Abstract
Background
Globally, antimicrobial resistance (AMR) restricted the armamentarium of the health care providers against infectious diseases, mainly due to the emergence of multidrug resistant. This review is aimed at providing contemporary bacterial profile and antimicrobial resistance pattern among pregnant women with significant bacteriuria.
Methods
Electronic biomedical databases and indexing services such as PubMed/MEDLINE, Web of Science, EMBASE and Google Scholar were searched. Original records of research articles, available online from 2008 to 2021, addressing the prevalence of significant bacteriuria and AMR pattern among pregnant women and written in English were identified and screened. The relevant data were extracted from included studies using a format prepared in Microsoft Excel and exported to STATA 14.0 software for the outcome measure analyses and subgrouping.
Results
The data of 5894 urine samples from 20 included studies conducted in 8 regions of the country were pooled. The overall pooled estimate of bacteriuria was 15% (95% CI 13–17%, I2 = 77.94%, p < 0.001) with substantial heterogeneity. The pooled estimate of Escherichia coli recovered from isolates of 896 urine samples was 41% (95% CI 38–45%) followed by coagulase-negative Staphylococci, 22% (95% CI 18–26%), Staphylococcus aureus, 15% (95% CI 12–18%), Staphylococcus saprophytic, 12% (95% CI 6–18%) Proteus mirabilis, 7% (95% CI 4–10%), Enterococcus species, 6% (0–12%), Pseudomonas aeruginosa, 4% (2–6%), Citrobacter species, 4% (95% CI 2–4%), Group B streptococcus, 3% (1–5%), and Enterobacter species, 2% (1–4%). Multidrug resistance proportions of E. coli, Klebsiella species, Staphylococcus aureus and Coagulase negative staphylococci, 83% (95% CI 76–91%), 78% (95% CI 66–90%), 89% (95% CI 83–96%), and 78% (95% CI 67–88%), respectively.
Conclusion
The result of current review revealed the occurrence of substantial bacteriuria among pregnant women in Ethiopia. Resistance among common bacteria (E. coli, Klebsiella species, Staphylococci species) causing UTIs in pregnant women is widespread to commonly used antibiotics. The high rate of drug resistance in turn warrants the need for regular epidemiological surveillance of antibiotic resistance and implementation of an efficient infection control and stewardship program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infection (UTI) is referred to the invasion of microorganism and their subsequent growth in any part of the urinary tract including the kidneys, ureters, bladder, and urethra [1]. It is one of the most common infectious disease resulting in over 150 million cases per year globally [1, 2]. Although both males and females may become infected by UTI, females are more likely to develop UTI compared to males due to short urethra, proximity to anus which causes easy contamination of the urinary tract with fecal microbial, hormonal changes and pregnancy [3].
The most frequent bacterial infection during pregnancy is urinary tract infection, which is linked to preeclampsia, low birth weight, premature delivery, and intrauterine growth restriction [4]. UTIs are classified as either asymptomatic or symptomatic bacteriuria during pregnancy. The presence of a significant amount of bacteria (105 colony-forming unit (CFU)/ml of cultured urine) in the absence of signs and symptoms of UTI is known as asymptomatic bacteriuria (ABU) [5, 6]. If left untreated, asymptomatic bacteriuria occurs 2–15% of pregnant women and is a common risk factor for pyelonephritis [7, 8]. Although, recent studies question the benefit of ABU treatment particularly, in low-risk pregnant women [7,8,9], timely initiation of antibiotic as soon as significant bacteriuria is diagnosed likely reduce the incidence of pyelonephritis, preterm delivery, and low birth weight [6]. Several factors are associated with an increased frequency of bacteriuria during pregnancy. These will include age, presence of genitourinary abnormalities (kidney, ureteral and bladder stones, tumors, urethral strictures, vesico-ureteric reflux), anemia, sexual activity, decreased immunity, lower socioeconomic classes, past history of UTI, multiparity and gestational age [10, 11]. For example, the prevalence for bacteriuria increases with age from about 1% in females aged 5–14 years [12].
Escherichia coli is the most common pathogenic microorganisms associated with both asymptomatic and symptomatic bacteriuria and accounting up 60–80% of all UTIs in pregnancy [13, 14]. Other bacteria identified in UTIs during pregnancy include Klebsiella pneumoniae, Staphylococcus aureus, Coagulase negative staphylococci, Enterobacter spp., Pseudomonas aeruginosa, Enterococcus spp., Proteus mirabilis, and others [14].
Antimicrobial resistance (AMR) continued to increase as a result of the rapid emergence of resistant bacteria worldwide [15]. This is demonstrated by recent world health organization (WHO) surveillance data from 22 high- and low-income countries which reported a high level of AMR to numerous bacterial infections and identified E. coli and K. pneumoniae as the most common resistant pathogen [16]. In addition, meta-analysis of 23 studies from different part of the world reported a high prevalence of extended‐spectrum beta‐lactamase (ESBL)-producing Enterobacteriaceae in pregnant women with significant bacteriuria [17]. The resistance of uropathogenic to third-generation cephalosporin, amoxicillin, and other antibiotics in pregnant women especially, in Africa pose a big challenge to the management of UTI during pregnancy [17, 18].
Routine antimicrobial susceptibility test is a major challenge in the majority of low-income countries [19]. As a result, treatment of infectious disease including UTI in pregnant women is initiated empirically and most pregnant women treated with an unnecessary antibiotic which further contributes to the emergence of resistant pathogens [20]. In Ethiopia, there are several studies conducted at different regions and hospitals regarding the bacterial profile and antimicrobial susceptibility patterns of UTI in pregnant women [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. However, there is no pooled prevalence data at the national level which alert health care providers and clinicians on the current prevalence of AMR in UTI during pregnancy. Therefore, this systematic review and meta-analysis is aimed at providing contemporary bacterial profile and antimicrobial resistance pattern among pregnant women with significant bacteriuria.
Methods
Reporting
This systematic review and meta-analysis is based on a recommended methodology by the Joanna Briggs Institute’s approach [41] and followed the Preferred Reporting Items for Systematic review and Meta-Analysis for Protocols (PRISMA-P) 2015 guidelines [42].
Search strategy and data extraction
The present review exhaust all available full-text articles in English language (without date restrictions) indexed in the following major scientific databases: MEDLINE (via PubMed), Web of Science (via Saudi Digital Library), Excerpta Medica dataBASE (EMBASE) and Google scholar. To identify potential search terms and retrieve the best set of results possible, a pre-determined MEDLINE search strategy was constructed using the PICO (patients, interventions, comparators, outcomes) equivalents: patients, exposures of interests, comparison, and outcomes. Accordingly the PECO framework used in our search was described as follows: population (P): pregnant women with bacteriuria in Ethiopia; exposure (E): significant bacteriuria; comparison (C): pregnant women without significant bacteriuria in Ethiopia; outcome (O): bacteria profile, antibiotic resistance profile.
A manual search for additional relevant studies using references from retrieved articles and related systematic reviews was also performed to identify original articles we might have missed. In addition, to find unpublished papers relevant to this systematic review and meta-analysis, some research centers and digital library of higher institutions found in Ethiopia was also explored. The search strings or terms were stemmed from the following keywords: pregnant women, pregnant mother, pregnancy, bacteriuria, urinary tract infection, UTI, significant bacteriuria, uropathogens, antibiotic resistance, antimicrobial resistance, multidrug resistance and Ethiopia. In the advanced searching databases, the searching strategy was built based on the above-mentioned terms using the “Medical Subject Headings (MeSH)” and “All fields” by linking “AND” and “OR” Boolean operator terms as appropriate. The pre-determined MEDLINE search strategy was adopted in searching relevant articles in all other databases. Modifications to indexing terms (e.g., Medical Subject Headings, field tags) for other databases were applied as necessary.
Data extraction and quality assessment
Data extraction was implemented using a standard and extraction format adapted from the Joanna Briggs Institute (JBI) data extraction format [41]. Screening by title, abstract, and full text and data extraction were done independently by two authors (LC and TM) from the published studies and recorded by Microsoft excel spreadsheet. Consensus was reached by discussion whenever there was disagreement. References and data for each study were carefully cross-checked to ensure that no overlapping data were present and to maintain the integrity of the meta-analysis. Endnote citation manager software version X9 for Windows was utilized to collect and organize search outcomes and for removal of duplicate articles. The retrieved articles were screened according to predefined inclusion and exclusion criteria. We extracted information on name of the first author and year of publication, study period, study design, study region, total sample size, number of isolates, criteria for diagnosis of significant bacteriuria, number and percentage of gram positive and gram negative bacteria, number of asymptomatic and symptomatic bacteriuria and the prevalence and antimicrobial resistance patterns of common bacteria identified. The JBI quality appraisal criteria established for cross-sectional were used to measure the quality of the studies included in the meta-analysis. The JBI’s appraisal criteria consist of nine questions. The first three questions measure about appropriateness of the sampling frame to address the target population, whether participants sampled in appropriate way and sample size is adequate enough. The next three questions measure whether the study subjects and setting of the study described in detail, the data analysis conducted with sufficient coverage of the identified samples and validated for identification method of the condition. The last three questions measure the reliability of measuring the condition in a standard way, the appropriateness of statistical analysis and the adequacy of response rate.
Inclusion and exclusion criteria
We included published and unpublished (Addis Ababa University) studies reported bacterial profile and their antimicrobial-resistance in pregnant women. We also included studies published in English, human studies and conducted only in Ethiopia. We excluded studies in other population other than in pregnancy, qualitative studies, review paper, commentaries, case series, case reports, conference proceeding and abstracts.
Data processing and analysis
Data were extracted in Microsoft Excel format, followed by analysis using STATA Version 14.0 statistical software. Random effect model was applied to estimate the pooled estimate and antimicrobial resistance pattern of the isolates. We conducted meta-regression to understand the source of heterogeneity and pooled the estimate using “metaprop” command. Potential source of heterogeneity was investigated by subgroup and meta-regression analysis. The existence of heterogeneity among studies were examined by I2 heterogeneity test, in which 0–40%, 50–60%, 50–90% and 75–100% represented low, moderate, substantial and considerable heterogeneity, respectively. I2 heterogeneity test of ≥ 50% and a p value of < 0.05 was assured the presence of heterogeneity. Thus, the DerSimonian–Laired random effects model was employed [43]. Subgroup analysis was done based on the patients symptoms status (asymptomatic vs. symptomatic), bacterial isolates (Gram positive vs. Gram negative), geographical region, study period (before 2015 vs. 2015 or after) to minimize the random variations between the point estimates of the primary study. Visual inspection of the funnel plots and Egger’s regression test was used for evaluating the possibility of publication bias. Due to the presence of publication bias the result was corrected by Duval and Tweedie’s trim and fill analysis. Forest plot format was used to present the pooled estimate with 95% CI. Two-sided p values < 0.05 were accepted as statistical significant.
Outcome measurement
This review has three major outcomes. The first outcome was to determine the pooled estimates of significant bacteriuria among pregnant women in Ethiopia. The second outcome was to assess the rate of antimicrobial resistance of common bacteria to common antibiotics used in the country for the treatment of urinary tract infection and finally pattern of multidrug resistance of common uropathogens among pregnant women. The pooled estimates of bacterial isolates and their antimicrobial resistance isolates were calculated using the following formula: a pooled estimate of each isolate was the number of isolate divided by the number of all the detected bacteria isolates. The pooled estimates of resistance to each tested antibiotic was calculated by dividing the number of resistance isolates of each species to total number of all the detected isolates of the species. Multidrug resistance was defined as resistance to at least to two antibiotics to the isolated Gram-positive bacteria for the various antibiotics.
Results
Literature identification and characteristics of included studies
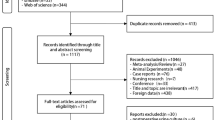
Of 1204 identified studies (Medline = 642, Web of Science = 321, EMBASE = 134, Google scholar = 108, and manual search = 3), 673 duplicates were excluded. We further excluded 358 studies because they were not relevant up-on reviewing the titles. Then the full-text of the remaining 173 articles was downloaded and fully assessed for fulfilling the required criteria. We again excluded 150 articles because they were not about pregnant women (N = 150) and not done in Ethiopia (N = 3). Finally, a total of 20 studies were included in this review that met the inclusion criteria [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. Figure 1 summarizes the process of identification, screening, checking for eligibility and inclusion into the final analyses.
All of these studies were conducted from January 2005 to September 2019 and published online from 2008 to 2020. All of the studies were cross sectional in design. All of the studies published on peer review journals except two unpublished data which were obtained from Addis Ababa digital library [44,45,46,47,48]. About one-third of the studies were conducted in Amhara region (n = 6) [21, 22, 24, 25, 31, 33] followed by three studies in Addis Ababa city [23, 32, 40], three in Tigray region [26, 37, 38], three in SNNPR [28, 36, 39], two in Oromia region [27, 30], one in Somalia region [29], one in Dire Dawa city [34], and one in Harari region [35]. Sample size of the studies included ranged from 168 [49] to 414 [50]. The prevalence of significant bacteriuria ranged from 7.8 [39] to 24% [34]. Table 1 summarizes the baseline characteristics, tests used, diagnostic criteria, and prevalence of significant bacteriuria among pregnant women.
Pooled estimate of significant bacteriuria
A total of 20 studies reported that significant bacteriuria was detected in 896 urine samples out of a total 5894 samples taken from pregnant women during their antenatal care visit to the health care system. In random-effect model, the overall prevalence of significant bacteriuria was 15% (95% CI 13–17%) with substantial heterogeneity (I2 = 77.94%, p < 0.001) across the studies (Fig. 2).
Subgroup analysis
Subgroup analyses revealed that the proportion of pregnant women developed asymptomatic bacteriuria was 12% (95% CI 9–15%, I2 = 89.09%, p < 0.001) as shown in Fig. 3, whereas only 6% (95% CI 4–9%, I2 = 91.33%, p < 0.001, Fig. 4) developed symptomatic bacteriuria with no statistical significant difference (p = 0.14) between the two. Gram-negative bacteria accounted for 64% (95% CI 57–69%, I2 = 72.80%, p < 0.001, Fig. 5) of bacteriuria in participants included in this study, whereas Gram-positive counterparts accounted for 36% (95% CI 30–43%, I2 = 78.91%, p < 0.001, Fig. 6) with a statistically significant difference (p = 0.001).
Another subgroup analysis by study period also revealed that the prevalence of significant bacteriuria before 2015 was 13% (95% CI 10–17%, I2 = 69.40%, p < 0.001) while it was 16% (95% CI 14–19%, I2 = 78.39%, p < 0.001) after 2015 with no significant statistical difference (p = 0.16) (Fig. 7). Lastly, subgroup by region showed that the prevalence of significant bacteriuria among pregnant women was 16% in Addis Ababa city, 13% in Amhara region, 14% in Dire Dawa city, 20% in Harari region, 17% in Oromia region, 13% in Somalia region, 13% in SNNP region and 18% in Tigray region with no significant difference across the regions (p = 0.46) (Fig. 8).
Meta-regression
Just to identify the sources of heterogeneity, meta-regression was conducted using geographic region, year of publication, and sample size as a covariate. The analysis showed that there is no effect of geographic region (supplementary 1), year of publication (supplementary 2) and sample size (supplementary 3) on heterogeneity between studies (Table 2).
Types of bacterial isolates
Data of 5894 urine samples from 20 studies conducted in 8 regions of the country were pooled. Eleven different types of bacterial isolates were extracted from studies included in this review. The most common bacterial isolate of both asymptomatic and symptomatic bacteriuria was E. coli with an overall prevalence of 41% (95% CI 38–45%, Fig. 9) followed by Coagulase negative staphylococci 22 (18–26% Fig. 10), Staphylococcus aureus 15% (12–18%, Fig. 11), Staphylococcus saprophyticus 12% (7–17%, Supplementary 4), Klebsiella species 9% (7–11%, Fig. 12), Proteus mirabilis 7% (4–10%, Supplementary 5), Enterococcus species 6% (0–12%, Supplementary 6), P. aeruginosa 4% (2–6%, Supplementary 7), Citrobacter species 4% (2–6%, Supplementary 8), Group B streptococcus 3% (1–5%, Supplementary 9) and Enterobacter species 2% (1–4%, Supplementary 10) as depicted on Table 3.
Antibiotic resistance patterns of E. coli and Klebsiella species isolates
Table 4 shows that antibiotic resistance pattern for E. coli isolated of significant bacteriuria among Ethiopian pregnant women who attained the antenatal care, the most resistance was to amoxicillin with prevalence of 81% (95% CI 69–94%), followed by ampicillin, amoxicillin–clavulanic acid, and sulfamethoxazole–trimethoprim with prevalence of 80% (95% CI 72–88%), 46% (95% CI 29–63%), 40% (95% CI 26–53%), respectively. The lowest resistance was observed to nitrofurantoin with a prevalence of 19% (95% CI 11–27%) followed by ceftriaxone, ciprofloxacin, ceftazidime, gentamicin and norfloxacin with a prevalence of 20%, 21%, 22%, 28% and 28%, respectively. Similarly, the highest rate of resistance by Klebsiella species was observed to ampicillin with a prevalence of 76% (95% CI 66–86%) while the lowest resistance was to ceftriaxone with a prevalence of 20% (95% CI 13–28%) as shown in Fig. 13. Three studies reported that the pooled prevalence of ESBL E. coli was 19% (95% CI 10–27%, I2 = 8.16%, p = 0.34, Fig. 14), whereas the prevalence of ESBL Klebsiella species was 33% (95% CI 3–64%, Fig. 15) reported by two studies. The prevalence of multidrug resistance E. coli was 83% (95% CI 76–91%, I2 = 64.4%, p < 0.001, Fig. 16) as reported by 11 studies with a total sample size of 208 and 166 cases while, the prevalence of multidrug-resistant (MDR) Klebsiella species was 78% (95% CI 66–90%, I2 = 00.00%, p = 0.99, Fig. 17).
Antibiotic resistance patterns of Staphylococcal species
This review showed that S. aureus exhibited the highest resistance to ampicillin, 84% (95% CI 75–93%) followed by penicillin, 82% (95% CI 70–93%), tetracycline, 62% (95% CI 40–88%), amoxicillin–clavulanic acid, 54% (95% CI 10–98%), sulfamethoxazole–trimethoprim, 53% (95% CI 36–70%), and erythromycin, 50% (95% CI 27–73%) as shown in Table 5. Relatively lower rates of resistance were observed to nitrofurantoin, 16% (95% CI 4–49%), ciprofloxacin, 21% (95% CI −98%), clindamycin, 22% (95% CI 11–33%), chloramphenicol, 32% (95% CI 22–42%), and ceftriaxone, 34% (95% CI 18–50%). Similarly, the highest resistance by coagulase-negative Staphylococci was observed to penicillin with a prevalence of 87% (95% CI 79–94%) while, the lowest rate of resistance was to nitrofurantoin with a prevalence of 8% (95% CI 0–15%) as depicted in Fig. 18. The prevalence of multidrug resistance isolated S. aureus was 89% (95% CI 83–96%, I2 = 00.00%, p = 0.75, Fig. 19) while, it was 78% (95% CI 67–88%, I2 = 46.20%, p = 0.05, Fig. 20) for coagulase-negative Staphylococci.
Publication bias
The asymmetry of funnel plots visual inspection showed that there are some evidence of publication biases in the pooled estimates, which were statistically confirmed by Egger’s regression test (β = 8.30, 95% CI 4.30–12.30, p < 0.001, Supplementary 11) and after adjusting for publication bias by trim and fill analysis the funnel plot appeared symmetrical (Supplementary 12).
Discussion
The most prevalent bacterial infection in pregnancy is urinary tract infection (UTI), which increases the risk of maternal and newborn morbidity and mortality [51]. Bacteriuria causes a significantly larger number of neonates with low birth weight, premature delivery, and a higher neonatal mortality rate when it occurs during pregnancy [52]. Thus, this meta-analysis was aimed to determine the burden of bacteriuria among symptomatic and asymptomatic pregnant women, the common bacterial etiologies, and their susceptibility patterns.
In this meta-analysis of 20 studies, 15% of the pregnant women attending the antenatal care follow at different regions of Ethiopia had significant bacteriuria. Our finding showed a slightly higher number of bacteria identified compared to a review study from other low-income countries, where 13.5% of UTI-causing bacterial uropathogens were isolated from the urine sample [14]. In contrast to our meta-analysis, this review included a larger sample size (24,248 vs. 5536 urine specimens), however, the prevalence estimate did not contain the rigorous statistical analysis including the sub-group analysis. However, from a multicentre study of Tanzania, a slightly higher prevalence of significant bacteriuria among pregnant women was reported (17.7%); compared to our finding [19]. In different studies, Greve et al. [53], Lee et al. [54] and Prifti et al. [55], lower findings were reported, where the urine culture positivity (bacteriuria) among 8807, 4034, and 2149 pregnant women were 5.6%, 8.9%, and 13.31%, respectively. Compared with the rest of the world especially the developed countries, the prevalence of bacteriuria among pregnant women in Ethiopia were high. These could be associated with the different modifiable and preventable prenatal factors. These will include anemia, decreased immunity, sexual activity, early age marriage, lower socioeconomic classes, multiparity and gestational age [56,57,58,59,60].
Untreated asymptomatic bacteriuria in pregnancy leads, in as much as 40%, to the development of acute pyelonephritis with all the subsequent negative effects not only for the woman herself but particularly for the foetus [52]. This meta-analytic result indicated 12% of the pregnant women with significant bacteriuria were reported to be asymptomatic. A similar meta-analytic result from Iran indicated 13% of pregnant women had asymptomatic bacteriuria [61]. However, our finding is higher compared to a study by Lee et al. (Bangladesh), where 4.5% of the pregnant women with UTI had asymptomatic bacteriuria [54] and lower compared to a study by Mwambete and Malaba [62] from Tanzania, Dar es Salaam where 23.3% of the pregnant women attending the antenatal care had an asymptomatic urinary tract infection.
In this meta-analysis, Gram-negative bacteria accounted for 64% of culture-positive urine samples. Similarly, a review article from the low-income countries by Belete and Saravanan [14], and a study by Johnson et al. reported Gram-negative bacteria were the most common [63]. Regarding the specific bacteria identified, E. coli represented 41% of all the bacteria isolated from 20 studies. Several studies were reported E. coli was the most frequent bacteria isolated from the urine culture of pregnant women [19, 53,54,55, 63,64,65]. Staphylococcus species were the second frequent uropathogenic bacteria identified after E. coli. A similar finding was reported from the community cohort of pregnant women from Bangladesh that staphylococcal species were the second commonest bacterial isolates after E. coli [54]. However, a cross-sectional study from Cameroon reported, the Staphylococcal species (45%) were the most frequent bacterial isolates from pregnant women [66]. In contrast, Johnson et al. reported Klebsiella species (37.41%) was the most frequently identified bacteria than E. coli (28.78%) [63]. The difference might be related to the small sample size of the two studies.
Antibiotic resistance has led to significant challenges in treating UTI [67]. In this meta-analysis, E. coli was highly resistant to amoxicillin (81%) and ampicillin (80%). Similarly, Forson et al. from Ghana reported E. coli was 79.3% resistant to ampicillin [68]. However, higher resistance of E. coli to ampicillin (94.5%) and cotrimoxazole (88.8%) was reported in a multicentre study by Seni et al. compared to our findings. In contrast, in our meta-analysis, lower (40%) of the E. coli isolates were resistant to cotrimoxazole [19]. Our findings indicated lower resistance of E. coli to the following antibiotics were reported: nitrofurantoin (19%), ceftriaxone (20%), and ciprofloxacin (21%). Similar findings were reported by Seni et al., 12.8%, 13.4%, and 16.5%, respectively [19]. Similarly, in a meta-analysis by Emami et al., E. coli was 22% resistant to nitrofurantoin [18]. Our findings showed that 83% of the E. coli isolates were MDR and 19% were ESBL producers. Similar findings were reported in another meta-analysis by Mansouri et al. [17] and a study by Sekikubo et al. [20], where 17 and 18% of the E. coli strains identified from pregnant women with UTIs were ESBL producers, respectively.
The second frequent Gram-negative isolate in our meta-analysis was Klebsiella spp. (9%) from the 20 studies. Similar to E. coli, Klebsiella spp. were highly resistant to ampicillin (76%). This finding was relatively lower than a study by Seni et al. [19], where about 98% of the Klebsiella spp. were resistant to ampicillin. However, lower resistance of Klebsiella (21.8%) to ceftriaxone was reported, which is comparable to our finding (20%). Our finding indicated, the pooled prevalence of MDR Klebsiella spp. was 78% and 33% of the isolates were ESBL producers. Kaduma et al. reported a lower value; 15.4% of the Klebsiella spp. were ESBL producers [69]. The difference might be due to the lower number of participants in a study by Kaduma et al.
In this meta-analysis, Staphylococcus spp. isolates were highly resistant to the beta-lactam antibiotics. S. aureus was 84% and 82% resistant to ampicillin and penicillin, respectively. And, low resistance to both nitrofurantoin (16%) and ciprofloxacin (21%) identified. A similar resistance profile was noted with coagulase-negative Staphylococcus. Similar findings, but a slightly higher percentage of resistance of S. aureus to beta-lactam antibiotics was reported by Johnson et al.; ampicillin (90.1%), amoxicillin (93.9%), and amoxicillin/clavulanic acid (78.8%). Similar to our findings, lower resistance to nitrofurantoin (18.2%) and ciprofloxacin (33.3%) was reported [63].
In addition, this meta-analysis result showed the prevalence of multidrug resistance isolated S. aureus from urine samples of pregnant women with significant bacteriuria was 89%. Similarly, a study from Nigeria reported S. aureus isolated from urine samples of pregnant women was 90.0% each, and 85% resistant to cotrimoxazole, tetracycline, cefoxitin, and vancomycin, respectively [70]. Another study by Asmat et al. [71] also reported all the S. aureus isolates were multidrug-resistant; resistant to tetracycline, doxycycline, tobramycin, and intermediately resistant to pipemidic acid. However, a study by Asmat et al. had included a small number of pregnant women.
Strengths and limitations
The main strength of this meta-analysis is that it was the first to be reported from Ethiopia. In addition, it pooled a relatively large number of articles, which could improve the power and the precision of the estimates of the effect sizes. While the study findings led to the conclusion of high antibiotic resistance in pregnant women with UTI, the original studies included in the analyses came from only six of the country’s nine regions and two cities. As a result, the results’ applicability to the rest of the country may be questioned. In this meta-analysis, there is also significant publication bias, which is graphically assessed using funnel plots and statistically checked for the presence of a small study effect using the Egger test, affecting the interpretation of the findings. However, the pooled prevalence was corrected by Duval and Tweedie’s trim and fill analysis (the same as the original result, 15%). Furthermore, the reader should be aware that the protocol for this study was not made public, which could lead to bias.
Conclusion
The result of current review revealed the occurrence of substantial bacteriuria among pregnant women in the country. Resistance among common bacteria (E. coli, Klebsiella species, Staphylococcus species) causing UTIs in pregnant women is widespread to commonly used antibiotics. The high rate of bacteriuria among pregnant women in the country is an alert for clinicians to screen bacteriuria at least once using urine culture during antenatal care and treat if urine culture turn around positive. The high rate of drug resistance in turn warrant the need for regular epidemiological surveillance of antibiotic resistance and implementation of an efficient infection control and stewardship program.
Availability of data and materials
All relevant data are within the manuscript and its Supporting Information files.
References
Flores-Mireles AL et al (2015) Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 13(5):269–284
Foxman B (2014) Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin 28(1):1–13
Magliano E et al (2012) Gender and age-dependent etiology of community-acquired urinary tract infections. Sci World J 2012:1–7
Mazor-Dray E et al (2009) Maternal urinary tract infection: is it independently associated with adverse pregnancy outcome? J Matern Fetal Neonatal Med 22(2):124–128
Schnarr J, Smaill F (2008) Asymptomatic bacteriuria and symptomatic urinary tract infections in pregnancy. Eur J Clin Investig 38:50–57
Nicolle LE et al (2019) Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis 68(10):e83–e110
Kazemier BM et al (2015) Maternal and neonatal consequences of treated and untreated asymptomatic bacteriuria in pregnancy: a prospective cohort study with an embedded randomised controlled trial. Lancet Infect Dis 15(11):1324–1333
Smaill FM (2019) Vazquez JC (2019) Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev 11:1–52
Angelescu K et al (2016) Benefits and harms of screening for and treatment of asymptomatic bacteriuria in pregnancy: a systematic review. BMC Pregnancy Childbirth 16(1):1–10
Forland M (1991) Urinary tract infections, 2nd edn. In: Therapy of renal diseases and related disorders, chap 3. Kluwer Academic Publishers, pp 349–362
Gilstrap LC III, Ramin SM (2001) Urinary tract infections during pregnancy. Obstet Gynecol Clin N Am 28(3):581–591
Colgan R et al (2006) Asymptomatic bacteriuria in adults. Am Fam Physician 74(6):985–990
Azami M et al (2019) The etiology and prevalence of urinary tract infection and asymptomatic bacteriuria in pregnant women in Iran: a systematic review and meta-analysis. BMC Urol 19(1):1–15
Belete MA, Saravanan M (2020) A systematic review on drug resistant urinary tract infection among pregnant women in developing countries in Africa and Asia; 2005–2016. Infect Drug Resist 13:1465
Aslam B et al (2018) Antibiotic resistance: a rundown of a global crisis. Infect Drug Resist 11:1645
Chand KS, Kapoor P (2020) Two case reports of integrated management of antibiotic-resistant urinary tract infection. Homeopathy 109(02):097–106
Mansouri F et al (2019) Extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae and urinary tract infections in pregnant/postpartum women: a systematic review and meta-analysis. Int J Clin Pract 73(12):e13422
Emami A, Javanmardi F, Pirbonyeh N (2020) Antibiotic resistant profile of asymptomatic bacteriuria in pregnant women: a systematic review and meta-analysis. Expert Rev Anti Infect Ther 18(8):807–815
Seni J et al (2019) Multicentre evaluation of significant bacteriuria among pregnant women in the cascade of referral healthcare system in North-Western Tanzania: bacterial pathogens, antimicrobial resistance profiles and predictors. J Glob Antimicrob Resist 17:173–179
Sekikubo M et al (2017) Antibiotic overconsumption in pregnant women with urinary tract symptoms in Uganda. Clin Infect Dis 65(4):544–550
Alemu A et al (2012) Bacterial profile and drug susceptibility pattern of urinary tract infection in pregnant women at University of Gondar Teaching Hospital, Northwest Ethiopia. BMC Res Notes 5(1):1–7
Belete MA (2020) Bacterial profile and ESBL screening of urinary tract infection among asymptomatic and symptomatic pregnant women attending antenatal care of northeastern Ethiopia region. Infect Drug Resist 13:2579
Bizuwork K et al (2020) Asymptomatic bacteriuria among pregnant women in Addis Ababa, Ethiopia: prevalence, causal agents, and their antimicrobial susceptibility. Int J Microbiol. https://doi.org/10.1155/2021/8418043
Demilie T et al (2012) Urinary bacterial profile and antibiotic susceptibility pattern among pregnant women in North West Ethiopia. Ethiop J Health Sci 22(2):121–128
Ferede G et al (2012) The prevalence and antimicrobial susceptibility pattern of bacterial uropathogens isolated from pregnant women. Eur J Exp Biol 2(5):1497–1502
Gebremariam G et al (2019) Bacteriological profile, risk factors and antimicrobial susceptibility patterns of symptomatic urinary tract infection among students of Mekelle University, northern Ethiopia. BMC Infect Dis 19(1):1–11
Gessese YA et al (2017) Urinary pathogenic bacterial profile, antibiogram of isolates and associated risk factors among pregnant women in Ambo town, Central Ethiopia: a cross-sectional study. Antimicrob Resist Infect Control 6(1):1–10
Kumalo A, Tadesse M (2020) Asymptomatic bacteriuria and their antimicrobial susceptibility pattern among pregnant women attending antenatal clinics at Mizan Aman town, Southwestern Ethiopia. Eur J Clin Biomed Sci 6(4):56–62
Negussie A, Worku G, Beyene E (2018) Bacterial identification and drug susceptibility pattern of urinary tract infection in pregnant women at Karamara Hospital Jigjiga, Eastern Ethiopia. Afr J Bacteriol Res 10(2):15–22
Nisha AK, Etana AE, Tesso H (2015) Prevalence of asymptomatic bacteriuria during pregnancy in Adama city, Ethiopia. Int J Microbiol Immunol Res 3(5):58–63
Ali IE et al (2018) Asymptomatic bacteriuria and antimicrobial susceptibility pattern of the isolates among pregnant women attending Dessie Referral Hospital, Northeast Ethiopia: a hospital-based cross-sectional study. Turk J Urol 44(3):251
Assefa A et al (2008) Bacterial profile and drug susceptibility pattern of urinary tract infection in pregnant women at Tikur Anbessa Specialized Hospital Addis Ababa, Ethiopia. Ethiop Med J 46(3):227–235
Biset S et al (2020) Multi-drug resistant and extended-spectrum β-lactamases producing bacterial uropathogens among pregnant women in Northwest Ethiopia. Ann Clin Microbiol Antimicrob 19:1–9
Derese B et al (2016) Bacterial profile of urinary tract infection and antimicrobial susceptibility pattern among pregnant women attending at Antenatal Clinic in Dil Chora Referral Hospital, Dire Dawa, Eastern Ethiopia. Ther Clin Risk Manag 12:251
Edae M et al (2020) Asymptomatic bacteriuria among pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia: magnitude, associated factors, and antimicrobial susceptibility pattern. Int J Microbiol 2020:1–8
Tadesse E et al (2014) Asymptomatic urinary tract infection among pregnant women attending the antenatal clinic of Hawassa Referral Hospital, Southern Ethiopia. BMC Res Notes 7(1):1–5
Tadesse S et al (2018) Prevalence, antimicrobial susceptibility profile and predictors of asymptomatic bacteriuria among pregnant women in Adigrat General Hospital, Northern Ethiopia. BMC Res Notes 11(1):1–6
Tsegay E (2014) Bacterial profile and drug susceptibility pattern of urinary tract infection in pregnant women attending antenatal care at Mekelle Hospital, Mekelle, Northern Ethiopia. Addis Ababa University, Addis Ababa
Tula A et al (2020) Bacterial profile and antibiotic susceptibility pattern of urinary tract infection among pregnant women attending antenatal care at a Tertiary Care Hospital in Southern Ethiopia. Can J Infect Dis Med Microbiol. https://doi.org/10.1155/2020/5321276
Wabe YA et al (2020) Prevalence of asymptomatic bacteriuria, associated factors and antimicrobial susceptibility profile of bacteria among pregnant women attending Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Ther Clin Risk Manag 16:923
Moola S et al (2015) Conducting systematic reviews of association (etiology): the Joanna Briggs Institute’s approach. JBI Evid Implement 13(3):163–169
Moher D et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1–9
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Zeamanuel T et al (2009) Bacteriology of surgical site and catheter related urinary tract infections among patients admitted in Mekelle Hospital, Mekelle, Tigray, Ethiopia. Ethiop Med J 47(2):117–127
Endalafer N (2008) Bacterial nosocomial infections and their antimicrobial susceptibility patterns in surgical wards and surgical intensive care unit of Tikur Anbessa University Hospital. Addis Ababa University, Addis Ababa
Tekie K (2008) Surgical wound infection in Tikur Anbessa Hospital with special emphasis on Pseudomonas aeruginosa. Unpublished MSc thesis in medical microbiology, Addis Ababa University, Medical Faculty, Ethiopia. http://etd.aau.edu.et/bitstream/handle/123456789/5772/Kassaye%20Tekie.pdf. Accessed 31 Jan 2014.
Ayalew S (2014) Bacterial profile and drug resistance pattern of pathogens isolated from wound infection at Armed Force Referral and Teaching Hospital, Addis Ababa, Ethiopia. Addis Ababa University, Addis Ababa
Abdurrahman Ali KD (2017) Incidence of surgical site infection, predisposing factors and associated costs at Dessie Referral Hospital, Dessie, Ethiopia (unpublished article)
Sewunet T et al (2013) Bacterial profile and antimicrobial susceptibility pattern of isolates among burn patients at Yekatit 12 Hospital burn center, Addis Ababa, Ethiopia. Ethiop J Health Sci 23(3):209–216
Amare B et al (2011) Postoperative surgical site bacterial infections and drug susceptibility patterns at Gondar University Teaching Hospital, Northwest Ethiopia. J Bacteriol Parasitol 2(8):126
Kalinderi K et al (2018) Urinary tract infection during pregnancy: current concepts on a common multifaceted problem. J Obstet Gynaecol 38(4):448–453
Kladenský J (2012) Urinary tract infections in pregnancy: when to treat, how to treat, and what to treat with. Ceska Gynekol 77(2):167–171
Greve VH, Greve T, Helmig RB (2020) Bacteriuria in pregnancy in a Danish contemporary cohort of women. Infect Dis Obstet Gynecol. https://doi.org/10.1155/2020/8398537
Lee AC et al (2020) Urinary tract infections in pregnancy in a rural population of Bangladesh: population-based prevalence, risk factors, etiology, and antibiotic resistance. BMC Pregnancy Childbirth 20(1):1–11
Prifti E et al (2014) Urinary tract infections in pregnant women: Uropathogens and antimicrobial resistance profiles. Int J Infect Dis 21:359
Emiru T et al (2013) Associated risk factors of urinary tract infection among pregnant women at Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia. BMC Res Notes 6(1):1–6
Nguefack CT et al (2019) Clinical presentation, risk factors and pathogens involved in bacteriuria of pregnant women attending antenatal clinic of 3 hospitals in a developing country: a cross sectional analytic study. BMC Pregnancy Childbirth 19(1):1–6
Awolude OA et al (2010) Asymptomatic bacteriuria among HIV positive pregnant women. Virulence 1(3):130–133
Asrie F (2017) Prevalence of anemia and its associated factors among pregnant women receiving antenatal care at Aymiba Health Center, northwest Ethiopia. J Blood Med 8:35
Okia CC et al (2019) Prevalence, morphological classification, and factors associated with anemia among pregnant women accessing antenatal clinic at Itojo Hospital, south western Uganda. J Blood Med 10:351
Ghafari M et al (2016) The prevalence of asymptomatic bacteriuria in Iranian pregnant women: a systematic review and meta-analysis. PLoS ONE 11(6):e0158031
Mwambete K, Malaba P (2017) High prevalence of antibiotic resistance among bacteria isolated from pregnant women with asymptomatic urinary tract infections in Dar es Salaam, Tanzania. Res J Health Sci 5(2):65–73
Johnson B et al (2021) Prevalence and bacteriology of culture-positive urinary tract infection among pregnant women with suspected urinary tract infection at Mbarara Regional Referral Hospital, South-Western Uganda. BMC Pregnancy Childbirth 21(1):1–9
Naghi P et al (2019) A retrospective study in etiology of urinary tract infections in pregnant women in county Emergency Clinical Hospital-Obstetrics and Gynecology Clinic Oradea, Romania. Clin Chim Acta 493:S261–S262
Simon-Oke I, Odeyemi O, Afolabi O (2019) Incidence of urinary tract infections and antimicrobial susceptibility pattern among pregnant women in Akure, Nigeria. Sci Afr 6:e00151
Ndmason LM, Marbou WJ, Kuete V (2019) Urinary tract infections, bacterial resistance and immunological status: a cross sectional study in pregnant and non-pregnant women at Mbouda Ad-Lucem Hospital. Afr Health Sci 19(1):1525–1535
Waller TA et al (2018) Urinary tract infection antibiotic resistance in the United States. Prim Care Clin Off Pract 45(3):455–466
Forson AO et al (2018) Escherichia coli bacteriuria in pregnant women in Ghana: antibiotic resistance pattern, virulence factors and resistant genetic markers. BMC Res Notes 11:901
Kaduma J et al (2019) Urinary tract infections and preeclampsia among pregnant women attending two hospitals in Mwanza City, Tanzania: a 1:2 matched case–control study. BioMed Res Int. https://doi.org/10.1155/2019/3937812
Onanuga A, Omeje MC, Eboh DD (2018) Carriage of multi-drug resistant urobacteria by asymptomatic pregnant women in Yenagoa, Bayelsa State, Nigeria. Afr J Infect Dis 12(2):14–20
Asmat U, Mumtaz MZ, Malik A (2021) Rising prevalence of multidrug-resistant uropathogenic bacteria from urinary tract infections in pregnant women. J Taibah Univ Med Sci 16(1):102–111
Acknowledgements
Not applicable.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
LCK and TM conducted the database search, screening, quality assessment, and data analysis. KF and TMU wrote and revised the manuscript for the intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chelkeba, L., Fanta, K., Mulugeta, T. et al. Bacterial profile and antimicrobial resistance patterns of common bacteria among pregnant women with bacteriuria in Ethiopia: a systematic review and meta-analysis. Arch Gynecol Obstet 306, 663–686 (2022). https://doi.org/10.1007/s00404-021-06365-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06365-4