasing long-term cardiovascular risks for the offspring [9, 27].
In our study, we demonstrated that patients with GDM and SGA newborns were more likely to exhibit higher rates of obesity and hypertensive disorders, including chronic hypertension. These conditions, along with GDM, might exacerbate placental dysfunction, leading to impaired fetal growth. The prevalence of obesity and hypertension in these patients suggests an underlying metabolic syndrome, representing an ongoing assault on the maternal vascular system. This connection provides a clinical basis to suggest that these patients are at a higher risk of developing type 2 diabetes in the future, as their inability to manage the “stress test” of pregnancy indicates an increased vulnerability to metabolic disorders [42].
To further support our findings and hypotheses, future research could incorporate Doppler studies to assess placental pathology, offering direct evidence of the vascular abnormalities associated with GDM and SGA outcomes. Investigating maternal blood markers such as placental growth factor (PlGF), soluble fms-like tyrosine kinase-1 (sFlt-1), and inflammatory cytokines could further elucidate the mechanisms at play [22]. These biomarkers might shed light on the impact of GDM on placental function and its contribution to the development of SGA, thereby providing potential avenues for therapeutic intervention and improving maternal–fetal health outcomes.
Strength and limitation
The strengths of our study include its multicenter design and the utilization of electronic medical records with real-time validation, minimizing retrospective study biases. Additionally, the comprehensive uniform coverage of all expenses related to antenatal, delivery, and postnatal care by the national health insurance enhances the reliability of our findings.
However, the study is not devoid of limitations. Its retrospective design inherently carries limitations, including potential biases not accounted for in the study design. The specific demographic characteristics of the population, especially the preference for larger family sizes, may limit the generalizability of the findings to other populations. The omission of Doppler studies of SGA infants and their correlation to placental pathology leaves unanswered questions about the underlying vascular pathophysiology, highlighting the need for further investigation in this area.
Additionally, the absence of long-term outcome data on SGA infants born to patients with GDM, such as catch-up growth and cardiovascular disease incidence, indicates a gap that necessitates further research.
Conclusions
In conclusion, our multicenter retrospective cohort study sheds light on the association between GDM and adverse outcomes in SGA infants. The increased rates of adverse neonatal outcomes underscore the need for heightened clinical attention and management in pregnancies complicated by both GDM and SGA, advocating for personalized and proactive care strategies to safeguard their health and development. Further research should delve into placental pathology using Doppler studies and explore maternal blood markers to elucidate the mechanisms linking GDM to SGA outcomes.
Data availability
Not applicable.
References
Care D, Suppl SS (2022) Classification and diagnosis of diabetes : standards of medical care in diabetes — 2022. Diabetes Care 45:17–38
Wang H, Li N, Chivese T, Werfalli M, Sun H, Yuen L et al (2022) IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by international association of diabetes in pregnancy study group’s criteria. Diabetes Res Clin Pract. https://doi.org/10.1016/j.diabres.2021.109050
Garcia-Patterson A, Corcoy R, Balsells M, Altirriba O, Adelantado JM, Cabero L et al (1998) In pregnancies with gestational diabetes mellitus and intensive therapy, perinatal outcome is worse in small-for-gestational-age newborns. Am J Obstet Gynecol 179:481–485. https://doi.org/10.1016/S0002-9378(98)70383-7
Landon MB, Mele L, Spong CY, Carpenter MW, Ramin SM, Casey B et al (2011) The relationship between maternal glycemia and perinatal outcome. Obstet Gynecol 117:218–224. https://doi.org/10.1097/AOG.0b013e318203ebe0
Lees CC, Stampalija T, Baschat A, da Silva CF, Ferrazzi E, Figueras F et al (2020) ISUOG practice guidelines: diagnosis and management of small-for-gestational-age fetus and fetal growth restriction. Ultrasound Obstet Gynecol 56:298–312. https://doi.org/10.1002/uog.22134
Sharma D, Shastri S, Farahbakhsh N, Sharma P (2016) Intrauterine growth restriction–part 1. J Matern Neonatal Med 29:3977–3987. https://doi.org/10.3109/14767058.2016.1152249
Sharma D, Farahbakhsh N, Shastri S, Sharma P (2016) Intrauterine growth restriction–part 2. J Matern Neonatal Med 29:4037–4048. https://doi.org/10.3109/14767058.2016.1154525
García-Patterson A, Balsells M, Solà I, Gich I, Corcoy R (2023) Impact of gestational diabetes mellitus treatment on medium/long-term outcomes after pregnancy: a systematic review and meta-analysis. Diabet Med 40:1–11. https://doi.org/10.1111/dme.14998
Kawasaki M, Arata N, Ogawa Y (2018) Obesity and abnormal glucose tolerance in the offspring of mothers with diabetes. Curr Opin Obstet Gynecol 30:361–368. https://doi.org/10.1097/GCO.0000000000000479
Chen J, Xiao H, Yang Y, Tang Y, Yang X, Zhang Z et al (2021) Demographic and clinical features of small-for-gestational-age infants born to mothers with gestational diabetes mellitus. Front Pediatr 9:1–9. https://doi.org/10.3389/fped.2021.741793
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 144:768–773
Temming LA, Tuuli MG, Stout MJ, Macones GA, Cahill AG (2016) Diagnostic ability of elevated 1-h glucose challenge test. J Perinatol 36:342–346. https://doi.org/10.1038/jp.2015.215
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon ES (2005) Birthweight standards in the live-born population in Israel. Isr Med Assoc J 7:311–314
Paper P (2023) Gestational diabetes mellitus-The Israeli Association of Obstetrics and Gynecology, paper position no.16
Paper P (2023) IUGR-The Israeli Association of Obstetrics and Gynecology, paper position no.10
Adamkin DH, Papile LA, Baley JE, Bhutani VK, Carlo WA, Kumar P et al (2011) Clinical report - postnatal glucose homeostasis in late-preterm and term infants. Pediatrics 127:575–579. https://doi.org/10.1542/peds.2010-3851
Abramowski A, Ward R, Hamdan AH (2023) Neonatal Hypoglycemia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan–2023 Sep 4. PMID: 30725790
Harris DL, Weston PJ, Harding JE (2012) Incidence of neonatal hypoglycemia in babies identified as at risk. J Pediatr 161:787–791. https://doi.org/10.1016/j.jpeds.2012.05.022
Puchalski ML, Russell TL, Karlsen KA (2018) Neonatal hypoglycemia: is there a sweet spot? Crit Care Nurs Clin North Am 30:467–480. https://doi.org/10.1016/j.cnc.2018.07.004
Ye W, Luo C, Huang J, Li C, Liu Z, Liu F (2022) Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. https://doi.org/10.1136/bmj-2021-067946
Rozance PJ, Hay WW (2006) Hypoglycemia in newborn infants: features associated with adverse outcomes. Biol Neonate 90:74–86. https://doi.org/10.1159/000091948
Joo EH, Kim YR, Kim N, Jung JE, Han SH, Cho HY (2021) Effect of endogenic and exogenic oxidative stress triggers on adverse pregnancy outcomes: preeclampsia, fetal growth restriction, gestational diabetes mellitus and preterm birth. Int J Mol Sci. https://doi.org/10.3390/ijms221810122
Esakoff TF, Guillet A, Caughey AB (2017) Does small for gestational age worsen outcomes in gestational diabetics?*. J Matern Neonatal Med 30:890–893. https://doi.org/10.1080/14767058.2016.1193142
Barquiel B, Herranz L, Martínez-Sánchez N, Montes C, Hillman N, Bartha JL (2020) Increased risk of neonatal complications or death among neonates born small for gestational age to mothers with gestational diabetes. Diabetes Res Clin Pract. https://doi.org/10.1016/j.diabres.2019.107971
Wang M, Athayde N, Padmanabhan S, Cheung NW (2019) Causes of stillbirths in diabetic and gestational diabetes pregnancies at a NSW tertiary referral hospital. Aust New Zeal J Obstet Gynaecol 59:561–566. https://doi.org/10.1111/ajo.12936
Ovesen PG, Jensen DM, Damm P, Rasmussen S, Kesmodel US (2015) Maternal and neonatal outcomes in pregnancies complicated by gestational diabetes. a nation-wide study. J Matern Neonatal Med. 28:1720–1724. https://doi.org/10.3109/14767058.2014.966677
Abokaf H, Shoham-Vardi I, Sergienko R, Landau D, Sheiner E (2018) In utero exposure to gestational diabetes mellitus and long term endocrine morbidity of the offspring. Diabetes Res Clin Pract 144:231–235. https://doi.org/10.1016/j.diabres.2018.09.003
Neimark E, Wainstock T, Sheiner E, Fischer L, Pariente G (2019) Long-term cardiovascular hospitalizations of small for gestational age (SGA) offspring born to women with and without gestational diabetes mellitus (GDM)‡. Gynecol Endocrinol 35:518–524. https://doi.org/10.1080/09513590.2018.1541233
Koren R, Idan C, Elkan M, Koren S, Wiener Y (2022) The risk of small and large for gestational age newborns in women with gestational diabetes according to pre-gestational body mass index and weight gain. J Matern Neonatal Med 35:8382–8387. https://doi.org/10.1080/14767058.2021.1974390
Xiao Y, Zhang X (2020) Association between maternal glucose / lipid metabolism parameters and abnormal newborn birth weight in gestational diabetes complicated by preeclampsia : a retrospective analysis of 248 cases. Diabetes Ther 11:905–914. https://doi.org/10.1007/s13300-020-00792-3
Li J, Pan Y, Zheng Q, Chen X, Jiang X, Liu R et al (2024) Risk factors and glycaemic control in small-for-gestational-age infants born to mothers with gestational diabetes mellitus: a case-control study using propensity score matching based on a large population. BMJ Open 14:e078325. https://doi.org/10.1136/bmjopen-2023-078325
Drever HJ, Davidson SJ, Callaway LK, Sekar R, De Jersey SJ (2023) Factors associated with higher risk of small-for-gestational-age infants in women treated for gestational diabetes. Aust New Zeal J Obstet Gynaecol 63:714–720. https://doi.org/10.1111/ajo.13696
Babinszki A, Kerenyi T, Torok O, Grazi V, Lapinski RH, Berkowitz RL (1999) Perinatal outcome in grand and great-grand multiparity: effects of parity on obstetric risk factors. Am J Obstet Gynecol 181:669–674. https://doi.org/10.1016/s0002-9378(99)70511-9
Samueloff A, Mor-Yosef S, Seidman DS, Rabinowitz R, Simon A, Schenker JG (1989) Grand multiparity–a nationwide survey. Isr J Med Sci 25:625–629
Kofman R, Farkash R, Rottenstreich M, Samueloff A, Wasserteil N, Kasirer Y et al (2022) Parity-adjusted term neonatal growth chart modifies neonatal morbidity and mortality risk stratification. J Clin Med. https://doi.org/10.3390/jcm11113097
Morgan AR, Thompson JMD, Murphy R, Black PN, Lam WJ, Ferguson LR et al (2010) Obesity and diabetes genes are associated with being born small for gestational age: results from the auckland birthweight collaborative study. BMC Med Genet. https://doi.org/10.1186/1471-2350-11-125
Shi Y, Vanhoutte PM (2017) Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes 9:434–449. https://doi.org/10.1111/1753-0407.12521
Kaur R, Kaur M, Singh J (2018) Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: Molecular insights and therapeutic strategies. Cardiovasc Diabetol 17:1–17. https://doi.org/10.1186/s12933-018-0763-3
Hattersley AT, Tooke JE (1999) The fetal insulin hypothesis: an alternative explanation of the association of low birthweight with diabetes and vascular disease. Lancet 353:1789–1792. https://doi.org/10.1016/S0140-6736(98)07546-1
Lan Q, Zhou Y, Zhang J, Qi L, Dong Y, Zhou H et al (2022) Vascular endothelial dysfunction in gestational diabetes mellitus. Steroids 184:108993. https://doi.org/10.1016/j.steroids.2022.108993
Buchanan TA, Xiang AH, Buchanan TA, Xiang AH (2005) Gestational diabetes mellitus. J Clin Investig 115:485–491. https://doi.org/10.1172/JCI200524531.The
Funding
Open access funding provided by Hebrew University of Jerusalem. This study was not funded.
Author information
Authors and Affiliations
Contributions
AH conducted the study and wrote the manuscript, TP conducted the study and wrote the manuscript, HYS designed, planned, and conducted the study and wrote the manuscript, SS designed, planned, and wrote the manuscript, SGG analyzed the data and edited the manuscript, and MR designed, planned, conducted the study, analyzed the data and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have nothing to disclose and that they have no financial or non-financial conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hirsch, A., Peled, T., Schlesinger, S. et al. Impact of gestational diabetes mellitus on neonatal outcomes in small for gestational age infants: a multicenter retrospective study. Arch Gynecol Obstet 310, 685–693 (2024). https://doi.org/10.1007/s00404-024-07587-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07587-y