Abstract
Introduction
The importance of the assembly procedure on the taper connection strength is evident. However, existent surgical technique guides frequently lack comprehensive and precise instructions in this regard. The aim of our experimental study was to evaluate the influence of the surgical technique guide on the femoral head assembly procedure in surgeons with differing levels of experience in total hip arthroplasty.
Materials and methods
Twenty-eight participants, divided into four groups based on their lifetime experience in total hip arthroplasty, conducted a femoral head assembly procedure in a simulated intraoperative environment before and after reviewing the surgical technique guide. Demographic information and the number of hammer blows were documented. Hammer velocity and impaction angle were recorded using an optical motion capturing system, while the impaction force was measured using a dynamic force sensor within the impactor.
Results
We observed a high variation in the number of hammer blows, maximum force, and impaction angle. Overall, the number of hammer blows decreased significantly from 3 to 2.2 after reviewing the surgical technique guide. The only significant intragroup difference in the number of hammer blows was observed in the group with no prior experience in total hip arthroplasty. No correlation was found between individual factors (age, weight, height) or experience and the measured parameters (velocity, maximum force and angle).
Conclusions
The present study demonstrated a high variation in the parameters of the femoral head assembly procedure. Consideration of the surgical technique guide was found to be a limited factor among participants with varying levels of experience in total hip arthroplasty. These findings underline the importance of sufficient preoperative training, to standardize the assembly procedure, including impaction force, angle, and use of instruments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of modularity at the head-neck junction in primary total hip arthroplasty (THA) offers surgeons the flexibility to adjust size and offset of the femoral head, neck and stem to the anatomy of the patient. However, modularity provides the femoral component with an additional interface, which is a potential source of wear and corrosion.
Taper wear and corrosion involve a complex interplay of many factors that mostly depend on implant design and surgical technique. Retrieval studies indicate that more rigid trunnions and tapers with a smaller taper angle are less susceptible to corrosion and fretting [1,2,3,4]. In recent decades there has been a trend towards smaller trunnions as they have the inherent advantage of a bigger head-neck-ratio with an increased impingement-free range of motion. Despite their clinical advantages, smaller trunnions are less rigid and may result in a higher risk of taper corrosion [2].
The underlying process of significant tribocorrosion in the junction between the metallic stem taper and the femoral head is referred to as mechanically assisted crevice corrosion (MACC) and can result in the release of metal corrosion products into the joint fluid. These particles and metal ions can lead to an adverse local tissue reaction (ALTR) with osteolysis and cytotoxic effects (necrosis) in the surrounding bone stock and soft tissues [5, 6]. While this problem is well known in metal-on-metal bearings, studies showed a prevalence of MACC from 1.1 to 3.2% in metal-on-polyethylene bearings for total hip arthroplasties [7, 8], which are still a common bearing in total hip arthroplasty up to date [9, 10]. A recent clinical study showed a revision rate of 11.6% for MACC with metal-on-polyethylene bearing with a mean time to revision of 6.6 years [11]. Although ALTR is less common with ceramic femoral heads, there are some reports about ALTR with ceramic-on-polyethylene and ceramic-on-ceramic bearings [12,13,14]. In addition to the design of the total hip implant, there is increasing evidence that the assembly procedure of modular components plays a crucial role for taper stability and thus for fretting and corrosion of modular hip endoprostheses [15,16,17]. Reduced wear in the taper-head junction with increasing assembly forces was reported [18, 19].
Experimental studies advised an assembly of the femoral head with a force of at least 4 kN with one hammer blow with the femoral head placed on a clean, dry taper [20,21,22]. However, preclinical studies face challenges in simulating the intraoperative setting during the femoral head assembly and often neglect the influence of the human factor.
Although the method for femoral head impaction is described and illustrated in the surgical technique guide, information differs about the number of hammer blows, impaction force, and impaction angle depending on the used implant [23]. Therefore, the purpose of our experimental study was to evaluate the effect of the surgical technique guide on variables of the femoral head assembly procedure (number of hammer blows, hammer velocity, maximum impaction force and impaction angle) of participants with different experience in THA.
Materials and methods
Experimental test rig
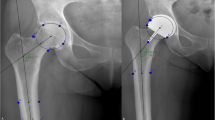
An experimental test rig to simulate intraoperative conditions during a femoral head assembly procedure was developed (Fig. 1). A cementless stem (LCU, Size 11, 12/14 taper, Ti6Al4V4, Waldemar Link GmbH & Co. KG, Hamburg, Germany) was embedded in a polyurethane casting (Rencast FC 52 Isocyanate / FC 52 Polyol, Huntsman Advanced Materials; Salt Lake City, UT, USA) in an iron alloy pipe (made of X6CrNiMoTi17-12-2) that acted as a spring to simulate the elastic behaviour of a leg. The pipe had an analytically calculated stiffness of 275 N/mm in the longitudinal taper axis, which was in agreement to spring stiffness in previous studies [24]. We fixed the pipe to an aluminium profile construction (item Industrietechnik GmbH, Solingen, Germany) which was mounted on a wooden base. To simulate a patient lying in supine position with an antero-lateral hip approach on the left side we connected an artificial leg to the stem and covered the test rig with large surgical drapes (Fig. 1). For the impaction trials a BIOLOX®delta ceramic head with a diameter of 36 mm (CeramTec GmbH, Plochingen, Germany) was placed on the taper.
Hammer and impactor
We used a commercially available impaction hammer (mass = 758 g, Waldemar Link GmbH & Co. KG, Hamburg, Germany) with two impaction sides: stainless steel or polyamide (PA12). For our trials we used only the stainless-steel impaction side of the hammer. We also used a commercially available impactor consisting of a stainless-steel impact area and a PA12 tip (mass = 416 g, Waldemar Link GmbH & Co. KG, Hamburg, Germany). We modified the shaft of the impactor to mount a force sensor along the shaft axis (Fig. 2). This was realized by sawing the shaft into two at its centre and turning threads into the single shaft parts to fix the sensor.
Force measurement
The force measurement was performed with a dynamic force sensor (Model M201A76, PCB Piezotronics, Depew, USA) with a capacity of 22 kN, which was supplied with energy by a piezotron coupler (Type 5134B, Kistler Instrumente GmbH, Sindelfingen, Germany). The output voltage of the piezotron coupler was sampled with 100 kHz and 16 bit by an analog to digital converter (Model USB 6216, National Instruments, Austin, TX, USA) resulting in a resolution of 0.73 N.
Additionally, the force sensor was manually calibrated before the tests. This was performed using a static testing machine (Model Z50, ZwickRoell GmbH & Co. KG, Ulm, Germany) equipped with a 50 kN load cell (GTM Testing and Metrology GmbH, Bickenbach, Germany) by means of static loading (duration > 120 s) and as fast as possible relieving (duration < 1 s). The force amplitude shown at the relieving process was evaluated as the measured force of the sensor. This process was performed at multiple force values (500–5,000 N). The coefficient of determination of the correction curve was > 0.9999.
Before calibration and testing, an initial compression pre-load of at least 4.5 kN was applied to the force sensor according to the instructions given by the manufacturer. The analysis of the force data was performed with LabView Version 13 (National Instruments, Austin, TX, USA). The absolute force was evaluated by subtracting the signal before impact from the signal peak caused by the impact. The error range for the force measurements was ± 10%.
Angle and velocity measurement
The angle and velocity were recorded with an infrared optical tracking system (Model MCU200, LUKOtronic, Innsbruck, Austria), with the corresponding software. Three infrared markers were used (upper impactor, lower impactor, and hammer) which were sampled at 240 Hz. The impaction angle measurement was performed by calculating the linear curve between the two infrared markers mounted at the impactor (Fig. 2). Before starting the tests, the zero angle was determined by positioning the impactor on a socket that was connected to the femoral stem equal to the taper axis. The angle that was measured during the tests was the solid angle in relation to the zero angle. The error range for the angle measurement was ± 3°.
For the velocity measurement, the coordinate of the hammer marker was captured. This marker was positioned in a way that captured the absolute velocity of the hammer head without axial rotation. A software computed function was used to differentiate the velocity data from the motion data.
Trajectories, velocity, and force data were collected and evaluated with a script using MATLAB 2018a (MathWorks, Natick, MA, USA). In this script the absolute velocity of the hammer-marker, equivalent to the velocity of the hammer head, was calculated based on the assumption, that the hammer releases the entire kinetic energy (at some point the velocity equals zero) at the end of the impaction. The angles were calculated for every hammer blow at the time point when the velocity was at the maximum. The error range for the velocity measurement was ± 5%.
Impaction trials
A total of 28 participants, consisting of 17 orthopaedic surgeons with different experience in THA and 11 non-surgeons took part in the study. We divided the participants into four study groups according to their lifetime experience in THA. Group 1 had no experience in THA, Group 2 performed 1–10 THA, Group 3 performed 11–100 THA and Group 4 performed > 100 THA during their career. We documented the age, height, and weight of the participants. The experimental setup was split into two sections. In the first section, the participants were asked to hit the femoral head according to their experience or, for the unexperienced participants, according to their idea how to hit the femoral head, respectively. The impactor, that was placed on the femoral head was hit with the metal side of the hammer. The participants had three attempts to perform the assembly procedure. In the second section, the participants were provided with the available surgical technique guide of the THA implant system for the assembly procedure with following instructions: “Clean and dry the taper of the stem thoroughly. This is particularly important with ceramic heads. Mount the head by hand using axial pressure and a turning motion. Impact the head lightly if necessary, using the impactor for prosthesis heads”. After reading the surgical technique guide, the assembly procedure was carried out again according to the first part of the experimental setup. The femoral head was disassembled before each attempt and was placed on the taper by the participants. To optimise the position of the subject during the assembly procedure, we offered a step stool to account for different body heights.
Statistics
The differences between the four groups for maximum force, hammer velocity, impaction angle and variance were evaluated with Kruskal-Wallis test and Dunn´s as the post hoc test. Non-parametric tests were chosen as analysis with Shapiro-Wilk test revealed that the data were not normally distributed. Maximum force, hammer velocity, impaction angle and variance and overall differences within a group before and after reading the surgical technique guide were compared statistically using Wilcoxon test for a paired, non-parametric analysis. Correlations between maximum force, impaction angle, hammer velocity, height, weight, age, and group were calculated using the Spearman rank test. Cut-off for positive or negative correlation was rs< -0.5 or rs> 0.5.
The analysis was performed using Graph Pad Prism 8 (GraphPad Software, San Diego, CA, USA) with a significance level of 0.05. All results are reported as mean ± standard deviation (range).
Results
Twenty-eight participants with a mean age of 37.4 years ± 11.3 years (20 years – 68 years), a mean height of 178.2 cm ± 9.4 cm (155 – 198 cm) and a mean weight of 78.5 kg ± 16.9 kg (53 – 115 kg) participated in the study. All participants were right-handed. Detailed data for the single groups are presented in Table 1.
Number of hammer blows
A total of 438 hammer blows from 28 participants with 6 attempts each (3 attempts before and 3 attempts after reading the surgical technique guide) were recorded, 255 before and 183 after reading the surgical technique guide. The mean number of hammer blows before reading the surgical technique guide over all participants and attempts was 3.0 ± 1.7 (1–11), which decreased significantly to 2.2 ± 1.1 (1–5) after reading the surgical technique guide (p < 0.0001).
The average number of hammer blows per attempt for the four separate groups is shown in Table 2. Group 2 used significantly lower numbers of hammer blows on the femoral head for assembly than Group 3 before reading the surgical technique guide (p < 0.05). After reading the surgical technique guide there were no significant differences between the groups.
Within the groups there was a significant decrease in number of hammer blows in Group 1 after reading the surgical technique guide (p < 0.05). In Groups 2, 3 and 4 reading the surgical technique guide had no significant influence on the number of hammer blows.
Influence of surgical technique guide on hammer velocity, maximum force and impaction angle
The mean data for hammer velocity, maximum force and impaction angle are presented in Table 3.
Hammer velocity
The average hammer velocity calculated from all hammer blows was 2.544 ± 1.171 m/s (0.522 m/s – 4.844 m/s) before and 2.362 ± 1.503 m/s (0.577 m/s – 5.735 m/s) after reading the surgical technique guide without a significant change (p = 0.227).
Hammer velocity differed between Group 1 and Group 3 with lower hammer velocities recorded in Group 3. While before reading the surgical technique guide this was only a trend (p = 0.0558) the difference between the two groups reached significance after reading the surgical technique guide (p = 0.0225). In general, Group 3 showed a non-significant trend towards decreased velocity after reading the surgical technique guide (p = 0.0742) (Fig. 3).
Hammer velocity by Group before and after reading the surgical technique guide (STG). The hammer velocity of Group 3 was significantly lower than of Group 1 (* p = 0.0225) after reading the surgical technique guide (STG) and showed a similar trend (# p = 0.0558) before reading the surgical technique guide (STG). Comparison of intragroup difference showed a non-significant trend towards a decreasing hammer velocity in Group 3 after reading the surgical technique guide (STG) (+ p = 0.0742)
Maximum Force
The overall average maximum force before reading the surgical technique guide was 7,467 N ± 4,166 N (1,546 N – 20,269 N) and did not significantly change after reading the surgical technique guide with 6,551 N ± 4,821 N (1,128–22,828 N). There was no significant difference between the groups in the maximum applied force (Fig. 4). However, there was a non-significant trend towards a decreased maximum force in Group 3 (p = 0.0558) after reading the surgical technique guide.
Impaction angle
For all hammer blows the average impaction angle was 10.4° ± 7.5° (3.5° – 29.9°) before and 8.7° ± 6.9° (1.8° – 34.6°) after reading the surgical technique guide. There were no significant changes in impaction angle between the groups and no significant change after reading the surgical technique guide (Fig. 5).
Intergroup and intragroup variance in impaction parameters
The angle, at which the femoral head was hit, varied widely between participants with coefficients of variation (CV) of 36.8% ± 22.5% (4.9 – 77.8%) and 30.4% ± 21.9% (3.5 – 92.9%) before and after reading the surgical technique guide, respectively. While there was also a high variation for the applied force (CV before reading the surgical technique guide: 16.1% ± 10.23% (2.8 − 45.8%); CV after reading the surgical technique guide: 15.9% ± 9.1% (3.6 − 48.2%)), the velocity of the hammer was relatively homogenous (CV before reading the surgical technique guide: 11.1% ± 7.2% (1.8 − 31.8%); CV after reading the surgical technique guide: 8.4% ± 7.0% (1.5 − 27.2%)). There was no significant difference between variance of impaction angle, force, and hammer velocity before and after reading the surgical technique guide (Fig. 6). Also, no significant intergroup or intragroup differences were found in the coefficient of variance of impaction angle, maximum force, and hammer velocity.
Correlations
There was no correlation between experience in THA and number of hammer blows. In the personal data, there was a positive correlation between experience and age (p < 0.001, rs= 0.65) as well as between height and weight (p < 0.0001, rs=0.79). No correlations between personal data (age, height, weight) and measured variables (number of hammer blows, maximum force, hammer velocity, impaction angle) were observed. Hammer velocity and maximum impaction force showed a positive correlation before (p < 0.0001, rs=0.89) and after reading the surgical technique guide (p < 0.0001, rs=0.94). The impaction angle showed no correlation to any other measured variables.
Discussion
The aim of this study was to examine the impact of the surgical technique guide on the femoral head assembly procedure among participants with different levels of experience in THA. While the number of hammer blows was not explicitly stated, reading the surgical technique guide resulted in a significant overall decrease in the number of hammer blows used during the procedure. However, this effect was only significant in Group 1 (no experience in THA). Moreover, reading the surgical technique guide did not have any significant intragroup impact on the hammer speed, force, and angle during the assembly procedure. Additionally, it was observed that force and impaction angle exhibited a high variation among the participants. Overall, the consideration of the surgical technique guide demonstrated only a limited effect on the assembly procedure, highlighting the need for sufficient preoperative training and corresponding instruments to achieve standardized head assembly.
Number of hammer blows
The assembly procedure plays a pivotal role in establishing the initial stability of the taper connection to prevent excessive micromotion, which may lead to corrosion. Despite its fundamental importance in the assembly procedure, there is still no consensus about the proper surgical technique. The information provided by most surgical technique guides lacks specific information about the instruments that should be used for impaction and about the parameters of impaction (number of hammer blows, impaction force, impaction angle). The assembly procedure for the femoral head shows even conflicting recommendations across various surgical technique guides [23]. Recent preclinical studies give contradictory recommendations concerning the number of hammer blows during the femoral head assembly procedure. Rehmer et al. [20] and Pandorf et al. [25] advise a single hammer impact according to their finding that additional impactions did not increase the pull-off force. The same was confirmed by Pennock et al. [22] who reported that the first impaction accounted for 90% of the mechanical strength of the taper connection. In contrast, Heiney et al. [26] suggested to apply at least two hammer blows as they found a significant increase in pull-off force after the second, third or fourth blow in comparison to hitting the head once. In the present study the mean number of hammer blows before reading the surgical technique guide was three, which was in accordance to previous studies [27, 28]. Although, no exact number of hammer blows was specified in the surgical technique guide, the information provided resulted in a decrease of the overall number of blows. When analysing the intragroup difference, this was only significant in Group 1 (no experience in THA). The number of blows in Group 2–4 decreased after reading the surgical technique guide but did not reach significance. This could be due to the already lower numbers of blows in these groups before reading the surgical technique guide (maximum 5 blows in Group 2–4 compared to 11 in Group 1) as well as the limited number of participants. It is noteworthy, that there was no significant difference in number of blows between non-surgeons and surgeons before and after surgical technique guide.
Force
Numerous studies have demonstrated a positive correlation between the assembly force and the initial stability of the taper connection [20, 22, 29, 30]. In the current study, the utilized surgical technique guide recommended to “Mount the head by hand using axial pressure and a turning motion” and to “Impact the head lightly if necessary, using the impactor for prosthesis heads”. The terms “axial pressure” “turning motion” and “impact lightly” provide the user with a broad range of interpretations resulting in substantial variations in the assembly procedure among different surgeons. The strongest impaction force in the present study after reading the surgical technique guide (22,828 N) was 20-fold higher than the weakest impaction (1,128 N) which shows how differently the information given in the surgical technique guide regarding the femoral head assembly procedure is interpreted. The impaction forces for the femoral head assembly recorded in our study (1,128 N – 22,828 N) are consistent with forces in other studies that ranged between 273 N and 26,602 N [26, 27, 31, 32].
However, there was no significant intra- and intergroup difference in the maximum force before or after reading the surgical technique guide. These findings are in contrast to Brial et al. [28] who found a positive correlation between years in practice and the average maximum impaction force for attending surgeons. The recommended assembly force depends on head size and is indicated with 4,000 N to 6,000 N in trials that were carried out under laboratory conditions [20, 33]. This force range was met in our study by 22% of the applied impactions before and by 18% after reading the surgical technique guide. The rest of the impactions was below or above the indicated range. On the one hand there is a risk to produce an insufficient taper connection with the consequence of higher wear and corrosion rates as recent studies demonstrated for inferior assembly forces [18, 34]. On the other hand, excessive forces can cause damage to ceramic implant components and adjacent bone tissue [18, 35, 36].
The measured force depends on several conditions, like the location of force acquisition, the material of the hammer, impactor, and the compliance of the system. Lavernia et al. who reported the lowest average forces of 1,661 N ± 148 N, used a force transducer on which eight surgeons performed impactions with an impactor and a hammer [31]. Nassutt et al. [32] used an experimental setup with a force sensor placed under a CoCr taper on a socket with a rubber mat to simulate the intraoperative compliance. The reported minimal force of 273 N ± 24 N was approximately four times lower than our minimal force and corresponded to the maximal force that they reported for assembly of the head by a turning motion with the hand (204 N ± 21 N) [32]. Heiney et al. [26] reported mean impaction forces for attending orthopaedic surgeons to be 4,409 N ± 660 N and 4,346 N ± 939 N for resident orthopaedic surgeons using a pressure sensitive film without specifying the exact assembly conditions. Scholl et al. used a bench-top-model with a stem fixed in a sawbone femur and a force sensor located in the tip of a metal hammer. With this setup, which was similar to our setup, they reported impaction forces with a range from 3,597 N to 26,602 N [27]. However, a study examining the impaction force applied by surgeons conducted by Wendler et al. [37] with human cadavers and damping simulating human soft tissue showed considerably lower impaction forces (822.5 N to a maximum of 3835.2 N) than our study.
Impaction angle and hammer velocity
Factors, that have so far received little attention, are the impaction angle and hammer velocity. The hammer velocity showed a highly positive correlation with the maximum impaction force acting as an indicator for the impaction force.
Up to date there are only few investigations analysing the impaction angle [38] and there is no literature known to the authors that deals with the influence of the impaction angle on the taper connection strength. However, a study examining factors influencing the femoral head seating displacement could identify impaction angle and assembly force as the most significant factors for impaction assembly [39]. Studies carried out under laboratory conditions use a drop hammer that applies a reproducible axial force. Furthermore, the Standard Test Method for Determining the Axial Disassembly Force of Taper Connections of Modular Prostheses, stipulates a quasi-axial load application, “so that the line of load application is aligned with the axes of the male and female taper components within ± 1°” [40]. However, our results indicate that an axial force application is not usual under realistic conditions. Furthermore, in our study the angle showed the highest variance among the impaction parameters with no significant change after reading the surgical technique guide.
Clinical implications
The variation of assembly force and angle among surgeons with different experience in total hip arthroplasty in our study persisted, even after advice from the surgical technique guide was provided. The fact demonstrates that there is still a huge potential for a more standardized femoral head assembly process. From the various factors that can positively affect the stability of the taper connection, the impaction force was pointed out as the most important factor in a recent study [17]. The femoral head assembly process during surgery can be influenced by the surgeon. Proper assembly ensures an effective locking of the head-taper connection and reduces potential micromotion. While experimental setups like in this study provide surgeons with perfect conditions for the assembly, the situation in situ usually presents further hurdles for a standardized femoral head assembly. Depending on the anatomy of the patients, the surgical approach, and the design of the used instruments, the assembly process can be negatively influenced, resulting in an unfavourable angle and transduced force of the femoral head impaction. This means an insufficient interlocking of the head-taper connection can lead to MACC and ALTR [6]. With revision rates up to 11.6% for MACC in non-metal-on-metal bearings [11, 14], the problem of MACC is still one of the common severe complications in total hip arthroplasty. A femoral head assembly procedure with instruments that standardize impaction force and angle could be a potential key factor to reduce MACC and consecutive complications as ALTR.
Limitations
The results of the specific instrumentation system are not generally transferable to other surgical systems. Additionally, our developed test rig represents a more realistic but still artificial test system as no soft tissue that could distract the impactor was implemented. Furthermore, the resulting forces below the taper and disassembly forces or moments were not measured in the present study.
Conclusion
Consideration of the surgical technique guide had only limited influence on the femoral head assembly procedure of surgeons with varying levels of experience in total hip arthroplasty who participated in the present study. These findings underline the importance of sufficient preoperative training to standardize the assembly procedure, including impaction force, angle, and use of instruments. Otherwise, the fixation strength of the taper connection and consecutively the taper corrosion may vary. The data emphasize the need for precise personal instructions including the definition of the number of hammer blows, impaction force, impaction angle and impaction instruments. Moreover, our results indicate that laboratory test setups should represent more realistic conditions of the intraoperative assembly procedure of the femoral head.
References
Kao Y-YJ, Koch CN, Wright TM, Padgett DE (2016) Flexural Rigidity, Taper Angle, and contact length affect fretting of the femoral stem trunnion in total hip arthroplasty. J Arthroplasty 31:254–258. https://doi.org/10.1016/j.arth.2016.02.079
Porter DA, Urban RM, Jacobs JJ et al (2014) Modern trunnions are more flexible: a mechanical analysis of THA taper designs. Clin Orthop 472:3963–3970. https://doi.org/10.1007/s11999-014-3965-3
Higgs GB, Hanzlik JA, MacDonald DW et al (2013) Is increased modularity associated with increased fretting and corrosion damage in metal-on-metal total hip arthroplasty devices? A retrieval study. J Arthroplasty 28:2–6. https://doi.org/10.1016/j.arth.2013.05.040
Goldberg JR, Gilbert JL, Jacobs JJ et al (2002) A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop 149–161. https://doi.org/10.1097/00003086-200208000-00018
Urish KL, Giori NJ, Lemons JE et al (2019) Trunnion Corrosion in Total Hip Arthroplasty-Basic concepts. Orthop Clin North Am 50:281–288. https://doi.org/10.1016/j.ocl.2019.02.001
Hall DJ, Pourzal R, Jacobs JJ (2020) What surgeons need to know about adverse local tissue reaction in total hip arthroplasty. J Arthroplasty 35:S55–S59. https://doi.org/10.1016/j.arth.2020.01.016
Hussey DK, McGrory BJ (2017) Ten-year cross-sectional study of mechanically assisted crevice corrosion in 1352 consecutive patients with metal-on-polyethylene total hip arthroplasty. J Arthroplasty 32:2546–2551. https://doi.org/10.1016/j.arth.2017.03.020
McGrory BJ, MacKenzie J, Babikian G (2015) A high prevalence of corrosion at the Head-Neck taper with contemporary Zimmer non-cemented femoral Hip Components. J Arthroplasty 30:1265–1268. https://doi.org/10.1016/j.arth.2015.02.019
W-Dahl A, Kärrholm J, Rogmark C et al (2022) The Swedish Arthroplasty Register Annual Report 2022, https://doi.org/10.18158/ryr8eIN_i
Ben-Shlomo Y, Blom A, Boulton C et al (2022) The National Joint Registry 19th Annual Report 2022 [Internet]. London: National Joint Registry; 2022 Oct. PMID: 36516281
Wilson JM, Broggi MS, Oladeji P et al (2021) Outcomes following revision for mechanically assisted crevice corrosion in a single femoral design. J Arthroplasty 36:3966–3972. https://doi.org/10.1016/j.arth.2021.08.010
Banerjee S, Cherian JJ, Bono JV et al (2015) Gross trunnion failure after primary total hip arthroplasty. J Arthroplasty 30:641–648. https://doi.org/10.1016/j.arth.2014.11.023
Kusaba A, Katsui M, Hakuta N et al (2014) Catastrophic stem taper wear in ceramic on polyethylene bearing couple: a case report. J Long Term Eff Med Implants 24:185–188. https://doi.org/10.1615/jlongtermeffmedimplants.2014011133
Matharu GS, Pandit HG, Murray DW, Judge A (2016) Adverse reactions to metal debris occur with all types of hip replacement not just metal-on-metal hips: a retrospective observational study of 3340 revisions for adverse reactions to metal debris from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. BMC Musculoskelet Disord 17:495. https://doi.org/10.1186/s12891-016-1329-815
Jacobs JJ (2016) Corrosion at the Head-Neck Junction: why is this happening now? J Arthroplasty 31:1378–1380. https://doi.org/10.1016/j.arth.2016.03.029
Weiser MC, Lavernia CJ (2017) Trunnionosis in total hip arthroplasty. J Bone Joint Surg Am 99:1489–1501. https://doi.org/10.2106/JBJS.17.00345
Mueller U, Bormann T, Schroeder S, Kretzer J (2021) Taper junctions in modular hip joint replacements: what affects their stability? J Mech Behav Biomed Mater 116. https://doi.org/10.1016/j.jmbbm.2020.104258
English R, Ashkanfar A, Rothwell G (2016) The effect of different assembly loads on taper junction fretting wear in total hip replacements. Tribol Int 95:199–210. https://doi.org/10.1016/j.triboint.2015.11.025
Fallahnezhad K, Feyzi M, Hashemi R, Taylor M (2022) The role of the Assembly Force in the Tribocorrosion Behaviour of Hip Implant Head-Neck junctions: an adaptive finite element Approach. Bioeng Basel Switz 9:629. https://doi.org/10.3390/bioengineering911062920
Rehmer A, Bishop NE, Morlock MM (2012) Influence of assembly procedure and material combination on the strength of the taper connection at the head-neck junction of modular hip endoprostheses. Clin Biomech Bristol Avon 27:77–83. https://doi.org/10.1016/j.clinbiomech.2011.08.002
Krull A, Morlock MM, Bishop NE (2017) The influence of contamination and cleaning on the strength of modular head taper fixation in total hip arthroplasty. J Arthroplasty 32:3200–3205. https://doi.org/10.1016/j.arth.2017.05.009
Pennock AT, Schmidt AH, Bourgeault CA (2002) Morse-type tapers: factors that may influence taper strength during total hip arthroplasty. J Arthroplasty 17:773–778. https://doi.org/10.1054/arth.2002.33565
McGrory BJ, Ng E (2017) No Consensus for femoral head impaction technique in Surgeon Education materials from Orthopedic Implant manufacturers. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.12.036
Krull A, Morlock MM, Bishop NE (2018) Maximizing the fixation strength of modular components by impaction without tissue damage. Bone Jt Res 7:196–204. https://doi.org/10.1302/2046-3758.72.BJR-2017-0078.R2
Pandorf T, Preuss R, Czak R (2010) Impaction forces and proper seating of ceramic ball heads. In: 56th Annu. Meet. Orthop. Res. Soc. 2010. https://www.ors.org/transactions/56/2256.pdf. Accessed 29 Jul 2023
Heiney JP, Battula S, Vrabec GA et al (2009) Impact magnitudes applied by surgeons and their importance when applying the femoral head onto the Morse taper for total hip arthroplasty. Arch Orthop Trauma Surg 129:793–796. https://doi.org/10.1007/s00402-008-0660-4
Scholl L, Schmidig G, Faizan A et al (2016) Evaluation of surgical impaction technique and how it affects locking strength of the head-stem taper junction. Proc Inst Mech Eng [H] 230:661–667. https://doi.org/10.1177/0954411916644477
Brial C, Rancourt M-F, Wright T, Westrich G (2016) Femoral Head Impaction Force Varies with Surgeon Experience and is Dependent on Head Material for Surgeons in Training. In: 62th Annu. Meet. Orthop. Res. Soc. 2016. https://www.ors.org/transactions/62/1062.pdf. Accessed 29 Jul 2023
Mroczkowski ML, Hertzler JS, Humphrey SM et al (2006) Effect of impact assembly on the fretting corrosion of modular hip tapers. J Orthop Res off Publ Orthop Res Soc 24:271–279. https://doi.org/10.1002/jor.20048
Brial C, Koch CN, Wright TM, Westrich GH (2017) Do Taper Design and Impaction Load affect Micromotion and Pulloff Strength of the Head-Neck Junction in Total Hip Arthroplasty? In: 63th Annu. Meet. Orthop. Res. Soc. 2017. https://www.ors.org/transactions/63/1993.pdf. Accessed 29 Jul 2023
Lavernia CJ, Baerga L, Barrack RL et al (2009) The effects of blood and fat on Morse taper disassembly forces. Am J Orthop Belle Mead NJ 38:187–190
Nassutt R, Mollenhauer I, Klingbeil K et al (2006) [Relevance of the insertion force for the taper lock reliability of a hip stem and a ceramic femoral head]. Biomed Tech (Berl) 51:103–109. https://doi.org/10.1515/BMT.2006.018
MacLeod AR, Sullivan NPT, Whitehouse MR, Gill HS (2016) Large-diameter total hip arthroplasty modular heads require greater assembly forces for initial stability. Bone Jt Res 5:338–346. https://doi.org/10.1302/2046-3758.58.BJR-2016-0044.R1
Panagiotidou A, Cobb T, Meswania J et al (2018) Effect of impact assembly on the interface deformation and fretting corrosion of modular hip tapers: an in vitro study. J Orthop Res off Publ Orthop Res Soc 36:405–416. https://doi.org/10.1002/jor.23601
Weisse B, Affolter C, Stutz A et al (2008) Influence of contaminants in the stem-ball interface on the static fracture load of ceramic hip joint ball heads. Proc Inst Mech Eng [H] 222:829–835. https://doi.org/10.1243/09544119JEIM374
Schwarz E, Reinisch G, Brandauer A et al (2018) Load transfer and periprosthetic fractures after total hip arthoplasty: comparison of periprosthetic fractures of femora implanted with cementless distal-load or proximal-load femoral components and measurement of the femoral strain at the time of implantation. Clin Biomech Bristol Avon 54:137–142. https://doi.org/10.1016/j.clinbiomech.2018.03.010
Wendler T, Prietzel T, Möbius R et al (2021) Quantification of assembly forces during creation of head-neck taper junction considering soft tissue bearing: a biomechanical study. Arthroplasty 3:20. https://doi.org/10.1186/s42836-021-00075-7
Noble P, Foley E, Simpson J et al (2017) Inter-surgeon variability in the assembly of modular head-neck tapers in Tha via the posterior approach. Orthop Proc 99–B:59–59. https://doi.org/10.1302/1358-992X.99BSUPP_5.ISTA2016-059
Grostefon JD, Camino TS, Leisinger SR et al (2016) Femoral Head Displacement Comparing Impaction and Quasi-Static Assembly Methods. In: 62th Annu. Meet. Orthop. Res. Soc. 2016. https://www.ors.org/transactions/62/1125.pdf. Accessed 29 Jul 2023
Standard Test Method for Determining the Axial Disassembly Force of Taper Connections of Modular Prostheses https://www.astm.org/f2009-20.html. Accessed 29 Jul 2023
Acknowledgements
The authors would like to acknowledge Mr. Mario Jackszis and the Institute of Physics at the University of Rostock for supporting us at the construction of the impaction device and test rig.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The stem, hammer and impactor were provided by Waldemar Link GmbH & Co. KG, Hamburg, Germany. Waldemar Link GmbH & Co. KG, Hamburg, Germany, had no influence on study design, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Martin Darowski and Leo Ruehrmund. Data analysis and statistics were performed by Martin Darowski, Leo Ruehrmund and Annett Klinder. The first draft of the manuscript was written by Martin Darowski and Leo Ruehrmund and all authors commented on previous versions of the manuscript. All authors assessed the results and assure the accuracy of the data. All authors agree with the content in the submitted manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Financial interests
Authors Martin Darowski, Annett Klinder, Rainer Bader, and Leo Ruehrmund declare they have no financial interests. Author Daniel Kluess is CEO at INNOPROOF GmbH (Rostock, Germany, independent accredited testing lab for medical devices). Wolfram Mittelmeier has received fees for court expert opinions about implant failure and product liability from district courts (15 different courts) and will receive support for attending meetings and travel from the Japanese Orthopaedic Association (JOA).
Non-financial interests
Authors Martin Darowski, Daniel Kluess, Annett Klinder, Rainer Bader, and Leo Ruehrmund declare they have no non-financial interests. Author Wolfram Mittelmeier is a board member at the German Society for medical technical aids (DGIHV e.V.) and President of the AFOR Foundation (Association for Orthopaedic Research).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Darowski, M., Ruehrmund, L., Kluess, D. et al. The influence of surgical technique guidance and surgeon’s experience on the femoral head assembly in total hip arthroplasty. Arch Orthop Trauma Surg 144, 2391–2401 (2024). https://doi.org/10.1007/s00402-024-05282-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05282-w