Abstract
Purpose
Does performing total joint arthroplasty in the afternoon or evening increase the rate of early prosthetic joint infection and the likelihood of early prosthetic joint infection?
Methods
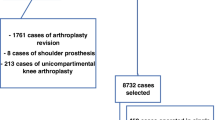
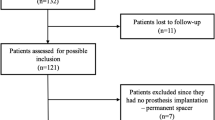
We evaluated patients retrospectively, who underwent primary total hip (THA) or knee arthroplasty (TKA) between January 2016 and December 2019, met the inclusion criteria and had at least 90 days of follow-up. Patients were divided into two groups. Group I consisted of patients whose surgeries had been started and finished before 14:00, and group II included patients whose surgeries started after 14:01. All patients were operated after non-septic cases in specific orthopedic operating rooms. Their demographic data and comorbidities were noted. Primary outcome was to compare the risk of PJI between the groups.
Results
Group I and group II included 2309 and 1881 patients. Total number of patients with the diagnosis of PJI was 58 (1.4%). It was 31 (1.3%) and 27 (1.4%), respectively (p = 0.79). Performing total joint arthroplasty after 14:01 did not increase likelihood of infection (p = 0.83, OR 1.03). Among the parameters, PJI was significantly associated with age (p < 0.01, OR 0.99), smoking status (p < 0.01, OR 0.15) and operating time (p = 0.04, OR 0.99) in TKA and with direct anterior approach (p = 0.02, OR 4.72) in THA. Age (p = 0.06, OR 1.03) was the factor affecting the risk of subsequent PJI after total joint arthroplasty.
Conclusion
Performing total joint arthroplasty in the afternoon or in the evening, after aseptic cases does not increase the risk of subsequent of PJI.

Similar content being viewed by others
References
Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J (2013) Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg Am 95:2177–2184. https://doi.org/10.2106/JBJS.L.00789
Akindolire J, Morcos MW, Marsh JD, Howard JL, Lanting BA, Vasarhelyi EM (2020) The economic impact of periprosthetic infection in total hip arthroplasty. Can J Surg 63:E52–E56
Roth VR, Mitchell R, Vachon J, Alexandre S, Amaratunga K, Smith S, Vearncombe M, Davis I, Mertz D, Henderson E, John M, Johnston L, Lemieux C, Pelude L, Gravel D (2017) Periprosthetic infection following primary hip and knee arthroplasty: the impact of limiting the postoperative surveillance period. Infect Control Hosp Epidemiol 38:147–153. https://doi.org/10.1017/ice.2016.256
Kapadia BHBR, Daley JA, Fritz J, Bhave A, Mont MA (2016) Periprosthetic joint infection. Lancet 387(10016):386–394. https://doi.org/10.1016/S0140-6736(14)61798-0
Everhart JS, Altneu E, Calhoun JH (2013) Medical comorbidities are independent preoperative risk factors for surgical infection after total joint arthroplasty. Clin Orthop Relat Res 471:3112–3119. https://doi.org/10.1007/s11999-013-2923-9
Chen AF, Kheir MM, Greenbaum JM, Restrepo C, Maltenfort MG, Parvizi J (2017) Surgical case order has an effect on the risk of subsequent periprosthetic joint infection. J Arthroplasty 32:2234–2238. https://doi.org/10.1016/j.arth.2017.02.029
Charnley J (1964) A clean-air operating enclosure. Br J Surg 51:202–205. https://doi.org/10.1002/bjs.1800510309
Bischoff PKN, Allegranzi B, Egger M, Gastmeier P (2017) Effect of laminar airflow ventilation on surgical site infections: a systematic review and meta-analysis. Lancet Infect Dis 17(5):553–561. https://doi.org/10.1016/S1473-3099(17)30059-2
Panahi P, Stroh M, Casper DS, Parvizi J, Austin MS (2012) Operating room traffic is a major concern during total joint arthroplasty. Clin Orthop Relat Res 470:2690–2694. https://doi.org/10.1007/s11999-012-2252-4
Li X, Zhang Q, Dong J, Zhang G, Chai W, Chen J (2018) Impact of surgical case order on peri-operative outcomes for total joint arthroplasty. Int Orthop 42:2289–2294. https://doi.org/10.1007/s00264-018-3835-9
Namdari S, Voleti PB, Baldwin KD, Lee GC (2011) Primary total joint arthroplasty performed in operating rooms following cases of known infection. Orthopedics 34:e541-545. https://doi.org/10.3928/01477447-20110714-09
Suda AJ, Heilgeist E, Tinelli M, Bischel OE (2018) High early post-operative complication rate after elective aseptic orthopedic implant removal of upper and lower limb. J Orthop Res 36:1035–1039. https://doi.org/10.1002/jor.23718
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469:2992–2994. https://doi.org/10.1007/s11999-011-2102-9
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27(61–65):e61. https://doi.org/10.1016/j.arth.2012.02.022
Poll AM, Baecker H, Yilmaz E, Jansen O, Waydhas C, Schildhauer TA, Hamsen U (2020) Risk factors and outcome of patients with periprosthetic joint infection admitted to intensive care unit. Arch Orthop Trauma Surg 140:1081–1085. https://doi.org/10.1007/s00402-020-03471-x
Workgroup of the American Association of H, Knee Surgeons Evidence Based C (2013) Obesity and total joint arthroplasty: a literature based review. J Arthroplasty 28:714–721. https://doi.org/10.1016/j.arth.2013.02.011
Duchman KR, Gao Y, Pugely AJ, Martin CT, Noiseux NO, Callaghan JJ (2015) The effect of smoking on short-term complications following total hip and knee arthroplasty. J Bone Joint Surg Am 97:1049–1058. https://doi.org/10.2106/JBJS.N.01016
Namba RS, Inacio MC, Paxton EW (2013) Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg Am 95:775–782. https://doi.org/10.2106/JBJS.L.00211
Aggarwal VK, Weintraub S, Klock J, Stachel A, Phillips M, Schwarzkopf R, Iorio R, Bosco J, Zuckerman JD, Vigdorchik JM, Long WJ (2019) Frank Stinchfield Award: a comparison of prosthetic joint infection rates between direct anterior and non-anterior approach total hip arthroplasty. Bone Joint J. https://doi.org/10.1302/0301-620X.101B6.BJJ-2018-0786.R1
Marchant MH Jr, Viens NA, Cook C, Vail TP, Bolognesi MP (2009) The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am 91:1621–1629. https://doi.org/10.2106/JBJS.H.00116
Maoz G, Phillips M, Bosco J, Slover J, Stachel A, Inneh I, Iorio R (2015) The Otto Aufranc award: modifiable versus nonmodifiable risk factors for infection after hip arthroplasty. Clin Orthop Relat Res 473:453–459. https://doi.org/10.1007/s11999-014-3780-x
George J, Mahmood B, Sultan AA, Sodhi N, Mont MA, Higuera CA, Stearns KL (2018) How fast should a total knee arthroplasty be performed? An analysis of 140,199 surgeries. J Arthroplasty 33:2616–2622. https://doi.org/10.1016/j.arth.2018.03.012
Ahmed SM, Ahmad R, Case R, Spencer RF (2009) A study of microbial colonisation of orthopaedic tourniquets. Ann R Coll Surg Engl 91:131–134. https://doi.org/10.1308/003588409X359402
Grabsch EA, Mitchell DJ, Hooper J, Turnidge JD (2004) In-use efficacy of a chlorhexidine in alcohol surgical rub: a comparative study. ANZ J Surg 74:769–772. https://doi.org/10.1111/j.1445-1433.2004.03154.x
Blomgren GHJ, Nyström B (1990) Reduction of contamination at total hip replacement by special working clothes. J Bone Joint Surg Br 72(6):985–987
Fuchs M, von Roth P, Pfitzner T, Kopf S, Sass FA, Hommel H (2018) Contamination of irrigation fluid during primary total knee arthroplasty. J Am Acad Orthop Surg Glob Res Rev 2:e027. https://doi.org/10.5435/JAAOSGlobal-D-17-00027
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical review committee statement
This retrospective study was approved by the institutional review board (45446446-010.99-4383).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yıldız, F., Aliyev, O., Erden, T. et al. Does performing total joint arthroplasty in the afternoon or evening increase the risk of prosthetic joint infection?. Arch Orthop Trauma Surg 141, 321–326 (2021). https://doi.org/10.1007/s00402-020-03673-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03673-3