Abstract
Introduction
The purpose was to compare the arthroscopic rod technique to stress ultrasound in the dynamic assessment of lateral elbow instabilities.
Materials and methods
Fifteen elbows of eight specimen with a mean age of 66.4 ± 13.3 years were assessed in a prone position following a defined dissection setup. After evaluation of the native status, an arthroscopic dissection of the radial collateral ligament (RCL) or lateral ulnar collateral ligament (LUCL), and finally of entire capsuloligamentous structures was performed. Three raters examined each state (native, RCL or LUCL lesion, complete lesion) with the arthroscopic rod technique in 90° flexion and with stress ultrasound in 30 and 90° flexion. The intra-class correlation coefficient (ICC) was calculated to assess the interrater reliability as well as test–retest reliability for each testing modality (arthroscopy and ultrasound).
Results
The arthroscopic rod technique showed a superior interrater and test–retest reliability of 0.953 and 0.959 (P < 0.001), respectively, when compared to stress ultrasound with an ICC of 0.4 and 0.611 (P < 0.001). A joint space opening during arthroscopy of > 6 mm humero-ulnar or > 7 mm humero-radial was indicative for a lateral collateral ligament lesion. However, a differentiation between an isolated RCL or LUCL tear was not possible. A lateral joint opening of ≥ 9 mm was only observed in complete tears of the lateral capsuloligamentous complex.
Conclusions
The arthroscopic rod technique showed a superior interrater and test–retest reliability when compared to stress ultrasound. Arthroscopic assessment for radial elbow instability was found to be reliable and reproducible. A joint gapping ≥ 9 mm in the arthroscopic evaluation is a sign for a complete insufficiency of the radial capsuloligamentous complex. However, it is not possible to precisely distinguish between a lesion of the RCL or LUCL by arthroscopy.
On the basis of our results, dynamic ultrasound testing may be inappropriate to objectify lateral elbow instability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With an incidence of 5.2 per 100.000, elbow dislocations are the second most common dislocations in the human body. In most cases, young adults, who are active in sports, are affected [1]. Despite the generally favorable long-term results after conservative therapy, chronic subtle joint instabilities can persist after a traumatic dislocation and may lead to pain, subjective instability or even movement restrictions in this young and active patient population [2,3,4,5,6]. Furthermore, apart from acute trauma, chronic elbow instabilities may also be the result of a chronic epicondylitis, repetitive corticosteroid injections and surgical approaches [2, 3, 7,8,9].
The precise identification of elbow instabilities in the chronic setting represents a great challenge, even for the experienced orthopedic surgeon. Especially in unsedated patients, the clinical evaluation of the elbow is infringed and the interpretation of an instability severity is not reliable [10]. This may result in overlooking ligamentous instability of the elbow [2, 3].
Multiple imaging modalities can be applied for the diagnosis of elbow instability [11]. Magnetic resonance imaging (MRI) has been established as gold standard for diagnosing soft tissue injuries of the elbow [12]. However, MRI remains a static examination of a dynamic problem and may be inappropriate to assess dynamic aspects of instability [13, 14].
Stress ultrasound is used by many clinicians to evaluate dynamic elbow stability and represents a fast as well as non-invasive modality with greater availability and high imaging resolution [12, 14,15,16].
The value of arthroscopy in the diagnosis as well as treatment of chronic elbow instability has recently increased [17,18,19].
As early as 1996, Field et al. [20] introduced a technique that used switching rods to evaluate elbow stability on the medial side in cadaveric specimen. Different rod sizes were used to objectively quantify the gapping of the medial compartment under valgus-stress. A complete release of the medial collateral ligament led to a significant medial joint opening of 4 to 10 mm. Later, the “elbow drive-through sign” was described by several authors during elbow arthroscopy [21,22,23]. Here, the complete insufficiency of the lateral collateral ligaments allows the surgeon to arthroscopically glide from the lateral compartment to the medial compartment.
In our experience, arthroscopic stability testing using a scaled switching rod is a valuable tool to assess elbow instabilities. To our knowledge, no standardized procedure has been described to arthroscopically objectify a lateral capsuloligamentous complex insufficiency. Furthermore, the arthroscopic assessment has not yet been compared to stress ultrasound as the second dynamic instability assessment modality.
The purpose of this study was to compare arthroscopic evaluation with scaled switching rods to stress ultrasound. It was hypothesized that the arthroscopic evaluation provides a more precise assessment with a higher reliability when compared to stress ultrasound.
Materials and methods
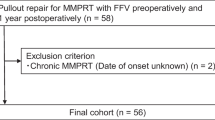
Eight male Specimen with a mean age of 66.4 ± 13.3 (range 48–83) years were assessed for elbow instability. Each specimen included paired elbows of a complete human torso provided by the pathologic institute of the University Hospital of Augsburg. Prior to testing, it was ensured that the specimen had no history of elbow surgery and an assessment with a mobile C-arm image intensifier was performed to exclude severe osteoarthritis. One elbow was excluded due to osteoarthritis, which resulted in seven right and eight left elbows that were finally assessed. This study was reviewed and approved by the ethical board of the University Hospital of Augsburg (IRB No. 2017-26).
Testing setup and arthroscopic dissection
Testing was performed with the specimen thawed to room temperature and free range of motion of the elbow joint. It was ensured that the range of motion was not infringed due to cadaveric rigidity. The cadaver was placed in prone position and the humerus was secured to a mount allowing the desired flexion angle of the elbow joint (Fig. 1).
Standardized portals orientated on anatomic landmarks were established in every specimen. A low posterolateral portal at the soft-spot between the radial epicondyle, the radial head and the tip of the olecranon was used for initial joint distension. Before instability testing, it was ensured that a thorough arthroscopy was possible and a complete resection of the posterolateral plica was performed.
After evaluation of the native status, selective arthroscopic dissection of the radial collateral ligament (RCL) or the lateral ulnar collateral ligament (LUCL), respectively, was performed. The order of RCL or LUCL dissection was determined by a simple randomization technique. Finally, the complete lateral ligamentous complex was cut and complete lateral instability was reached. The arthroscopic dissection was adapted from McAdams et al. [8] (Fig. 2a–c).
Arthroscopic view via a high posterolateral portal visualizing the posterolateral elbow compartment of a left elbow (RH radial head, LC lateral condyle). View on the intact lateral capsuloligamentous complex of the elbow (a), dissection of the capsule and ligaments with a hook electrode (b) and incised anterior capsuloligamentous structures of the elbow (c)
Each state: native (n = 15), RCL lesion (n = 7) or LUCL lesion (n = 8), and complete lateral ligamentous lesion (n = 15) was assessed with arthroscopy and ultrasound by three independent examiners to enable interrater reliability calculations. All examiners were orthopedic surgeons specialized in arthroscopic surgery. For test–retest reliability calculations, all measurements of the senior author (A.L.) were repeated at a later stage during testing.
Arthroscopic testing
Visualizing through a high posterolateral portal lateral to the tip of the olecranon stability testing was performed. The low posterolateral portal was used to enter the joint with rods of different sizes. The rods were gently inserted to avoid any damage to the cartilage beginning with a diameter of 1 mm and increasing in increments of 1 mm up to a maximum of 9 mm.
Humero-radial instability was assessed at the center of the radial head and humero-ulnar instability at the level of the incisura olecrani. The largest diameter that could be fitted into the joint space without excessive stress was recorded. (Fig. 3a–c) All stability measurements were performed with the elbow flexed at 90 degrees and at neutral forearm rotation.
Instability testing of a left native elbow for humero-radial stability at the center of the radial head (a) and for humero-ulnar stability at the level of the incisura olecrani (b) fitting a 4 mm switching rod. After dissection of the lateral collateral ligament a 9 mm rod fits at the level of the incisura olecrani (c). (RH radial head, LC lateral condyle, MC medial condyle, OL olecranon)
Ultrasound
In the ultrasonic evaluation (Mindray Z6, Mindray, Shenzhen, China), the transducer was aligned to the lateral epicondyle and the extensor tendons. The shortest distance between the rim of the radial head and the capitellum was documented. (Fig. 4a, b) All measurements were performed at 30 and 90° elbow flexion with neutral forearm rotation. The difference between the varus loaded vs. unloaded elbow was documented. It was ensured that the ultrasound probe maintained its orientation as well as position during the varus maneuver to avoid deviations in the plane of measurement.
Statistics
Statistical analysis was performed using SPSS software version 23 (SPSS Inc). Based on the observations of Field et al. [24], an a priori power analysis was performed. It was determined that a sample size of 15 would provide a power of 80% to detect a 2 mm difference between the native and the sectioned state at an alpha of 0.05.
The intra-class correlation coefficient (ICC) overall as well as for each dissection state was calculated to assess the interrater reliability as well as test–retest reliability for each testing modality (arthroscopy and ultrasound).
Absolute values for joint space opening were calculated for each dissection state and presented as means ± SDs and ranges.
Results
The successive dissection of the lateral ligamentous structures resulted in an increase in lateral instability in both testing modalities. Overall, arthroscopy showed a superior interrater and test–retest reliability of ICC 0.953 and 0.959 when compared to sonography with an ICC of 0.4 and 0.611, respectively. This observation was independent from the degree of lateral instability. (Table 1).
Despite the high interrater and test–retest reliability for the arthroscopic rod technique, we found a high inter-individual variance for lateral joint opening at an intact lateral ligament complex with a mean of 4 mm (range 2–6) for humero-ulnar and 3.7 mm (range 2–7) for humero-radial testing. A high inter-individual variance was also observed after sequential dissection of the lateral collateral ligament complex. (Table 2) However, a joint space opening of more than 6 mm humero-ulnar or more than 7 mm humero-radial was indicative for a lateral collateral ligament lesion. On the basis of our data, a differentiation between an isolated RCL or LUCL tear by absolute values was not possible.
A lateral joint opening of 9 mm or more at the humero-ulnar or humero-radial compartment, however, was only observed at complete tear of the lateral capsuloligamentous structures (Table 2).
Discussion
The most important finding was that a high interrater reliability as well as test–retest reliability was observed for the arthroscopic stability assessment. Even in the setting of multiple insufficient ligaments, the arthroscopic assessment provided a high interrater and test–retest reliability in the current study. The ultrasound assessment, however, showed poor measurement reliabilities.
To correctly treat our patients, a precise identification of the affected ligaments in chronic elbow instability is mandatory, yet challenging [24]. A reproducible as well as simple test modality closest to clinical application would allow optimizing surgical treatment and avoid missing relevant ligamentous instabilities. Here, the arthroscopic assessment of the elbow with rods has been introduced [21,22,23,24]. However, the accuracy of an arthroscopic evaluation is unknown [25].
We could observe a reliable and reproducible assessment of lateral elbow instability through the arthroscopic rod technique. Despite a high interrater as well as test–retest reliability for this technique, we found a high inter-individual variance for lateral joint opening in the intact ligamentous state. As observed by McAdams et al. [8], we were also unable to specifically differentiate between isolated RCL and LUCL tears. However, if the surgeon finds a joint gapping of more than 6 mm humero-ulnar, or more than 7 mm humero-radial during elbow arthroscopy, respectively, the surgeon must assume a lesion of the lateral collateral ligament complex. Moreover, if the surgeon observes a joint gapping of more than 9 mm all lateral capsuloligamentous structures are torn. In this scenario, a lateral collateral ligament reconstruction is indicated.
For ultrasound assessment of elbow instability, the interpretation and application were previously reported to be highly dependent on the experience of the examiner [25]. Furthermore, to our knowledge, no standard for evaluating the lateral ligamentous complex with ultrasound exists [26]. However, dynamic ultrasonography can provide a unique view of the radial head subluxation [27]. In the current ultrasound assessment, the elbows were examined at two different flexion angles (30 and 90° elbow flexion) to evaluate the anterior (RCL) or posterior (LUCL) parts of the lateral collateral ligament complex. Here, stress ultrasound resulted in a high variability with low ICC. Despite the usefulness of applying stress ultrasound for the differentiation between a stable and unstable elbow joint, the inconsistent findings make it impossible to objectifying the severity of instability. The inconsistency of data becomes even more obvious when appreciating the high data scattering for ultrasound assessment. A key issue could be—despite efforts to avoid this bias—the loss of the initial measurement plane of the ultrasound transducer due to elbow joint instability, while stress was applied. The effort to find the shortest distance on a correct measuring plane again may explain the tendency to lower mean joint gapping for ultrasound. This underlines the importance to develop a standardized ultrasound stress evaluation protocol which is orientated on clear anatomic landmarks and is robust to stress application. Furthermore, in clinical practice, muscular contraction during testing may further bias instability assessment.
There are limitations to our study that should be considered when interpreting the results. As delineated in the section above, the ultrasonic assessment might have been influenced by deviations in the measurement plane. This might be a disadvantage of our clinical testing setup. However, the variability of the ultrasonic evaluation represents an issue that can occur in the daily clinical examination. The authors preferred to apply a setup closest to their actual clinical setting to achieve a higher clinical relevance. The importance of maintaining transducer stability during sonographic testing has been stressed previously by Camp et al.[15, 28] during sonographic posterolateral rotatory instability testing. The authors suggested video capturing and distance measurements of joint opening on the recorded footage. This would minimize the loss of the measurement plane during instability testing. Furthermore, joint instability was currently evaluated at the humero-ulnar and humero-radial part of the elbow joint to differentiate the exact location of the lesion. However, despite a standardized approach, the anatomy of the lateral collateral ligament of the elbow may be too complex to be evaluated by these two simple measurements. Moreover, arthroscopic testing was only performed at 90° of flexion as sufficient arthroscopic visualization of the posterolateral joint closer to extension was not possible. As mentioned above, the aim of the study was to compare common dynamic testing setups as routinely performed in clinical practice.
A strength of this study is that a test setup closest to the actual clinical setting was applied, which allowed to increase the clinical relevance of this study. Another strength of the current setup is that two measurements were performed in each modality to assess the elbow humero-ulnar as well as humero-radial. The anatomic dissection provided a plausible effect on the elbow joint stability, which was measurable with both modalities.
Conclusion
The arthroscopic rod technique showed a superior interrater and test–retest reliability when compared to stress ultrasound. Arthroscopic assessment for radial elbow instability was found to be reliable and reproducible. A joint gapping ≥ 9 mm in the arthroscopic evaluation is a sign for a complete insufficiency of the radial capsuloligamentous complex. However, it is not possible to precisely distinguish between a lesion of the RCL or LUCL by arthroscopy.
On the basis of our results, dynamic ultrasound testing may be inappropriate to objectify lateral elbow instability.
References
Stoneback JW, Owens BD, Sykes J et al (2012) Incidence of elbow dislocations in the united states population. J Bone Jt Surg 94:240–245. https://doi.org/10.2106/jbjs.j.01663
Charalambous CP, Stanley JK (2008) Posterolateral rotatory instability of the elbow. The J Bone Joint Surg. Br Vol 90:272–279. https://doi.org/10.1302/0301-620x.90b3.19868
Morrey BF (1996) Acute and chronic instability of the elbow. J Am Acad Orthop Sur 4:117–128. https://doi.org/10.5435/00124635-199605000-00001
Hollinger B, Dehlinger F, Franke S (2014) Diagnosis and treatment of elbow instability. Obere Extremität 9:147–155. https://doi.org/10.1007/s11678-014-0280-2
de Haan J, den Hartog D, Tuinebreijer WE et al (2010) Functional treatment versus plaster for si mple el bow dislocations (FuncSiE): a randomized trial. Bmc Musculoskelet Di 11:263. https://doi.org/10.1186/1471-2474-11-263
O’Driscoll SW, Bell DF, Morrey BF (1991) Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am 73:440–446
Geyer S, Aspang JS, Geyer M, Schoch C (2021) Hidden instability in posttraumatic stiff elbows. Eur J Orthop Surg Traumatol 31:1135–1141. https://doi.org/10.1007/s00590-020-02846-5
McAdams TR, Masters GW, Srivastava S (2005) The effect of arthroscopic sectioning of the lateral ligament complex of the elbow on posterolateral rotatory stability. J Shoulder Elbow Surg 14:298–301. https://doi.org/10.1016/j.jse.2004.08.003
Ott N, Hackl M, Wegmann K et al (2020) Lateral epicondylitis. Obere Extremität 15:284–288. https://doi.org/10.1007/s11678-020-00614-9
Regan W, Lapner PC (2006) Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elb Surg 15:344–346. https://doi.org/10.1016/j.jse.2005.03.009
Gustas CN, Lee KS (2016) Multimodality imaging of the painful elbow current imaging concepts and image-guided treatments for the injured thrower’s elbow. Radiol Clin N Am 54:817–839. https://doi.org/10.1016/j.rcl.2016.04.005
Ciccotti MC, Ciccotti MG (2020) Ulnar collateral ligament evaluation and diagnostics. Clin Sport Med 39:503–522. https://doi.org/10.1016/j.csm.2020.02.002
Terada N, Yamada H, Toyama Y (2004) The appearance of the lateral ulnar collateral ligament on magnetic resonance imaging. J Shoulder Elb Surg 13:214–216. https://doi.org/10.1016/j.jse.2003.12.013
Kirschbaum S, Plachel F, Kerschbaum M et al (2021) Does sonography allow an objective and reproducible distinction between stable, hypermobile, and unstable elbow joints? J Shoulder Elb Surg 30:1142–1151. https://doi.org/10.1016/j.jse.2020.11.023
Camp CL, O’Driscoll SW, Wempe MK, Smith J (2017) The sonographic posterolateral rotatory stress test for elbow instability: a cadaveric validation study. Pm&r 9:275–282. https://doi.org/10.1016/j.pmrj.2016.06.014
Maeseneer MD, Brigido MK, Antic M et al (2015) Ultrasound of the elbow with emphasis on detailed assessment of ligaments, tendons, and nerves. Eur J Radiol 84:671–681. https://doi.org/10.1016/j.ejrad.2014.12.007
Goodwin D, Dynin M, Macdonnell JR, Kessler MW (2013) The role of arthroscopy in chronic elbow instability. Arthrosc J Arthrosc Relat Surg 29:2029–2036. https://doi.org/10.1016/j.arthro.2013.08.016
Arrigoni P, Cucchi D, D’Ambrosi R et al (2017) Intra-articular findings in symptomatic minor instability of the lateral elbow (SMILE). Knee Surg Sports Traumatol Arthrosc 25:2255–2263. https://doi.org/10.1007/s00167-017-4530-x
Leschinger T, Müller LP, Wegmann K (2016) Chronic ligamentous instability of the elbow. Orthopade 45:1–13. https://doi.org/10.1007/s00132-016-3324-z
Field LD, Altchek DW (1996) Evaluation of the arthroscopic valgus instability test of the elbow. The Am J Sports Med 24:177–181
Cheung EV (2008) Chronic lateral elbow instability. Orthop Clin N Am 39:221–228. https://doi.org/10.1016/j.ocl.2007.12.007
Savoie FH, Field LD, Gurley DJ (2009) Arthroscopic and open radial ulnohumeral ligament reconstruction for posterolateral rotatory instability of the elbow. Hand Clin 25:323–329. https://doi.org/10.1016/j.hcl.2009.05.010
Fhs III, O’Brien MJ, Field LD, Gurley DJ (2010) Arthroscopic and open radial ulnohumeral ligament reconstruction for posterolateral rotatory instability of the elbow. Clin Sport Med 29:611–618. https://doi.org/10.1016/j.csm.2010.06.008
Field LD, Callaway GH, O’Brien SJ, Altchek DW (1995) Arthroscopic assessment of the medial collateral ligament complex of the elbow. Am J Sports Medicine 23:396–400. https://doi.org/10.1177/036354659502300404
Schmidt-Horlohé K, Klug A, Weißenberger M et al (2018) Acute and chronic instability of the elbow joint. Orthopade 47:695–708. https://doi.org/10.1007/s00132-018-3597-5
Tagliafico AS, Bignotti B, Martinoli C (2015) Elbow US: anatomy, variants, and scanning technique. Radiology 275:636–650. https://doi.org/10.1148/radiol.2015141950
Nocerino EA, Cucchi D, Arrigoni P et al (2018) Acute and overuse elbow trauma: radio-orthopaedics overview. Acta Bio-medica Atenei Parmensis 89:124–137. https://doi.org/10.23750/abm.v89i1-s.7016
Camp CL, Smith J, O’Driscoll SW (2017) Posterolateral rotatory instability of the elbow: part ii. supplementary examination and dynamic imaging techniques. Arthrosc Tech 6:e407–e411. https://doi.org/10.1016/j.eats.2016.10.012
Acknowledgements
We thank Kai Hebick from the Department of Pathology, University Hospital of Augsburg, for his support in preparation of the cadavers.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received.
Author information
Authors and Affiliations
Contributions
JP: conception and design of study, data analysis and interpretation, drafting the work, AO: conception and design of study and drafting, SF: data acquisition and drafting, SS: data analysis and interpretation and revision, BG: data analysis and revision, EM: conception and design of study, final revision, ABI: conception and design of study, final revision, AL: conception and design of study and revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Sebastian Siebenlist reports personal fees from Arthrex GmbH (Munich, Germany), Martin GmbH & Co. KG (Tuttlingen, Germany), Medi GmbH & Co. KG (Bayreuth, Germany) and Medartis AG (Basel, Switzerland), outside the submitted work. Edgar Mayr reports personal fees from Marquardt Medizintechnik Europe, outside the submitted work. Andreas Imhoff reports personal fees from Arthrex (Naples, FL, USA), Medi GmbH & Co. KG (Bayreuth, Germany) and Arthrosurface (Franklin, MA, USA), outside the submitted work. All other authors declare no potential conflict of interest.
Ethical approval
This study was reviewed and approved by the ethical board of the University Hospital of Augsburg (IRB No. 2017–26).
Informed consent
There were no patients involved as for informed consent statement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Plath, J., Otto, A., Förch, S. et al. Arthroscopic rod technique compared to stress ultrasound in the dynamic evaluation of lateral ligament instabilities of the elbow. Arch Orthop Trauma Surg 143, 2087–2093 (2023). https://doi.org/10.1007/s00402-022-04491-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04491-5