Abstract
Atopic dermatitis (AD) is an inflammatory, chronically relapsing, pruritic skin disease and lesions associated with AD are frequently colonized with Staphylococcus aureus (S. aureus). Activation of T cells by staphylococcal enterotoxins (SE) plays a crucial role in the pathogenesis of AD. Previous studies have demonstrated that lidocaine could attenuate allergen-induced T cell proliferation and cytokine production in peripheral blood mononuclear cells (PBMCs) from asthma patients. The purpose of this study was to investigate the effects of lidocaine on SE-stimulated activation of PBMCs from AD patients. PBMCs were isolated from ten AD patients and stimulated by staphylococcal enterotoxin A (SEA) or staphylococcal enterotoxin B (SEB) in the presence or absence of lidocaine in various concentrations. Cellular proliferation and the release of representative TH1- and TH2-type cytokines were measured. The effect of lidocaine on filaggrin (FLG) expression in HaCaT cells co-cultured with SE-activated PBMCs was also examined. Our results demonstrated that lidocaine dose-dependently inhibited the proliferative response and the release of IL-4, IL-5, IL-13, TNF-α, and IFN-γ from SEA- and SEB-stimulated PBMCs and also blocked the down-regulation of FLG expression in HaCaT cells co-cultured with SEA- and SEB-activated PBMCs. These results indicate that lidocaine inhibited SEA- and SEB-stimulated activation of PBMCs from patients with AD. Our findings encourage the use of lidocaine in the treatment of AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skin lesions associated with atopic dermatitis (AD) are frequently colonized by Staphylococcus aureus (S. aureus) [23], which secrete two kinds of major staphylococcal enterotoxins A (SE), staphylococcal enterotoxin (SEA) and staphylococcal enterotoxin B (SEB), that are characteristic of staphylococcal superantigens (SsAgs) and bind to major histocompatibility complex class II molecules and selectively activate T cells expressing certain T cell receptor (TCR) Vβ-chain families. Therefore, SEA and SEB can precipitate or aggravate cutaneous inflammation in AD by induction of T cell proliferation and cytokine secretion [32, 43]. Reportedly, SEB-stimulated peripheral blood mononuclear cells (PBMCs) from AD patients and increased TH2 cytokine production were compared with healthy controls [19]. The TH2 cytokine milieu in AD is now thought to play a significant role in the destruction of skin barrier function [13]. In addition to superantigen activity, SsAgs also have been shown to induce inflammation and exacerbate disease activity by production of superantigen-specific IgE in patients with AD [37]. There have been various reports correlating disease activity in AD with superantigen production and with specific levels of anti-superantigen IgE [24, 26, 27]. Furthermore, SsAgs can inhibit the suppressive ability of regulatory T cells [3]. Thus, SsAg-induced T cell proliferation and subsequent cytokine production can be considered as a target in the management of AD.
AD is a chronic and relapsing T cell-mediated inflammatory skin disorder [8], which is likely driven by epidermal barrier dysfunction of the damaged skin and impaired host immune responses [42]. Filaggrin (FLG) is essential for the epidermal barrier formation and integrity and FLG gene mutations are the most recognized causes of skin barrier dysfunction and are considered as predisposing factors to AD [6]. Reportedly, tumor necrosis factor alpha (TNF-α), interleukin (IL)-4, and IL-13 are overexpressed in AD lesions and significantly down-regulate calcium-induced FLG expression in epidermal keratinocytes (KCs), which may contribute to skin barrier abnormalities [1, 13, 18]. Thus, skin barrier repair by blocking production of inflammatory cytokines that down-regulate FLG expression suggests a probable treatment strategy for AD.
Lidocaine is often clinically used as a short-acting local anesthetic and antiarrhythmic agent [40], as it possesses anti-inflammatory effects, and can be used as an immunomodulatory drug in treatment against allergic diseases [12, 29], as nebulized lidocaine was shown to be an effective and safe therapy in patients with mild-to-moderate asthma [14, 20, 39]. Recent studies have also demonstrated that lidocaine and its analogue JMF2-1 inhibited the activation of T lymphocytes and generation of important cytokines [17, 21, 30].
In the present study, we examined the effects of lidocaine on SEA- and SEB-stimulated cell proliferation and cytokine production in PBMCs from AD patients. Furthermore, the effect of lidocaine on FLG expression in HaCaT cells, a well-known immortalized human keratinocyte cell line, co-cultured with SE-activated PBMCs, was also examined.
Materials and methods
Materials
The following reagents were used: hydrochloride lidocaine (Sigma-Aldrich, St. Louis, MO, USA); SEA and SEB (Toxin Technology, Inc., Sarasota, FL, USA); cell lysis buffer for western blotting and immunoprecipitation (IP) analysis, phenylmethanesulfonyl fluoride (PMSF) and sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) sample loading buffer (5×) (Beyotime Institute of Biotechnology, Beijing, China); Dulbecco’s modified Eagle’s medium (DMEM)-high glucose, fetal calf serum (FCS), serum-free keratinocyte medium for culture of human KCs and Dispase II (GIBCO-BRL, Gland Island, NY, USA). If not otherwise stated, the reagents were obtained from Sigma-Aldrich Chemie GmbH (Deisenhofen, Germany).
Subjects
Patient consent and ethical approval were obtained prior to the study. A total of ten AD patients (four males and six females; mean age, 27.75 years), who were admitted to our hospital, were included in the present study (Table 1). AD was diagnosed in accordance with the criteria of Hanifin and Rajka. The severity of disease was evaluated using the SCORing Atopic Dermatitis (SCORAD) index [34], which categorizes cases as mild (0–24 points), moderate (25–50 points) and severe (51–103 points). Venous blood samples were collected from AD patients and analyzed for total serum IgE level using a Pharmacia UniCAP-100 automatic immunoassay analyzer (Pharmacia Diagnostics AB, Uppsala, Sweden). None of the AD patients were currently administered with systemic steroids or immunosuppressant treatments, or utilizing potent topical steroids. This study was approved by the Ethics Committee of Shanghai Jiaotong University School of Medicine (Shanghai, China).
PBMC purification
PBMCs were isolated from heparinized venous blood from AD patients on Ficoll-Hypaque gradients (Pharmacia, Uppsala, Sweden) and resuspended in Roswell Park Memorial Institute (RPMI) 1,640 medium supplemented with gentamicin (40 μg/mL) and 10 % pooled type AB normal human serum (Sigma-Aldrich). In all experiments, cells were cultured under the atmosphere containing 5 % CO2 at 37 °C.
Analysis of lidocaine cytotoxicity on PBMCs
PBMCs (1 × 105 cells/well) were cultured for up to 7 days in the presence or absence of lidocaine. Cell viability was determined using the Cell Counting Kit-8 (CCK-8) assay kit (Beyotime Institute of Biotechnology) according to the manufacturer’s instructions.
Cellular proliferation and cytokine production analysis
Freshly isolated PBMCs (1 × 105 cells/well) were cultured with SEA (100 ng/mL) and SEB (100 ng/mL) in the presence of different concentrations of lidocaine in 96-well plates for 7 days. Cells were pulsed with 1 μ Ci of tritiated methyl thymidine (Radiochemical Center, Amersham, UK) for the last 8 h of the culture period. The stimulation index was calculated by dividing the counts per million allergen-stimulated cultures by that of unstimulated cultures. For cytokine production analysis, PBMCs (1 × 106 cells) were cultured with or without SEA (100 ng/mL) or SEB (100 ng/mL) for 72 h in the presence of different lidocaine concentrations. The levels of IL-4, IL-5, IL-13, IL-10, IL-12, IL-2, interferon gamma (IFN-γ), and TNF-α in the supernatant were measured with enzyme-linked immunosorbent assay (ELISA) kits (BioSource International, Inc., Camarillo, CA, USA).
Co-culture experiment
HaCaT cells were grown in DMEM supplemented with 10 % FCS, 1 % penicillin–streptomycin, and differentiated in high CaCl2 (10 mM) to up-regulate FLG expression for 48 h at 37 °C and 5 % CO2, as previously described [13]. A co-culture system was established by culturing HaCaT cells and PBMCs using a polycarbonated trans-well insert membrane containing 0.4 μm pores (Becton-Dickinson & Company, Franklin Lakes, NJ, USA). Briefly, HaCaT cells (1 × 105 cells/mL) were cultured at the bottom of 12-well plates, whereas PBMCs (2 × 106 cells/mL) were cultured on the polycarbonated insert membranes. In the co-culture system, cells were cultured for 48 h in RPMI 1,640 medium supplemented with gentamicin (40 μg/mL) and 10 % pooled type AB normal human serum. The cells were then washed with phosphate-buffered saline and further incubated with serum-free medium for 24 h before stimulation. SEA and SEB were then added to the PBMCs alone or with lidocaine and cultured for an additional 72 h. As a control, HaCaT cells were cultured in 12-well plates with membrane inserts, but without PBMCs.
RNA isolation and analysis
Total RNA was extracted from cells after treatment according to the experimental requirement. RNA extraction was performed using RNeasy Mini Kits (Qiagen, Valencia, CA, USA) according to the manufacturer’s guidelines. Total RNA (1 μg) was reverse-transcribed using the iScript cDNA Synthesis Kit (Bio-Rad, Hercules, CA, USA) at 25 °C for 5 min and 42 °C for 30 min, followed by 85 °C for 5 min in a final reaction volume of 40 μL. All assays were carried out under the following conditions: 35 cycles of denaturation at 95 °C for 15 s, followed by annealing and extension at 60 °C for 60 s using the ABI7300 Real Time PCR System (Applied Biosystems, Inc., Foster City, CA, USA). Melt curve analysis was performed to confirm the specificity of the amplified products. All samples were run in triplicate and relative expression was determined by normalizing samples to β-actin. Data were analyzed using the comparative ΔΔCt method. Primers and probes for human FLG and β-actin were purchased from Applied Biosystems.
Western Blot analysis
For Western Blot analysis, protein extracts (30 μg) were prepared by lysing the cells in lysis buffer containing protease and phosphatase inhibitors, separated by SDS-PAGE, and transferred to polyvinylidene difluoride membranes. Membranes were blocked for 2 h in TBS [50 mM Tris–HCl (pH 7.5) and 150 mM NaCl] containing 0.1 % Tween 20 and 5 % non-fat dried milk. Mouse anti-human β-actin antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) and mouse anti-human FLG antibody (Vector Laboratories, Inc., Burlingame, CA, USA) were used for western blotting. Subsequently, the membranes were incubated for 1 h with goat anti-mouse immunoglobulin (IgG) conjugated to horseradish peroxidase, rewashed, and developed using ECLTM reagents (Amersham Pharmacia Biotech, Inc., Piscataway, NJ, USA) and exposed to film.
Statistical analysis
Results are presented as mean ± SEM. Significant differences between groups were examined using the Wilcoxon signed-rank test. A p value ≤0.05 was considered statistically significant.
Results
Cell viability
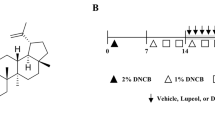
We initially investigated the cytotoxic effect of lidocaine on PBMCs from AD patients by culturing PBMCs in the presence or absence of different lidocaine concentrations for 7 days. Cell viability post-incubation was detected using the CCK-8 assay. We found that lidocaine at concentration up to 100 μmol/L did not affect PBMC viability, whereas concentrations at 1,000 μmol/L significantly decreased the percentage of viable cells (Fig. 1). Thus, subsequent experiments were performed with lidocaine concentrations ≤100 μmol/L.
Changes in PBMC viability after incubation with lidocaine. PBMCs from ten AD patients were cultured for up to 7 days in the presence or absence of lidocaine. The percentage of viable cells decreased significantly following exposure to 1,000 μmol/L of lidocaine (*p < 0.05, **p < 0.01, and ***p < 0.001 vs. untreated control)
Lidocaine inhibited SEA- and SEB-induced T cell proliferation
PBMCs from ten AD patients were stimulated by SEA, SEB, or phorbol myristate acetate (PMA) plus calcium ionophores in the presence or absence of lidocaine. Cellular proliferation was assessed by tritiated thymidine incorporation and expressed as stimulation index (SI). Our results demonstrated that lidocaine at 100 μmol/L significantly inhibited the proliferative response of PBMCs stimulated by SEA or SEB (p < 0.05, Fig. 2). We also found that lidocaine at 100 μmol/L inhibited PMA/calcium ionophore-stimulated proliferative responses, which was in agreement with a previous report [39].
Proliferative responses of PBMCs from ten AD patients after stimulation with SEA, SEB, or PMA plus calcium ionophore in the presence or absence of lidocaine. The stimulation index (SI) was calculated. Proliferative responses were significantly decreased with 100 μmol/L of lidocaine. (Comparisons were between the two treated groups and un-treated control; *p < 0.05 and **p < 0.01, respectively)
Lidocaine suppressed cytokine production in SEA- and SEB-stimulated PBMCs
Next, we tested the ability of lidocaine to reduce cytokine production in PBMCs from AD patients stimulated by SEA or SEB. Stimulation with SEA or SEB increased release of IL-4, IL-5, IL-13, TNF-α, IFN-γ, IL-2, IL-10, and IL-12 in PBMCs from AD patients, whereas lidocaine (100 μmol/L) significantly reduced IL-4, IL-5, IL-13, TNF-α, and IFN-γ production following SEA or SEB stimulation (p < 0.05, Figs. 3, 4). However, no similar inhibitory effects of lidocaine on IL-2, IL-10, and IL-12 production were observed (Figs. 3, 4).
IL-4, IL-5, IL-13, TNF-α, IFN-γ, IL-2, IL-10, and IL-12 production by PBMCs from ten AD patients after SEA stimulation in the presence or absence of lidocaine measured via ELISA. Lidocaine (100 μmol/L) significantly decreased SEA-induced IL-4, IL-5, IL-13, TNF-α, and IFN-γ production in PBMCs from AD patients. (Comparisons were between the two treated groups and nontreated control, respectively, *p < 0.05, **p < 0.01, and ***p < 0.001 vs. untreated control)
IL-4, IL-5, IL-13, TNF-α, IFN-γ, IL-2, IL-10, and IL-12 production by PBMCs from ten AD patients after stimulation with SEB in the presence or absence of lidocaine measured via ELISA. Lidocaine (100 μmol/L) significantly decreased SEB-induced IL-4, IL-5, IL-13, TNF-α, and IFN-γ production in PBMCs from AD patients. (Comparisons were between the two treated groups and nontreated control, respectively, *p < 0.05, **p < 0.01, and ***p < 0.001)
Lidocaine blocked the down-regulation of FLG expression in HaCaT cells co-cultured with SEA- and SEB-activated PBMCs
Next, we further investigated the effect of lidocaine on FLG expression in HaCaT cells co-cultured with SEA- and SEB-activated PBMCs and found that FLG mRNA levels in HaCaT cells co-cultured with activated PBMCs were significantly lower than those in HaCaT cells cultured alone. In the co-culture system, the addition of lidocaine (100 μmol/L) to PBMCs blocked the down-regulation of FLG expression, both at the mRNA (Fig. 5a) and protein levels (Fig. 5b, c), following induction by SEA- and SEB-activated PBMCs.
The effects of lidocaine on FLG expression in HaCaT cells were studied in a trans-well co-culture system. PBMCs from ten AD patients were seeded on the surface of insert membrane and HaCaT cells were seeded on the bottom of the plate. FLG expression was analyzed using real-time RT-PCR and western blotting. Lidocaine significantly inhibited FLG down-regulation in HaCaT cells co-cultured with PBMCs in the presence of SEA and SEB at both the mRNA (a) and proteins (b) levels. c Densitometric analysis of the western blotting results is shown, in which the intensity of the protein signal normalized against the β-actin signal. (Comparisons were between the two treated groups and nontreated control, respectively, *p < 0.05 and **p < 0.01)
Discussion
To the best of our knowledge, the present study is the first to demonstrate lidocaine inhibition of PBMC proliferation in response to SEA and SEB stimulation. In addition, the production of both TH1-type cytokines (TNF-α and IFN-γ) and TH2-type cytokines (IL-4, IL-5, and IL-13) from SEA and SEB-activated PBMCs was inhibited by lidocaine at a concentration of 100 μmol/L. These new findings indicate that lidocaine may exert immunoregulatory effects on immune cells and can be used as an anti-inflammatory agent in the treatment of AD.
The skin lesions present in AD are frequently colonized with S. aureus strains that produce SsAgs [23, 43] and recent evidence has indicated that one type of skin-homing T cell (CD4 +/Foxp3 +) in AD patients exerts effector TH2-like functions promoting SsAg stimulation, which may aggravate allergic skin inflammation [25]. SsAgs also have the ability to augment antigen-specific TH1 responses by stimulating antigen-presenting cells, which might contribute to AD chronification [2], and can contribute to AD pathogenesis by increasing the frequency of memory T cells that are able to migrate to and be activated within AD lesions, where they directly contact epidermal KCs [38]. Several cytokines, including TNF-α, IL-4, and IL-13, are released from T cells and monocytes and were found to down-regulate FLG expression in KCs [13, 18], thus contributing to compromised skin barrier function.
Staphylococcus aureus can colonize AD skin and simultaneously secrete SEA and SEB, which can subsequently induce the release of TNF-α, IL-4, and IL-13 from immune cells that, in turn, can down-regulate FLG expression in KCs. Thus, we evaluated the inhibitory effect of lidocaine on activated PBMCs via measuring FLG expression in HaCaTs and PBMCs in a co-culture system in which PBMCs were stimulated with SEA and SEB together to mimic an in vivo environment. Our results showed that lidocaine significantly blocked FLG down-regulation in HaCaT cells co-cultured with SEA and SEB-stimulated PBMCs. We ascribe this effect of lidocaine to its inhibition of cytokine production (i.e., TNF-α, IL-4, and IL-13) in activated PBMCs, suggesting that lidocaine may exert an inhibitory effect on inflammatory T cells activated by SE, which, in turn, provide beneficial effects to skin barrier repair.
Glucocorticosteroids are commonly used drugs for AD treatment, although corticosteroid treatment has been challenged for its adverse effects on the skin barrier. Topical corticosteroid application can delay epidermal barrier restoration, lead to epidermal thinning, and even induce a strong reduction in human beta-defensin production [16, 31, 36]. In this context, lidocaine, with its inhibitory effect on PBMCs and potential to improve skin barrier function, may be used as a novel treatment against AD. Nevertheless, the use of lidocaine–prilocaine cream (a eutectic mixture of local anesthetics) in pediatric and dermatologic practice to obtain local anesthesia, can also cause many skin side effects, which include transient skin blanching, erythema, urticaria, allergic contact dermatitis, irritant, contact dermatitis, hyperpigmentation, and purpura [4, 7, 10, 28, 33]. Thus, further studies on animals or patients are still needed and the safety of lidocaine for the treatment of AD should be evaluated as well.
Previous studies have demonstrated that lidocaine can relax smooth airway muscles by decreasing intracellular Ca2+ concentrations [15]. Activation of Ca2+, K+, and Cl− channels is important for activation of T-cells in the early phase of an immune reaction [35, 41]. Elevation of Ca2+ plays a critical role in the activation and translocation of nuclear transcription factors, including nuclear factor (NF) AT, NF-κB, and c-Jun N-terminal kinase (also known as mitogen-activated protein kinase 8) [5, 11]. Moreover, recent studies have reported that lidocaine attenuates lipopolysaccharide-induced acute lung injury and inhibits epithelial chemokine secretion through inhibition of NF-κB activation [9, 22], thus, inhibition of cytokine production and T cell proliferation by lidocaine is likely related to its down-regulation of NF-κB signaling [21]. Therefore, the inhibitory effects of lidocaine on SEA- and SEB-induced PBMC proliferation and cytokine production may occur through the inhibition of the NF-κB pathway; however, the precise underlying molecular mechanism(s) require further exploration.
In conclusion, herein, we demonstrated the inhibitory effects of lidocaine against SEA- and SEB-stimulated activation of PBMCs from AD patients. Therefore, lidocaine is a promising anti-inflammatory agent in the treatment of AD.
References
Bieber T (2008) Atopic dermatitis. N Engl J Med 358(14):1483–1494
Bright JJ, Xin Z, Sriram S (1999) Superantigens augment antigen-specific Th1 responses by inducing IL-12 production in macrophages. J Leukoc Biol 65(5):665–670
Cardona ID, Goleva E, Ou LS, Leung DY (2006) Staphylococcal enterotoxin B inhibits regulatory T-cells by inducing glucocorticoid-induced TNF receptor-related protein ligand on monocytes. J Allergy Clin Immunol 117(3):688–695
Clarkson A, Choonara I, O’Donnell K (1999) Localized adverse skin reactions to topical anesthetics. Pediatr Anesth 9(6):553–555
Clipstone NA, Crabtree GR (1992) Identification of calcineurin as a key signaling enzyme in T-lymphocyte activation. Nature 357(6380):695–697
Cork MJ, Danby SG, Vasilopoulos Y, Hadgraft J, Lane ME, Moustafa M, Guy RH, Macgowan AL, Tazi-Ahnini R, Ward SJ (2009) Epidermal barrier dysfunction in atopic dermatitis. J Invest Dermatol 129(8):1892–1908
de Waard-van der Spek FB, Oranje AP (1997) Purpura caused by Emla is of toxic origin. Contact Dermat 36(1):11–13
Eichenfield LF, Ellis CN, Mancini AJ, Paller AS, Simpson EL (2012) Atopic dermatitis: epidemiology and pathogenesis update. Semin Cutan Med Surg 31(3 Suppl):S3–S5
Feng G, Liu S, Wang GL, Liu GJ (2008) Lidocaine attenuates lipopolysaccharide-induced acute lung injury through inhibiting NF-kappaB activation. Pharmacology 81(1):32–40
Godwin Y, Brotherston M (2001) Hyperpigmentation following the use of Emla cream. Br J Plast Surg 54(1):82–83
Hivroz-Burgaud C, Clipstone NA, Cantrell DA (1991) Signaling requirements for the expression of the transactivating factor NF-AT in human T lymphocytes. Eur J Immunol 21(11):2811–2819
Hollmann MW, Durieux ME (2000) Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology 93(3):858–875
Howell MD, Kim BE, Gao P, Grant AV, Boguniewicz M, Debenedetto A, Schneider L, Beck LA, Barnes KC, Leung DY (2007) Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol 120(1):150–155
Hunt LW, Frigas E, Butterfield JH, Kita H, Blomgren J, Dunnette SL, Offord KP, Gleich GJ (2004) Treatment of asthma with nebulized lidocaine: a randomized, placebo-controlled study. J Allergy Clin Immunol 113(5):853–859
Kai T, Nishimura J, Kobayashi S, Takahashi S, Yoshitake J, Kanaide H (1993) Effects of lidocaine on intracellular Ca2+ and tension in airway smooth muscle. Anesthesiology 78(5):954–965
Kao JS, Fluhr JW, Man MQ, Fowler AJ, Hachem JP, Crumrine D, Ahn SK, Brown BE, Elias PM, Feingold KR (2003) Short-term glucocorticoid treatment compromises both permeability barrier homeostasis and stratum corneum integrity: inhibition of epidermal lipid synthesis accounts for functional abnormalities. J Invest Dermatol 120(3):456–464
Kawasaki T, Kawasaki C, Sata T, Chaudry IH (2011) Lidocaine suppresses mouse Peyer’s Patch T cell functions and induces bacterial translocation. Surgery 149(1):106–113
Kim BE, Howell MD, Guttman-Yassky E, Gilleaudeau PM, Cardinale IR, Boguniewicz M, Krueger JG, Leung DY (2011) TNF-alpha down-regulates filaggrin and loricrin through c-Jun N-terminal kinase: role for TNF-alpha antagonists to improve skin barrier. J Invest Dermatol 131(6):1272–1279
Konig B, Neuber K, Konig W (1995) Responsiveness of peripheral blood mononuclear cells from normal and atopic donors to microbial superantigens. Int Arch Allergy Immunol 106(2):124–133
Kubo A, Nagao K, Amagai M (2012) Epidermal barrier dysfunction and cutaneous sensitization in atopic diseases. J Clin Invest 122(2):440–447
Lahat A, Ben-Horin S, Lang A, Fudim E, Picard O, Chowers Y (2008) Lidocaine down-regulates nuclear factor-kappaB signaling and inhibits cytokine production and T cell proliferation. Clin Exp Immunol 152(2):320–327
Lang A, Ben Horin S, Picard O, Fudim E, Amariglio N, Chowers Y (2010) Lidocaine inhibits epithelial chemokine secretion via inhibition of nuclear factor kappa B activation. Immunobiology 215(4):304–313
Leung DY, Boguniewicz M, Howell MD, Nomura I, Hamid QA (2004) New insights into atopic dermatitis. J Clin Invest 113(5):651–657
Lin YT, Shau WY, Wang LF, Yang YH, Hwang YW, Tsai MJ, Tsao PN, Chiang BL (2000) Comparison of serum specific IgE antibodies to staphylococcal enterotoxins between atopic children with and without atopic dermatitis. Allergy 55(7):641–646
Lin YT, Wang CT, Chao PS, Lee JH, Wang LC, Yu HH, Yang YH, Chiang BL (2011) Skin-homing CD4+ Foxp3+ T cells exert Th2-like function after staphylococcal superantigen stimulation in atopic dermatitis patients. Clin Exp Allergy 41(4):516–525
Na SY, Roh JY, Kim JM, Tamang MD, Lee JR (2012) Analysis of colonization and genotyping of the exotoxins of Staphylococcus aureus in patients with atopic dermatitis. Ann Dermatol 24(4):413–419
Nada HA, Gomaa NI, Elakhras A, Wasfy R, Baker RA (2012) Skin colonization by superantigen-producing Staphylococcus aureus in Egyptian patients with atopic dermatitis and its relation to disease severity and serum interleukin-4 level. Int J Infect Dis 16(1):e29–e33
Neri I, Savoia F, Guareschi E, Medri M, Patrizi A (2005) Purpura after application of EMLA cream in two children. Pediatr Dermatol 22(6):566–568
Ohnishi T, Kita H, Mayeno AN, Okada S, Sur S, Broide DH, Gleich GJ (1996) Lidocaine in bronchoalveolar lavage fluid (BALF) is an inhibitor of eosinophil-active cytokines. Clin Exp Immunol 104(2):325–331
Olsen PC, Ferreira TP, Serra MF, Farias-Filho FA, Fonseca BP, Viola JP, Cordeiro RS, Silva PM, Costa JC, Martins MA (2011) Lidocaine-derivative JMF2-1 prevents ovalbumin-induced airway inflammation by regulating the function and survival of T cells. Clin Exp Allergy 41(2):250–259
Park KY, Kim DH, Jeong MS, Li K, Seo SJ (2010) Changes of antimicrobial peptides and transepidermal water loss after topical application of tacrolimus and ceramide-dominant emollient in patients with atopic dermatitis. J Korean Med Sci 25(5):766–771
Pinchuk IV, Beswick EJ, Reyes VE (2010) Staphylococcal enterotoxins. Toxins (Basel) 2(8):2177–2197
Roldan-Marin R, de-la-Barreda Becerril F (2009) Petechial and purpuric eruption induced by lidocaine/prilocaine cream: a rare side effect. J Drugs Dermatol 8(3):287–288
(1993) Severity scoring of atopic dermatitis: the SCORAD index. Consensus report of the European task force on atopic dermatitis. Dermatology 186(1):23–31
Shapiro DN, Adams BS, Niederhuber JE (1985) Antigen-specific T cell activation results in an increase in cytoplasmic free calcium. J Immunol 135(4):2256–2261
Sheu HM, Lee JY, Chai CY, Kuo KW (1997) Depletion of stratum corneum intercellular lipid lamellae and barrier function abnormalities after long-term topical corticosteroids. Br J Dermatol 136(6):884–890
Sonesson A, Bartosik J, Christiansen J, Roscher I, Nilsson F, Schmidtchen A, Back O (2012) Sensitization to skin-associated microorganisms in adult patients with atopic dermatitis is of importance for disease severity. Acta Derm Venereol
Strickland I, Hauk PJ, Trumble AE, Picker LJ, Leung DY (1999) Evidence for superantigen involvement in skin homing of T cells in atopic dermatitis. J Invest Dermatol 112(2):249–253
Tanaka A, Minoguchi K, Oda N, Yokoe T, Matsuo H, Okada S, Tasaki T, Adachi M (2002) Inhibitory effect of lidocaine on T cells from patients with allergic asthma. J Allergy Clin Immunol 109(3):485–490
Tetzlaff JE (2000) The pharmacology of local anesthetics. Anesth Clin N Am 18(2):217–233
Wacholtz MC, Cragoe EJ Jr, Lipsky PE (1992) A Na(+)-dependent Ca2+ exchanger generates the sustained increase in intracellular Ca2+ required for T-cell activation. J Immunol 149(6):1912–1920
Wolf R, Wolf D (2012) Abnormal epidermal barrier in the pathogenesis of atopic dermatitis. Clin Dermatol 30(3):329–334
Wollenberg A, Rawer HC, Schauber J (2011) Innate immunity in atopic dermatitis. Clin Rev Allergy Immunol 41(3):272–281
Acknowledgments
This study was supported by grants from the Science and Technology Commission of Shanghai Municipality (11JC1408400 and 12411951600), the National Nature Science Foundation of China (81171544), the Shanghai Municipal Health Bureau (2009065), the Shanghai Jiaotong University School of Medicine (BXJ 201122) and a foundation of Shanghai Jiaotong University School of Medicine (11XJ21020).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Jiao, Q., Wang, H., Hu, Z. et al. Lidocaine inhibits staphylococcal enterotoxin-stimulated activation of peripheral blood mononuclear cells from patients with atopic dermatitis. Arch Dermatol Res 305, 629–636 (2013). https://doi.org/10.1007/s00403-013-1339-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-013-1339-4