Abstract
Introduction
Patients who require a spacer exchange as part of a two-stage procedure for the treatment of periprosthetic hip and knee joint infections (PJI) have high failure rates. Little is known about the clinical impact of microbiological results and changes in the microbiological spectrum and resistance pattern in these patients.
Material and Methods
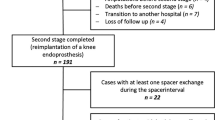
Between 01/2011 and 12/2019, 312 patients underwent a total of 327 two-stage revision arthroplasties at our institution. A spacer exchange was required in 52/312 (16.7%) patients (27 knee/25 hip). Microbiological results, antibiotic resistance patterns, patient’s host factors as well as re-revision and re-infection rates at a median follow-up of 47.8 months (range 12.2–116.7 months) were analyzed. A propensity score (PS)-matched analysis of patients who underwent spacer exchange and patients treated with standard two-stage procedure was performed.
Results
We found a high number of microbiological spectrum changes in patients with multiple culture positive procedures between explantations and spacer exchanges (10/12 [83.3%]), spacer exchanges and reimplantations (3/4 [75%]) as well as between reimplantations and subsequent re-revision surgeries (5/6 [83.3%]). In 9/52 (17.3%) patients, same microorganisms were detected repeatedly in two different procedures. We observed changes in the antibiotic resistance patterns in 6/9 (66.7%) of these patients. High re-infection rates were found in patients with culture positive reimplantations (10/12 [83.3%]), and low re-infection rates were found in patients with culture negative reimplantations (2/40 [5%]; p < 0.001). Between patients with and without spacer exchange, no differences were found in the re-revision rates (13/52 [25%] with vs. 13/52 [25%] without; p = 1.00) as well as re-infection rates (12/52 [23.1%] with vs. 8/52 [15.4%] without; p = 0.32).
Conclusions
Changes in microbiological spectrum and antibiotic resistance patterns between stages are common in patients who require a spacer exchange. If eradication of the microorganism at reimplantation can be accomplished, comparable re-revision rates to standard two-stage procedures can be achieved.


Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Kozaily E, Chisari E, Parvizi J (2020) Is there a role for spacer exchange in two-stage exchange arthroplasty for periprosthetic joint infection? J Clin Med 9:2901. https://doi.org/10.3390/jcm9092901
Klemt C, Smith EJ, Tirumala V et al (2020) Outcomes and risk factors associated with 2-stage reimplantation requiring an interim spacer exchange for periprosthetic joint infection. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.09.012
George J, Miller EM, Curtis GL et al (2018) Success of two-stage reimplantation in patients requiring an interim spacer exchange. J Arthroplasty 33:S228–S232. https://doi.org/10.1016/j.arth.2018.03.038
Tan TL, Goswami K, Kheir MM et al (2019) Surgical treatment of chronic periprosthetic joint infection: fate of spacer exchanges. J Arthroplasty 34:2085-2090.e1. https://doi.org/10.1016/j.arth.2019.04.016
Xu C, Tan TL, Chen JY (2019) Positive culture during reimplantation increases the risk of reinfection in two-stage exchange arthroplasty despite administrating prolonged antibiotics: a retrospective cohort study and meta-analysis. J Arthroplasty 34:1025–1031. https://doi.org/10.1016/j.arth.2019.01.039
Tan TL, Gomez MM, Manrique J et al (2016) Positive culture during reimplantation increases the risk of subsequent failure in two-stage exchange arthroplasty. J Bone Jt Surg Am 98:1313–1319. https://doi.org/10.2106/JBJS.15.01469
Akgün D, Müller M, Perka C, Winkler T (2017) A positive bacterial culture during reimplantation is associated with a poor outcome in two-stage exchange arthroplasty for deep infection. Bone Jt J 99B:1490–1495. https://doi.org/10.1302/0301-620X.99B11.BJJ-2017-0243-R1
Aalirezaie A, Bauer TW, Fayaz H et al (2019) Hip and knee section, diagnosis, reimplantation: proceedings of international consensus on orthopedic infections. J Arthroplasty 34:S369–S379. https://doi.org/10.1016/j.arth.2018.09.021
Hischebeth GT, Randau TM, Ploeger MM et al (2019) Staphylococcus aureus versus Staphylococcus epidermidis in periprosthetic joint infection—outcome analysis of methicillin-resistant versus methicillin-susceptible strains. Diagn Microbiol Infect Dis 93:125–130. https://doi.org/10.1016/j.diagmicrobio.2018.08.012
Tan TL, Kheir MM, Tan DD, Parvizi J (2016) Polymicrobial periprosthetic joint infections: outcome of treatment and identification of risk factors. J Bone Jt Surg Am 98:2082–2088. https://doi.org/10.2106/JBJS.15.01450
Ludwick L, Chisari E, Wang J et al (2021) Emergence of antibiotic resistance across two-stage revision for periprosthetic joint infection. J Arthroplasty 36:2946–2950. https://doi.org/10.1016/j.arth.2021.04.007
Clemente A, Cavagnaro L, Russo A et al (2022) Spacer exchange in persistent periprosthetic joint infection: microbiological evaluation and survivorship analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04300-5
Nodzo SR, Frisch NB (2018) The use of antibiograms in orthopedic surgery. Curr Rev Musculoskelet Med 11:341–346. https://doi.org/10.1007/s12178-018-9496-x
Sousa R, Pereira A, Massada M et al (2010) Empirical antibiotic therapy in prosthetic joint infections. Acta Orthop Belg 76:254–259
Drago L, De Vecchi E, Bortolin M et al (2017) Epidemiology and antibiotic resistance of late prosthetic knee and hip infections. J Arthroplasty 32:2496–2500. https://doi.org/10.1016/j.arth.2017.03.005
Rosteius T, Jansen O, Fehmer T et al (2018) Evaluating the microbial pattern of periprosthetic joint infections of the hip and knee. J Med Microbiol 67:1608–1613. https://doi.org/10.1099/jmm.0.000835
Li ZL, Hou YF, Zhang BQ et al (2018) Identifying common pathogens in periprosthetic joint infection and testing drug-resistance rate for different antibiotics: a prospective, single center study in Beijing. Orthop Surg 10:235–240. https://doi.org/10.1111/os.12394
Frank BJH, Aichmair A, Simon S et al (2021) Analysis of culture positive first and second stage procedures in periprosthetic knee and hip joint infections. J Arthroplast 36:2158–2164. https://doi.org/10.1016/j.arth.2021.01.074
Boelch SP, Jakuscheit A, Luedemann M et al (2021) Do not exchange the spacer during staged TKA exchange! J Orthop 23:41–45. https://doi.org/10.1016/j.jor.2020.12.022
Parvizi J, Tan TL, Goswami K et al (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty 33:1309-1314.e2. https://doi.org/10.1016/j.arth.2018.02.078
McPherson EJ, Woodson C, Holtom P et al (2002) Periprosthetic total hip infection: outcomes using a staging system. Clin Orthop Relat Res 403:8–15
Everhart JS, Andridge RR, Scharschmidt TJ et al (2016) Development and validation of a preoperative surgical site infection risk score for primary or revision knee and hip arthroplasty. J Bone Jt Surg Am 98:1522–1532. https://doi.org/10.2106/JBJS.15.00988
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. https://doi.org/10.1016/0021-9681(87)90171-8
D’Agostino RBJ (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281. https://doi.org/10.1002/(sici)1097-0258(19981015)17:19%3c2265::aid-sim918%3e3.0.co;2-b
Kunutsor SK, Whitehouse MR, Lenguerrand E et al (2016) Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS One 11(3):e0151537. https://doi.org/10.1371/journal.pone.0151537
Staats K, Boehler C, Frenzel S et al (2018) Failed two-stage exchange: factors leading to unachievable endoprosthetic reconstruction after multiple revision surgeries. J Arthroplasty 33:195–199. https://doi.org/10.1016/j.arth.2017.07.049
Bongers J, Jacobs AME, Smulders K et al (2020) Reinfection and re-revision rates of 113 two-stage revisions in infected TKA. J Bone Jt Infect 5:137–144. https://doi.org/10.7150/jbji.43705
Frank BJH, Aichmair A, Simon S et al (2021) Analysis of culture positive 1st and 2nd stage procedures in periprosthetic knee and hip joint infections. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.01.074
George J, Newman JM, Klika AK et al (2018) Changes in antibiotic susceptibility of Staphylococcus aureus between the stages of 2-stage revision arthroplasty. J Arthroplasty 33:1844–1849. https://doi.org/10.1016/j.arth.2018.01.056
Siljander MP, Sobh AH, Baker KC et al (2018) Multidrug-resistant organisms in the setting of periprosthetic joint infection d diagnosis, prevention, and treatment. J Arthroplasty 33:185–194. https://doi.org/10.1016/j.arth.2017.07.045
Acknowledgements
We would like to thank Christina Schober and Dr. Mojgan Prinz for their support in the development of this document and their kind support in data collection.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by BJHF, SS, MD, JGH and AA. The first draft of the manuscript was written by BJHF, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Our study was performed in accordance with the 1964 Declaration of Helsinki and was approved by our institutional review board (Ethics Committee of the Vienna Hospitals of the Vinzenz Group). The Ethics Committee reference number is ‘EK 04/2021.’
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Frank, B.J.H., Simon, S., Aichmair, A. et al. Clinical impact of microbiological results in two-stage revision arthroplasty with spacer exchange. Arch Orthop Trauma Surg 143, 4741–4754 (2023). https://doi.org/10.1007/s00402-023-04770-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04770-9