Abstract
Purpose
The purposes of this study were to determine demographics and characteristics of patients who underwent spacer exchange for persistent infection in the setting of two-stage arthroplasty for periprosthetic joint infection, to describe the microbiology of pathogens involved, to analyze survivorship free from infection in these patients.
Methods
The institutional prospectively collected database was reviewed to enroll patients with minimum 2 years follow-up. Patients who underwent two-stage procedure for septic arthritis were excluded, as were patients who had spacer fracture or dislocation.
Results
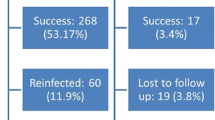
A total of 34 patients (41 procedures) were included. Mean age was 65.0 ± 12.8 years. Mean follow-up was 53.4 ± 24.8 months. Mean number of previous procedures was 3.6 ± 1.2. A total of 27 (79.4%) patients underwent final reimplantation. The most frequently isolated pathogen in spacer exchange was Staphylococcus epidermidis (10 cases, 28.6%). Polymicrobial cultures were obtained from 9 (25.71%) patients, 10 (28.6%) presented culture-negative infections. A total of 11 (32.4%) resistant pathogens were isolated, and 16 (47.0%) difficult to treat pathogens were detected. Eradication rate was 78.8%. Overall survivorship of implants after final reimplantation was 72.8% at 51.8 months.
Conclusion
Surgeons should be aware that subjects necessitating spacer exchange often present multiple comorbidities, previous staged revision failures, soft-tissue impairment and difficult to treat infection. In these patients, spacer exchange provides good clinical results and infection eradication, preventing arthrodesis or amputation.



Similar content being viewed by others
Availability of data and material
Not available.
Code availability
Not available.
References
Signore A, Sconfienza LM, Borens O et al (2019) Consensus document for the diagnosis of prosthetic joint infections: a joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-019-4263-9
Kozaily E, Chisari E, Parvizi J (2020) Is there a role for spacer exchange in two-stage exchange arthroplasty for periprosthetic joint infection? J Clin Med. https://doi.org/10.3390/jcm9092901
Tande AJ, Patel R (2014) Prosthetic joint infection. Clin Microbiol Rev. https://doi.org/10.1128/CMR.00111-13
Risitano S, Sabatini L, Atzori F et al (2018) Static antibiotic spacers augmented by calcium sulphate impregnated beads in revision TKA: surgical technique and review of literature. J Orthop. https://doi.org/10.1016/j.jor.2018.02.008
Siljander MP, Sobh AH, Baker KC et al (2018) Multidrug-resistant organisms in the setting of periprosthetic joint infection—diagnosis, prevention, and treatment. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.07.045
Hansen EN, Zmistowski B, Parvizi J (2012) Periprosthetic joint infection: what is on the horizon? Int J Artif Organs. https://doi.org/10.5301/ijao.5000145
Kapadia BH, Berg RA, Daley JA et al (2016) Periprosthetic joint infection. Lancet. https://doi.org/10.1016/S0140-6736(14)61798-0
McLawhorn AS, Nawabi DH, Ranawat AS (2016) Management of resistant, atypical and culture-negative periprosthetic joint infections after hip and knee arthroplasty. Open Orthop J. https://doi.org/10.2174/1874325001610010615
Burastero G, Basso M, Carrega G et al (2017) Acetabular spacers in 2-stage hip revision: is it worth it? A single-centre retrospective study. HIP Int. https://doi.org/10.5301/hipint.5000446
Pangaud C, Ollivier M, Argenson JN (2019) Outcome of single-stage versus two-stage exchange for revision knee arthroplasty for chronic periprosthetic infection. EFORT Open Rev. https://doi.org/10.1302/2058-5241.4.190003
Kunutsor SK, Whitehouse MR, Lenguerrand E et al (2016) Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS ONE 10:e0139166
Charette RS, Melnic CM (2018) Two-stage revision arthroplasty for the treatment of prosthetic joint infection. Curr Rev Musculoskelet Med. https://doi.org/10.1007/s12178-018-9495-y
Rodriguez-Merchan EC (2015) Knee fusion or above-the-knee amputation after failed two-stage reimplantation total knee arthroplasty. Arch Bone Jt Surg 3:241–243
Tan TL, Goswami K, Kheir MM et al (2019) Surgical treatment of chronic periprosthetic joint infection: fate of spacer exchanges. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.04.016
Logroscino G, Campana V, Pagano S et al (2019) Risk factors for failure of two-stage revision arthroplasty for infected hip prosthesis: review of the literature and single centre cohort analysis. Eur Rev Med Pharmacol Sci 23:65–75. https://doi.org/10.26355/EURREV_201904_17476
Faschingbauer M, Bieger R, Kappe T et al (2020) Difficult to treat: are there organism-dependent differences and overall risk factors in success rates for two-stage knee revision? Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03335-4
Zmistowski B, Tetreault MW, Alijanipour P et al (2013) Recurrent periprosthetic joint infection: persistent or new infection? J Arthroplasty. https://doi.org/10.1016/j.arth.2013.02.021
Parvizi J, Zmistowski B, Berbari EF et al (2011) New definition for periprosthetic joint infection: from the workgroup of the musculoskeletal infection society. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-011-2102-9
Frangiamore SJ, Siqueira MBP, Saleh A et al (2016) Synovial cytokines and the msis criteria are not useful for determining infection resolution after periprosthetic joint infection explantation. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-016-4710-x
Hoell S, Moeller A, Gosheger G et al (2016) Two-stage revision arthroplasty for periprosthetic joint infections: what is the value of cultures and white cell count in synovial fluid and CRP in serum before second stage reimplantation? Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-015-2404-6
Yang J, Parvizi J, Hansen EN et al (2020) 2020 Mark Coventry Award: microorganism-directed oral antibiotics reduce the rate of failure due to further infection after two-stage revision hip or knee arthroplasty for chronic infection: a multicentre randomized controlled trial at a minimum of two years. Bone Jt J. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1596.R1
Izakovicova P, Borens OTA (2019) Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev. https://doi.org/10.1302/2058-5241.4.180092
Zimmerli W, Moser C (2012) Pathogenesis and treatment concepts of orthopaedic biofilm infections. FEMS Immunol Med Microbiol. https://doi.org/10.1111/j.1574-695X.2012.00938.x
Gomez MM, Tan TL, Manrique J et al (2015) The fate of spacers in the treatment of periprosthetic joint infection. J Bone Jt Surg Am. https://doi.org/10.2106/JBJS.N.00958
George J, Miller EM, Curtis GL et al (2018) Success of two-stage reimplantation in patients requiring an interim spacer exchange. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.03.038
Kozaily ME, Timothy L, Tan M, Yacovelli MS et al (2021) Interim spacer exchange for treatment of periprosthetic joint infection: almost half the patients fail subsequently. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.08.028
Metsemakers WJ, Kuehl R, Moriarty TF et al (2018) Infection after fracture fixation: current surgical and microbiological concepts. Injury. https://doi.org/10.1016/j.injury.2016.09.019
Aali Rezaie A, Blevins K, Kuo FC et al (2020) Total hip arthroplasty after prior acetabular fracture: infection is a real concern. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.04.085
Burastero G, Alessio-Mazzola M, Cavagnaro L et al (2020) Conservative two-stage revision with primary components of infected total hip arthroplasty: an analysis of survival, clinical and radiographic outcomes. PLoS ONE. https://doi.org/10.1371/journal.pone.0239981
Yeung CM, Suhardi VJ, Varady NH et al (2020) Trends of prosthetic joint infection organisms and recurrence for a single high-volume arthroplasty surgeon over 20 years. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.10.002
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AC, LC, AR and FC. The first draft of the manuscript was written by AC and all authors commented on previous versions of the manuscript. Entire research study was supervised by GB and AM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval
Ethics approval was obtained by local institutional review board.
Informed consent
Informed consent, publish consent and privacy and data consent were obteined from all the participant to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clemente, A., Cavagnaro, L., Russo, A. et al. Spacer exchange in persistent periprosthetic joint infection: microbiological evaluation and survivorship analysis. Arch Orthop Trauma Surg 143, 1361–1370 (2023). https://doi.org/10.1007/s00402-021-04300-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04300-5