Abstract
Purpose
To evaluate the relationship between maternal left ventricular systolic function, utero-placental circulation, and risk of adverse neonatal outcomes in women with cardiac disease.
Methods
119 women managed in the pregnancy heart clinic (2019–2021) were identified. Women were classified by their primary cardiac condition. Adverse neonatal outcomes were: low birth weight (< 2500 g), small-for-gestational-age (< 10th birth-weight centile), pre-term delivery (< 37 weeks’ gestation), and fetal demise (> 20 weeks’ gestation). Parameters of left ventricular systolic function (global longitudinal strain, radial strain, ejection fraction, average S’, and cardiac output) were calculated and pulsatility index was recorded from last growth scan.
Results
Adverse neonatal outcomes occurred in 28 neonates (24%); most frequently in valvular heart disease (n = 8) and cardiomyopathy (n = 7). Small-for-gestational-age neonates were most common in women with cardiomyopathy (p = 0.016). Early pregnancy average S’ (p = 0.03), late pregnancy average S’ (p = 0.02), and late pregnancy cardiac output (p = 0.008) were significantly lower in women with adverse neonatal outcomes than in those with healthy neonates. There was a significant association between neonatal birth-weight centile and global longitudinal strain (p = 0.04) and cardiac output (p = 0.0002) in late pregnancy. Pulsatility index was highest in women with cardiomyopathy (p = 0.007), and correlated with average S’ (p < 0.0001) and global longitudinal strain (p = 0.03) in late pregnancy.
Conclusion
Women with cardiac disease may not tolerate cardiovascular adaptations required during pregnancy to support fetal growth. Adverse neonatal outcomes were associated with reduced left ventricular systolic function and higher pulsatility index. The association between impaired systolic function and reduced fetal growth is supported by insufficient utero-placental circulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meeting the physiological demands of pregnancy requires considerable adaptation of the maternal cardiovascular system [1]. The maternal vasculature must accommodate a significant increase in blood volume, increasing both preload and stroke volume [1, 2], and a concomitant drop in total peripheral resistance. Maternal cardiac output increases by up to 50% during pregnancy [3,4,5], with the consequent altered loading of the left ventricle resulting in reversible cardiac remodelling [6]. It has been estimated that left ventricular end-diastolic diameter increases by 7–12% and left ventricular mass increases by up to 50% in healthy pregnancy [1, 3, 4, 6,7,8]. These cardiovascular adaptations are primarily hormonally mediated and are necessary to ensure sufficient utero-placental circulation for fetal growth and development [1, 5, 9].
1–4% of pregnancies globally are complicated by maternal cardiac disease, which accounts for a high percentage of maternal deaths [10, 11]. Maternal cardiac disease is the leading cause of indirect maternal deaths in the United Kingdom [12] and of maternal death in the United States [13]. The association between cardiac disease in pregnancy and adverse maternal outcomes is well established [10, 14,15,16,17,18,19]; however, neonatal outcomes are less well studied. Pregnant women with cardiac disease may have impaired maternal cardiovascular adaptation to pregnancy and hence impaired utero-placental circulation, potentially leading to an increased risk of adverse neonatal outcomes [20,21,22]. Evidence suggests reduced maternal left ventricular systolic function during pregnancy in women with heart disease leads to placental insufficiency and hence prevents the fetus from fulfilling its growth potential [17, 20, 21, 23]. However, it is not currently known which parameters of left ventricular function may best predict sub-optimal fetal growth.
Assessment of left ventricular function is often limited to an estimate of ejection fraction from transthoracic echocardiograms [24]. Two-dimensional speckle tracking echocardiography is a newer imaging technique, which allows segmental myocardial deformation analysis of the left ventricle to be calculated as global longitudinal strain (GLS) [25, 26]. GLS is an accurate and reproducible parameter to assess myocardial systolic function outside of pregnancy that allows subclinical dysfunction to be identified [27, 28]. However, studies have found mixed results regarding changes in left ventricular parameters, such as GLS, in healthy pregnancy and expected normal ranges have not been established [4, 6, 29, 30]. There is currently a lack of evidence to evaluate whether strain analysis would be a useful additional assessment to predict pregnancy outcomes in women with heart disease [31].
The aim of this study was to evaluate which parameters of left ventricular systolic function are most closely associated with risk of adverse neonatal outcomes in the context of maternal cardiac disease. Moreover, to assess whether the addition of strain calculations could improve prediction of adverse outcomes. The relationship between maternal cardiac function and utero-placental flow in women with cardiac disease will be explored to investigate the relationship with fetal growth. Better understanding of the relationship between maternal left ventricular systolic function, utero-placental flow, and adverse neonatal outcomes will allow for improvements in clinical management, such as closer fetal growth surveillance for pregnancies at highest risk.
Materials and methods
All women with cardiac disease that attended the pregnancy heart clinic at a single tertiary UK obstetrics centre between January 2019 and October 2021 were screened against inclusion criteria (Online Resource 1). 181 women attended the service, of whom 119 (66%) were eligible for inclusion in the analytic cohort (Online Resource 2).
Data extraction
Maternal demographic data were abstracted from electronic medical records; including maternal age (at time of delivery), pre-pregnancy BMI, parity status (prior to delivery), cardiac history, smoking status, cardiac medications, and comorbidities. The clinical history of the patient’s cardiac condition was recorded and used to classify women into one of six groups based on their primary cardiac condition (aortopathy, arrhythmia, cardiomyopathy, congenital heart disease, valvular heart disease, and other), and detailed subtyping was performed (Online Resource 3).
Data on neonatal outcomes were collected from maternal delivery records and the neonatal medical record; including mode of delivery, gestational age at delivery, birth weight, and sex. Birth-weight centile was calculated using Intergrowth-21 standards [32]. Adverse neonatal outcome were pre-defined as: low birth weight (< 2500 g), small-for-gestational-age (< 10th birth-weight centile), premature delivery (< 37 weeks’ gestation), intrauterine fetal death (death > 20 weeks’ gestation), and neonatal death (death within the first 30 days of delivery).
Umbilical artery Doppler pulsatility index (PI) was recorded from the last obstetric ultrasound scan prior to birth (gestational age range 30–37 weeks). The PI did not vary significantly with gestational age within this range.
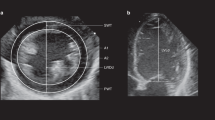
Calculation of echocardiographic parameters
Echocardiographic studies were identified for each participant and classified as: (i) pre-pregnancy (within 5 years of pregnancy), (ii) early pregnancy (0–28 weeks), and (iii) late pregnancy (> 28 weeks). All echocardiograms were performed in the left lateral decubitus position using GE Healthcare machines and a 2.5-MHz transducer. Parameters of left ventricular systolic function were calculated: GLS, radial strain at papillary muscle level (RS), ejection fraction (EF; Biplane Simpson’s method), averaged peak longitudinal myocardial velocities of the lateral and septal mitral valve annulus (Average S’), and cardiac output.
Two-dimensional speckle tracking echocardiography technique was used to calculate GLS and RS (Online Resource 4). Offline strain analysis was performed using EchoPAC (GE Healthcare; calculations performed according to the methods specified in Online Resource 5). A frame rate of 40–90 frames per second was required for analysis [33, 34]. Studies without required images, images with poor myocardial definition, or significant heart rate variability were excluded (Online Resource 6).
All strain measurements were performed by a single trained observer. To assess intra-observer variability of GLS and RS, repeat measurements were performed 9 months after initial measurements on 25 randomly chosen echocardiograms and intra-class correlation coefficients (ICC) were calculated. The repeatability of the measurements was strong for both GLS (ICC 0.93, 95% CI 0.82–0.98) and RS (ICC 0.76, 95% CI 0.43–0.91). Inter-observer variability was assessed using GLS measurements performed by further 3 independent accredited echocardiographers using blinded images from 5 echocardiograms (ICC 0.89, 95% CI 0.65–0.99).
Cardiac output was calculated as the product of stroke volume and heart rate. Stroke volume was calculated using the cross-sectional area of the left ventricular outflow tract measured in the parasternal long axis in systole and the velocity time integral of the pulsed wave Doppler waveform measured in the five-chamber or three-chamber view. Images with poor Doppler alignment were excluded. Heart rate was averaged from 4 images obtained during the echocardiogram.
Statistical analysis
The Kolmogoroff–Smirnoff test was used to assess normality of the distribution of data. Continuous data are reported as mean and standard deviation (SD) or median with interquartile range (IQR), depending on the distribution. Categorical data are presented as absolute numbers and percentages. Univariate analyses were performed to compare demographics between women with adverse neonatal outcomes and no adverse neonatal outcomes. Intergroup comparison was performed using one-way ANOVA, Student’s t test, or the Mann–Whitney test for numerical data and Pearson’s chi-squared test for categorical data. Correlations between numeric variables were assessed using linear regression models. The association between adverse neonatal outcomes and each parameter of left ventricular systolic function was assessed using binomial logistic regression models, with and without adjustment for beta-blockade. All data analysis was performed using GraphPad Prism (v9.2.0) and R statistical software (v4.1.1). A two-tailed p value of 0.05 was considered statistically significant.
Results
Neonatal outcomes
Adverse neonatal outcomes occurred in 28/119 (24%) pregnancies (Table 1). Premature delivery (n = 19/119, 16%) and low birth weight (n = 19/119, 16%) were the most common neonatal complications (Table 1). Of the 19 premature infants, 47% (9/19) were iatrogenic early deliveries due to maternal cardiac disease (Table 1). 20% (24/119) women required hospital admission during pregnancy due to their cardiac condition; 67% (16/24) of these women had an adverse neonatal outcome (Table 1). Vaginal delivery was the most frequent mode of delivery (60%; Table 1). The median gestational age at delivery was 39 weeks (IQR 37–39 weeks) and median birth weight was 3090 g (IQR 2680–3400 g; Table 1).
There were no significant differences in the maternal characteristics of women who experienced adverse neonatal outcomes compared to those with healthy neonates (Table 2).
Maternal left ventricular function by lesion type was characterised (Online Resource 7). Adverse neonatal outcomes occurred most frequently in women with cardiomyopathy and valvular heart disease (n = 15/119, 12.6%; Table 3) compared to other forms of heart disease. Small-for-gestational-age infants were significantly more likely in women with cardiomyopathy compared to women with other cardiac conditions (56% vs 44%, p = 0.02; Table 3).
Umbilical artery PI was significantly higher in women with adverse neonatal outcomes than those with healthy neonates (1.05 ± 0.24 PI vs. 0.87 ± 0.13 PI, p < 0.0001; Table 1). Umbilical artery PI was significantly higher in women with cardiomyopathy than other heart disease (1.00 ± 0.23 PI vs. 0.88 ± 0.16 PI, p = 0.007; Table 3).
Women treated with beta-blockade during pregnancy were significantly more likely to experience adverse neonatal outcomes (64% vs. 40%, p = 0.03; Table 2), although this association may not be causal. There was no significant difference between cardiac output in late pregnancy between women who took beta blockers and those who did not (5.61 ± 1.03 L/min vs 5.43 ± 0.99 L/min, p = 0.781).
Echocardiographic assessment of left ventricular systolic function during pregnancy
Pre-pregnancy echocardiograms were available in 34/119 (29%) women. 79/119 (66%) women had an early pregnancy echocardiogram (mean 19 ± 6 weeks, range 2–27 weeks) and 83/119 (70%) women had a late pregnancy echocardiogram (mean 33 ± 3 weeks, range 28–39 weeks).
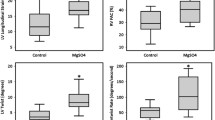
Cardiac output significantly increased during pregnancy. The most significant increase occurred between pre-pregnancy and early pregnancy (4.97 ± 1.00 L/min to 5.52 ± 1.16 L/min, p = 0.03), with no significant further increase in late gestation (Fig. 1A). The increase in cardiac output was primarily due to a significant increase in heart rate during pregnancy (73 ± 13 bpm to 83 ± 14 bpm, p = 0.0008; Fig. 1B). Overall, there was no significant change in stroke volume across the study time points (p = 0.80; Fig. 1C).
During pregnancy GLS decreased from − 18.70% pre-pregnancy to − 17.27% in late pregnancy (Fig. 2A), but this did not meet the threshold for statistical significance (p = 0.16). There were no significant changes in RS, EF or Average S’ across pregnancy (Fig. 2B–D).
Left ventricular systolic function and adverse neonatal outcomes
In early pregnancy, the average S’ was significantly lower in women with adverse neonatal outcomes versus those with healthy neonates (9.07 ± 2.52 cm/s vs. 10.21 ± 1.88 cm/s, p = 0.03; Table 4). Other parameters of cardiac function in early pregnancy did not show significant associations with neonatal outcome (Table 4).
Average S’ was also significantly reduced in late pregnancy in women with adverse neonatal outcomes (8.67 ± 1.88 cm/s vs. 9.95 ± 1.84 cm/s, p = 0.02; Table 5). Additionally, cardiac output was significantly lower in women with adverse neonatal outcomes versus those with healthy neonates (5.11 ± 1.02 L/min vs. 5.77 ± 0.94 L/min, p = 0.02; Table 5). Women with adverse neonatal outcomes had a significantly lower stroke volume (61.66 ± 14.56 ml vs. 70.88 ± 13.92, ml p = 0.01; Table 5) but no significant difference in heart rate (84 ± 13 bpm vs. 83 ± 15 bpm, p = 0.75; Table 5). Other parameters cardiac function in late pregnancy did not show significant associations with neonatal outcome (Table 5).
All significant associations between parameters of left ventricular systolic function and adverse neonatal outcome in early and late pregnancy remained significant following adjustment for beta-blockade in pregnancy.
Left ventricular systolic function and neonatal birth-weight centile
In early pregnancy, there were no systolic parameters of left ventricular function that were significantly associated with birth-weight centile. In late pregnancy, there was a significant association between birth-weight centile and both GLS (R2 = 0.11, p = 0.04; Fig. 3A) and cardiac output (R2 = 0.18, p = 0.0002; Fig. 3B). When cardiac output was further investigated, there was a significant positive association between stroke volume and birth-weight centile (R2 = 0.06, p = 0.04), but this did not meet statistical significance for heart rate (R2 = 0.03, p = 0.10). No other systolic parameters of left ventricular function were significantly associated with birth-weight centile in late pregnancy.
Left ventricular systolic function and utero-placental circulation
In early pregnancy, there were no systolic parameters of left ventricular function that were significantly associated with umbilical artery Doppler PI. In late pregnancy, there was a significant association between umbilical artery Doppler PI and both GLS (R2 = 0.14, p = 0.03; Fig. 4A) and average S’ (R2 = 0.20, p < 0.0001; Fig. 4B). Other parameters of left ventricular systolic function in late pregnancy did not show significant associations with umbilical artery Doppler PI.
Discussion
We show that adverse neonatal outcomes are significantly associated with specific parameters of maternal left ventricular systolic function in both early (average S’) and late (average S’ and cardiac output) pregnancy. Ejection fraction, which is the most commonly assessed measure of left ventricular systolic function [35], was not a significant predictor of adverse neonatal outcome at any stage. Moreover, GLS was also not significantly associated with adverse neonatal outcomes, although lower GLS in late pregnancy was associated with lower birth-weight centile.
Overall, 24% of women in our study experienced adverse neonatal outcomes, which is a similar incidence to other reported cohorts of women with cardiac disease and significantly higher than the expected incidence in a healthy population [20]. In our cohort, 54% of adverse neonatal outcomes occurred in women with valvular heart disease or cardiomyopathy, which is in keeping with the high risks previously reported for these women with these pathologies [14]. Overall, 20% of women with heart disease required hospital admission during pregnancy due to cardiac causes and 66% of these women had an adverse neonatal outcome. These findings highlight the risks associated with pregnancy in women with cardiac disease and the importance of close surveillance by specialist multi-disciplinary teams.
In late pregnancy, we show that cardiac output was significantly lower in women with cardiac disease who went on to have adverse neonatal outcomes than in those with healthy neonates. A similar relationship between cardiac output and neonatal outcome has previously been suggested in women with no known cardiac disease [21], and further evidence suggests that cardiac output may not increase appropriately during pregnancy in women with cardiac disease who have adverse neonatal outcomes [20]. We show significantly reduced stroke volume in late pregnancy in women with adverse neonatal outcomes but no significant difference in heart rate. In cases of adverse outcome, maternal cardiac output may be increasingly limited as pregnancy progresses due to impaired myocardial contractility, suggested by reduced average S' and stroke volume. This is also in keeping with our observation of an excess of adverse outcomes, specifically SGA neonates, in women with cardiomyopathy or valvular lesions compared to other forms of heart disease. The identification of cardiac output that is not appropriately increased by the third trimester should alert the clinician to the increased risk of complications in the neonate, potentially prompting increased surveillance of fetal growth. This finding requires prospective verification in a larger cohort, with appropriate power to determine a threshold for intervention. The association between reduced average S’ and higher umbilical artery Doppler PI in late pregnancy suggests that impaired utero-placental circulation supports the causal link between reduced fetal growth and maternal cardiac disease [17, 36].
We show that by early pregnancy, average S’ was already significantly lower in women who went on to have adverse neonatal outcomes and that this association was maintained into late pregnancy. This suggests decreased longitudinal myocardial velocities in women with heart disease who have adverse neonatal outcomes and supports previous findings that suggest impaired long-axis shortening in women with fetal growth restriction [21]. We investigated the possibility that strain calculation might offer additional clinical benefit in identifying subclinical myocardial dysfunction in women with heart disease and hence increased risk of adverse neonatal outcomes. However, neither GLS nor RS was significantly altered in early or late pregnancy in women with heart disease who had adverse neonatal outcomes compared to those with healthy neonates. Our results suggest that tissue Doppler imaging may be a more appropriate and sensitive parameter to identify myocardial dysfunction to predict adverse outcomes in this cohort of women, and may be a useful parameter to consider in the evaluation of cardiac function in pregnancy. However, there are significant limitations in calculating GLS retrospectively and the possibility that strain could be a useful additional tool to predict outcomes in women with heart disease should not be dismissed without a prospective evaluation.
Our study methodology has significant advantages, including a relatively large [20] and well-phenotyped cohort of women with heart disease, all of whom were managed by a small group of clinicians according to standardised guidelines [10] within a specialised multi-disciplinary service. We also recognise limitations in our study, particularly that women did not have an echocardiogram at all study time points, thus limiting our ability to perform longitudinal assessment of systolic function. Ideally, analysis would have occurred separately in the first and second trimester; however, due to heterogeneity in timing, these were combined as ‘early pregnancy’. Furthermore, a larger sample size would have allowed additional sub-group analyses to be performed, for example more detailed sub-grouping of cardiac pathologies.
Conclusions
Women with cardiac disease are at increased risk of neonatal complications, in particular fetal growth restriction. Our data suggest a significant association between late pregnancy cardiac output and birth-weight centile. Cardiac output in women with heart disease who have adverse neonatal outcomes is significantly lower in late pregnancy than in those who have healthy neonates, which is likely to impact on the utero-placental circulation. We identify average S’ and cardiac output as parameters of left ventricular systolic function that are significantly associated with risk of adverse neonatal outcomes in women with heart disease. These findings could help refine identification of women whose fetuses are at highest risk of adverse outcome and therefore enable clinicians to target additional fetal surveillance during pregnancy complicated by heart disease.
References
Sanghavi M, Rutherford JD (2014) Cardiovascular physiology of pregnancy. Circulation 130:1003–1008. https://doi.org/10.1161/CIRCULATIONAHA.114.009029
Liu S, Elkayam U, Naqvi TZ (2016) Echocardiography in pregnancy: part 1. Curr Cardiol Rep 18:92. https://doi.org/10.1007/s11886-016-0760-7
Desai DK, Moodley J, Naidoo DP (2004) Echocardiographic assessment of cardiovascular hemodynamics in normal pregnancy. Obstet Gynecol 104:20–29. https://doi.org/10.1097/01.AOG.0000128170.15161.1d
Estensen ME, Beitnes JO, Grindheim G, Aaberge L, Smiseth OA, Henriksen T, Aakhus S (2013) Altered maternal left ventricular contractility and function during normal pregnancy. Ultrasound Obstet Gynecol 41:659–666. https://doi.org/10.1002/uog.12296
Chattopadhyay R, Olwell B, Bhagra CJ (2021) Maternal cardiac disease in pregnancy. Obstet Gynaecol Reprod Med 32:1–7. https://doi.org/10.1016/j.ogrm.2021.11.001
Sengupta SP, Bansal M, Hofstra L, Sengupta PP, Narula J (2017) Gestational changes in left ventricular myocardial contractile function: new insights from two-dimensional speckle tracking echocardiography. Int J Cardiovasc Imaging 33:69–82. https://doi.org/10.1007/s10554-016-0977-y
Visentin S, Palermo C, Camerin M, Daliento L, Muraru D, Cosmi E, Badano LP (2017) Echocardiographic techniques of deformation imaging in the evaluation of maternal cardiovascular system in patients with complicated pregnancies. Biomed Res Int 2017:4139635. https://doi.org/10.1155/2017/4139635
Keser N (2006) Echocardiography in pregnant women. Anadolu Kardiyol Derg 6:169–173
Adam K (2017) Pregnancy in women with cardiovascular diseases. Method Debakey Cardiovasc J 13:209–215. https://doi.org/10.14797/mdcj-13-4-209
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lungqvist C, Cífková R, De Bonis M, Lung B et al (2018) 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J 7:3165–3241. https://doi.org/10.1093/eurheartj/ehy340
Kotit S, Yacoub M (2021) Cardiovascular adverse events in pregnancy: a global perspective. Glob Cardiol Sci Pract 2021:e202105. https://doi.org/10.21542/GCSP.2021.5
Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ (Eds.) on behalf of MBRRACE-UK. Saving lives, improving mothers’ care—lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015–17. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2019
Building US. Capacity to Review and Prevent Maternal Deaths (2018) Report from nine maternal mortality review committees. Retrieved from http://reviewtoaction.org/Report_from_Nine_MMRCs
Owens A, Yang J, Nie L, Lima F, Avila C, Stergiopoulos K (2018) Neonatal and maternal outcomes in pregnant women with cardiac disease. J Am Heart Assoc 7:e009395. https://doi.org/10.1161/JAHA.118.009395
Roos-Hesselink JW, Ruys TPE, Stein JI, Thilén U, Webb GB, Niwa K, Kaemmerer H et al (2013) Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. Eur Heart J 34:657–665. https://doi.org/10.1093/eurheartj/ehs270
Koutrolou-Sotiropoulou P, Parikh PB, Miller C, Lima FV, Butler J, Stergiopoulos K (2015) Impact of heart disease on maternal and fetal outcomes in pregnant women. Am J Cardiol 116:474–480. https://doi.org/10.1016/j.amjcard.2015.04.063
Cauldwell M, Steer P, Sterrenburg M, Wallace S, Malin G, Ulivi G, Everett T et al (2019) Birth weight in pregnancies complicated by maternal heart disease. Heart 105:391–398. https://doi.org/10.1136/heartjnl-2018-313551
Lima FV, Yang J, Xu J, Stergiopoulos K (2017) National trends and in-hospital outcomes in pregnant women with heart disease in the United States. Am J Cardiol 119:1694–1700. https://doi.org/10.1016/j.amjcard.2017.02.003
Lima F, Nie L, Yang J, Owens A, Dianati-Maleki N, Avila C, Stergiopoulos K (2019) Postpartum cardiovascular outcomes among women with heart disease from a nationwide study. Am J Cardiol 123:2006–2014. https://doi.org/10.1016/j.amjcard.2019.03.012
Wald RM, Silversides CK, Kingdom J, Toi A, Lau C, Mason J, Colamn JM et al (2015) Maternal cardiac output and fetal doppler predict adverse neonatal outcomes in pregnant women with heart disease. J Am Heart Assoc 4:1–11. https://doi.org/10.1161/JAHA.115.002414
Bamfo JEAK, Kametas NA, Turan O, Khaw A, Nicolaides KH (2006) Maternal cardiac function in fetal growth restriction. BJOG An Int J Obstet Gynaecol 113:784–791. https://doi.org/10.1111/j.1471-0528.2006.00945.x
Cornette J, Ruys TPE, Rossi A, Rizopoulos D, Takkenberg JJM, Karamermer Y, Opić P et al (2013) Hemodynamic adaptation to pregnancy in women with structural heart disease. Int J Cardiol 168:825–831. https://doi.org/10.1016/j.ijcard.2012.10.005
Pieper PG, Balci A, Aarnoudse JG, Kampman MAM, Sollie KM, Groen H, Mulder BJM et al (2013) Uteroplacental blood flow, cardiac function, and pregnancy outcome in women with congenital heart disease. Circulation 128:2478–2487. https://doi.org/10.1161/CIRCULATIONAHA.113.002810
Cole GD, Dhutia NM, Shun-Shin MJ, Willson K, Harrison J, Raphael CE, Zolgharni M et al (2015) Defining the real-world reproducibility of visual grading of left ventricular function and visual estimation of left ventricular ejection fraction: impact of image quality, experience and accreditation. Int J Cardiovasc Imaging 31:1303–1314. https://doi.org/10.1007/s10554-015-0659-1
Blessberger H, Binder T (2010) Two dimensional speckle tracking echocardiography: basic principles. Heart 96:716–722. https://doi.org/10.1136/hrt.2007.141002
Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, Pedri S et al (2014) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16:1–11. https://doi.org/10.1093/ehjci/jeu184
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH (2014) Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol 63(25):2751–2768. https://doi.org/10.1016/j.jacc.2014.01.073
Marwick TH (2018) Ejection fraction pros and cons: JACC state-of-the-art review. J Am Coll Cardiol 72:2360–2379. https://doi.org/10.1016/j.jacc.2018.08.2162
Savu O, Jurcuţ R, Giuşcǎ S, van Mieghem T, Gussi I, Popescu BA, Ginghina C et al (2012) Morphological and functional adaptation of the maternal heart during pregnancy. Circ Cardiovasc Imaging 5:289–297. https://doi.org/10.1161/CIRCIMAGING.111.970012
Cong J, Fan T, Yang X, Squires JW, Cheng G, Zhang L, Zhang Z (2015) Structural and functional changes in maternal left ventricle during pregnancy: a three-dimensional speckle-tracking echocardiography study. Cardiovasc Ultrasound 13:1–10. https://doi.org/10.1186/1476-7120-13-6
O’Kelly AC, Sharma G, Vaught AJ, Zakaria S (2019) The use of echocardiography and advanced cardiac ultrasonography during pregnancy. Curr Treat Options Cardiovasc Med. https://doi.org/10.1007/s11936-019-0785-5
Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Ismail LC, Lambert A, Jaffer YA et al (2014) International standards for fetal growth based on serial ultrasound measurements: The Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet 384:869–879. https://doi.org/10.1016/S0140-6736(14)61490-2
Johnson C, Kuyt K, Oxborough D, Stout M (2019) Practical tips and tricks in measuring strain, strain rate and twist for the left and right ventricles. Echo Res Pract 6:R87-98. https://doi.org/10.1530/ERP-19-0020
Mor-Avi V, Lang RM, Badano LP, Belohlavek M, Cardim NM, Derumeaux G, Galderisi M et al (2011) Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications: Endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr 24:277–313. https://doi.org/10.1016/j.echo.2011.01.015
Potter E, Marwick TH (2018) Assessment of left ventricular function by echocardiography: the case for routinely adding global longitudinal strain to ejection fraction. JACC Cardiovasc Imaging 11:260–274. https://doi.org/10.1016/j.jcmg.2017.11.017
Gelson E, Curry R, Gatzoulis MA, Swan L, Lupton M, Steer P, Johnson M (2011) Effect of maternal heart disease on fetal growth. Obstet Gynecol 117:886–891. https://doi.org/10.1097/AOG.0b013e31820cab69
Funding
CEA is supported by a Medical Research Council New Investigator Grant (MR/T016701/1) and the NIHR Cambridge Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to study design and manuscript drafting. EJE collected the data and analysed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the institution as a retrospective service evaluation (Clinical Project ID: 3420; PRN 9402, Approval date 11/12my/2020) and supported by HRA approval to analyse predictors of adverse pregnancy outcomes (REC reference 12/SC/0344).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eggleton, E.J., Bhagra, C.J., Patient, C.J. et al. Maternal left ventricular function and adverse neonatal outcomes in women with cardiac disease. Arch Gynecol Obstet 307, 1431–1439 (2023). https://doi.org/10.1007/s00404-022-06635-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06635-9