Abstract
Introduction
Venous thromboembolism (VTE) is an important problem in orthopedic trauma patients. An association between VTE and upper extremity injury has not been reported. The purpose of this investigation was to determine whether upper extremity trauma is an independent risk factor for lower extremity VTE. This study also attempted to identify associations between VTEs and demographic and injury variables in patients that sustained upper extremity trauma.
Methods
Eleven years of data from the trauma registry at our Level I trauma center was retrospectively reviewed in an injury-matched cohort study. From an initial pool of 646 patients who sustained upper extremity trauma, 32 subjects (4.95%) were identified as having major upper extremity injuries as well as thromboembolic complications. Thirty-two injury-matched controls were randomly selected from the 646 patients with major upper extremity injuries. Regression analysis was performed to determine variables that were significantly associated with lower extremity thromboembolic complications.
Results
Overall incidence of VTE in patients sustaining upper extremity injury was 4.95% (deep vein thrombus 4.64%, pulmonary embolism 0.31%) and was similar to the 4.95% VTE rate in patients without upper extremity injury. Major head injury (p = 0.022) occurred at increased frequency in the VTE group. Patients with increased length of hospital stay (p < 0.001) and length of time on a ventilator (p = 0.002) were at significantly higher risk for thromboembolic complications. No patient with isolated upper extremity trauma had complications from VTE.
Conclusion
Lower extremity VTE occurs at similar rates in patients sustaining upper extremity injury compared to those patients that do not. Major upper extremity orthopedic trauma is not an independent risk factor for lower extremity VTE, and current clinical management guidelines for VTE prophylaxis are adequate for patients sustaining major upper extremity trauma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE) is a life-threatening complication of major trauma and accounts for significant morbidity and mortality in the trauma population. The incidence of deep vein thrombus (DVT) and pulmonary embolism (PE) is significantly increased in immobilized patients as well as patients sustaining major trauma. Initial autopsy studies investigating trauma patients revealed PE as the cause of death in 20% of patients [1]. The rate of lower extremity VTE in patients that are not prophylaxed is reported to be 58%; 69% of patients sustaining lower extremity orthopedic injuries develop DVTs [2]. The incidence of PE in trauma patients has been reported to be between 2 and 22% [3], with nearly 40% of patients with symptomatic proximal DVTs found on pulmonary angiogram to have asymptomatic PE [4]. Patients sustaining major trauma have less physiologic reserve with which to cope with the deleterious physiologic effects of a PE.
Many studies have investigated specific risk factors for development of VTE. Geerts et al. [2] identified age, blood transfusions, surgery, lower extremity fracture, and spinal cord injury as independent risk factors for DVT. Various studies have also implicated increased age, extremity injury, head injury, thoracic injury, and surgery as risk factors [5–7]. Menakar et al. [8] looked at specific types of injuries and found the highest association of PE in those patients incurring femur/lower leg (38%), thoracic (37%), spinal (30%), and pelvic (22%) injuries.
Early intervention to prevent VTE is paramount in preventing morbidity and mortality in these patients. The use of low molecular weight heparin combined with mechanical prophylaxis appears to be effective in decreasing the incidence of fatal PE and significant DVT [3, 9, 10]. However, risk factors for VTE must be balanced with the potential bleeding complications, increased risk of wound drainage, and other side effects such as thrombocytopenia. The ability to determine which subgroups are at higher risk for developing VTE and subsequently need increased vigilance and prophylactic anticoagulation may help clinicians in their decision-making.
Although the development of DVT and PE in pelvic and lower extremity trauma has been investigated in various studies, the incidence of VTE in patients with major upper extremity trauma has never been reported previously. To our knowledge, the impact of upper extremity trauma on lower extremity VTE has not yet been described. The goal of this study was to determine the incidence of VTE in patients with upper extremity trauma and to establish whether upper extremity trauma is an independent risk factor for lower extremity thromboembolic complications using a long-running trauma database at a single institution. This study also aims to elucidate which patient variables correlate with VTE in those sustaining upper extremity trauma.
Materials and methods
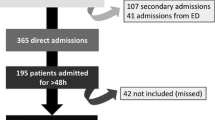
Between 1 January 1997 to 31 December 2007, 10,268 patients sustaining blunt trauma were admitted at a Level I trauma center and were prospectively entered into a trauma database. After institutional review board approval, information was retrospectively obtained from this database, and medical records were reviewed to identify 4,706 patients that met the pre-defined inclusion criteria with complete data points for collection.
The inclusion criteria for the study group were major upper extremity injury, including shoulder dislocations, upper extremity amputations not including the hand, and fractures of the glenoid, humerus, or forearm, and diagnosis of DVT or PE during hospital course. DVT was defined as an acute occlusive thrombus as documented by ultrasound, venogram, impedance plethysmography, or autopsy. PE was defined as a positive study by pulmonary arteriography, post-mortem exam, or initiation of treatment based on radionucleotide scanning. All patients during this time period were subject to routine DVT prophylaxis as outlined in the Clinical Management Guidelines [11] (Fig. 1). In this four-tiered program, “low risk” patients are not screened and do not receive DVT prophylaxis. “Medium risk” patients get prophylaxis but no screening. Patients in the “high risk” and “very high risk” groups underwent surveillance lower extremity ultrasound within 72 h of admission and then serially every 5–7 days. Additionally, “very high risk” patients receive an inferior vena cava (IVC) filter. This management guideline was instituted at the beginning of the study and was not modified over the course of the study. Routine upper extremity DVT surveillance was not undertaken as part of the clinical management guidelines. Exclusion criteria included: discharge to home directly from resuscitation bay, crucial data points missing, diagnosis of DVT or PE that could not be confirmed.
Deep vein thrombus prophylaxis clinical practice guidelines as described by Frankel et al. [11]. Asterisk SCDs are used if one or both lower extremities are accessible. Dagger Excluded or contraindicated in patients with epidural catheters. AIS Apache Injury Score, GCS Glasgow Coma Scale, ISS Injury Severity Score, IVC inferior vena cava, SCD sequential compression device
Of the 4,706 patients, 233 were found to have either DVT or PE. Of this group of patients with VTE, 32 had sustained a major upper extremity injury; these patients served as our case group. This case group included 1 glenoid fracture, 4 shoulder dislocations, 11 humerus fractures, 14 forearm fractures, and 2 upper extremity amputations. An injury-matched control group was formed from the trauma database. Of the 4,706 patients that had sustained blunt trauma, major upper extremity injury was identified in 646 patients including 29 glenoid fractures, 33 shoulder dislocations, 205 humerus fractures, 369 forearm fractures, and 10 upper extremity amputations. In order to have an equal number of control and study subjects for each injury subgroup, control subjects were placed in order by admit date, then a random number generator was used to select matched controls equal in number to the study group in a 1:1 fashion (i.e. of the 205 humerus fractures in the control subject pool, 11 were randomly selected to be in the control group).
Demographic data collected for all subjects included age, gender, weight, and height. Medical co-morbidities including coronary artery disease, history of cancer, hypertension, or diabetes were also collected. Concomitant injuries were classified by group and were defined as follows: (1) pelvic injuries included any bony injury involving the pelvis, sacrum, or acetabulum; (2) major lower extremity injuries included fractures of the femur or tibia including pilon fractures and open ankle fractures (but not closed ankle fractures), hip and knee dislocations, ankle fracture dislocations, and traumatic amputations; (3) minor lower extremity injuries included closed foot fractures and closed ankle fractures; (4) injuries to the spinal column included fractures or dislocations of the spinal column except the sacrum; (5) spinal cord injury; (6) major head trauma included subdural or epidural hematoma, subarachnoid or intraventricular bleed, pneumocephalus, and depressed skull fractures; (7) major thoracic trauma included cardiac or aortic injury, major pneumothorax or hemothorax, pulmonary contusions, rib fractures, and scapula fractures; (8) abdominal or retroperitoneal injuries. Other variables collected included Injury Severity Score (ISS), length of hospital stay, number of days on a ventilator, and mortality.
In cases where the comparison variable was continuous, the Students t test for independent samples was used, with no assumption of equality of variance. In cases where the variable was a count variable or categorical variable, a two-tailed Chi-squared test with Yates correction was used when appropriate. When numbers were too small to accurately use this test, the Fisher’s exact test was utilized. Pearson’s correlation coefficient was used to determine the degree of relationship between VTE rates over time. All statistics were calculated with SPSS version 15 (SPSS Inc., Chicago, IL).
Results
The overall rate of lower extremity VTE and upper extremity injury in the overall population was 4.95% (233/4,706) and 13.7% (646/4,706), respectively. Of the 646 patients sustaining upper extremity injuries, 32 (4.95%) developed either a DVT (30/646, 4.64%) or PE (2/646, 0.31%). A similar 4.95% incidence of lower extremity VTE was calculated for patients who did not incur any upper extremity injury (201/4,061). There was no significant change in the rate of VTE after upper extremity injury over time (Pearson’s coefficient = 0.390, p = 0.300). There was no significant difference between lower extremity VTE in patients with UE trauma compared to patients with no UE trauma (p = 0.997). The number of bilateral upper extremity injuries was similar between the two groups (p = 0.708).
The demographic and descriptive characteristics of the two cohorts are summarized in Table 1. The mean age was similar between the two groups (p = 0.757) with an average of 45.2 years in the control group and 46.7 years in our case group. When stratified by age (<40, 40–60, >60), the groups were also similar with no significant variation in rate of lower extremity VTE. Both cohorts were predominantly male, with a larger proportion in the thromboembolic group than in the control group, although not reaching statistically significant levels (p = 0.140). The rate of medical co-morbidities was not different between the two groups (p > 0.285).
Concomitant injuries sustained by the two groups are listed in Table 2. Head trauma was the only statistically significant (p = 0.022) concomitant injury associated with VTE. Both the length of hospital stay (25.5 vs. 10.9 days, p = 0.002) and the number of days on a ventilator (12.3 vs. 2.6 days, p < 0.001) were significantly higher in the thromboembolic group than the control group. Major lower extremity injury (p = 0.140) and spinal column injury (p = 0.107) approached significance. Of note, the two patients that developed PE in this cohort both had pelvic injuries and spinal column injury in addition to upper extremity trauma. There was no statistical difference in mortality rates (15.6% in VTE group vs. 9.7% in control group, p = 0.708).
Discussion
VTE, defined as deep vein thrombus (DVT) or a PE, is common among trauma patients and represents a major health problem that accounts for significant morbidity and mortality. While there is no agreement on the incidence of VTE in trauma patients and uncertainty regarding the correlation between DVT and PE, clinicians agree that prophylaxis is effective and important in preventing potentially fatal PEs. Many different strategies can be utilized to prevent VTEs, including external pneumatic compression devices [12, 13], pharmacologic anticoagulation [9, 10], and prophylactic IVC filter placement [14–16]. However, each method of prophylaxis does not come without expense to the health care system and risks of adverse effects. For this reason, the ability to determine which patients are at a higher risk for developing a VTE after a traumatic injury is essential to the management of these patients and can help determine what method of prophylaxis is most appropriate on a patient-specific basis. A comprehensive literature review reveals that the role of upper extremity trauma in development of VTE and the associated risk factors for development of VTE in patients incurring upper extremity trauma has not yet been investigated and reported. This study presents data showing that upper extremity trauma is not an independent risk factor for lower extremity DVT and PE.
The overall rate of VTE in this study (4.95%) is comparable to other studies with similar populations [2, 5, 7, 8, 17]. Incidence of VTE after trauma varies widely in the literature, most likely due to the various inclusion/exclusion criteria and patient populations, different criteria prompting appropriate DVT or PE workup, and varying use and levels of prophylaxis against thromboembolism in some studies. Although Geerts et al. [2] reported a high rate of lower extremity DVT (58%) and proximal vein thrombosis (18%) in a prospective cohort of 716 patients, all subjects in this study underwent plethysmography or venography to detect DVT regardless of risk factors, and none of the subjects received routine prophylaxis against thromboembolism. This is in contrast to a few large retrospective studies in which the incidence of DVT and/or PE is reported to be around 0.3% [5, 7, 8]. The subjects in these large retrospective studies received early prophylaxis, which has been shown to significantly decrease VTE rate by a multiple of three [18]. Sharma et al. [17], in a similar study of 507 patients that received VTE prophylaxis based on risk factors, reported a 6.1% rate of DVT. These studies are likely to underestimate the true rate of VTE, as studies have shown that asymptomatic PE occurs frequently in patients with DVT [4]. The relatively low rate of VTE in these studies, as well as our reported rate, is likely explained by the fact that not all patients received imaging to detect DVT or PE. In the clinical management guidelines used for this study, only patients with “high” and “very high” risk factors as outlined in the clinical management guidelines underwent routine duplex ultrasound during the hospital course. Also, because these patients received DVT prophylaxis according to clinical guidelines, the rate of DVT will likely be lower than studies in which no prophylaxis was used.
The most salient data in this study pertains to the rate of VTE in patients sustaining upper extremity injury compared to those that do not. The rate of VTE in upper extremity trauma patients was 4.95%, identical to the rate of VTE in the entire blunt trauma population. Notably, no patients that developed VTE incurred a major upper extremity fracture in isolation. Upper extremity trauma does not appear to be an independent risk factor for VTE based on the non-significant difference between VTE rates in the group with upper extremity injury and the group without upper extremity injury. As a result, we conclude that a standard anticoagulation regimen based on current clinical management guidelines is adequate and appropriate for this patient population; increased or more aggressive anticoagulation in patients with upper extremity trauma is unnecessary, as the associated risks would be unwarranted.
In this study, major head trauma was significantly associated with an increased VTE rate. This is unlikely to be limited to the population sustaining upper extremity trauma, as previous literature has supported head trauma as a risk factor for VTE [5]. The increased rate of VTE in major head trauma could be a result of clinicians’ reluctance to aggressively treat VTE in patients with potential evolving head injuries. Also, patients with severe head injuries are likely to spend longer periods of time immobile in the intensive care unit. Immobility from limb immobilization and/or neurologic injury predisposes to the development of VTE [19–21]. The effect of bilateral upper extremity injuries on mobility should also be considered. In our study, although the overall rate of bilateral upper extremity injury was similar between the two groups, our database did not allow us to examine the effect of the bilateral injuries on mobilization. Several other factors, such as weight, concomitant lower extremity injury, and spinal column trauma, also approached significance and would be consistent with other risk factor analyses [2, 5, 6, 8, 22]. Although this study encompasses an 11-year database of blunt trauma at a Level I trauma center, the power of this study would be insufficient to detect small differences in VTE rates, likely because VTE is a rare complication. Of note, pelvic injury, spinal cord injury, and abdominal injury were not associated with VTE in this study, and the rate of VTE in the two groups did not appear to be affected by medical co-morbidities. Length of hospital stay and number of ventilator days were significantly increased in the VTE group—these factors, such as head injury, are likely to indicate an increased injury severity and resultant physiologic insult. An intense hypercoagulable state exists in patients sustaining severe trauma, and some data have shown a correlation between severity of injury and coagulation profile [23]. However, this connection remains unspecified and some investigators have challenged this claim. Meissner et al. [22] demonstrated that although admission fragment 1 + 2 and d-dimer levels were elevated in 81.4 and 100% of patients, respectively, mean levels were not significantly different in those with or without VTE. Only obesity (p = 0.004) and immobilization greater than 3 days (p = 0.05) were independent predictors of VTE in a multivariate analysis. They concluded that although elevated in seriously injured patients, neither markers of activated coagulation nor specific injury patterns are predictive of VTE.
This study has several notable strengths. A large pool of patients was reviewed with a clearly defined cohort of patients with an injury-matched control group for comparison. Clinical management guidelines for VTE prophylaxis were adhered to throughout the entire period from which the patients were selected, and therefore, this population is known to be refractory to routine methods. There are, however, some weaknesses in this study. The clinical management guidelines followed in this study are part of a standard that was developed to manage patients in critical care surgery and was not necessarily designed specifically for trauma patients. The study is retrospective and utilized data up to 11 years old; as such, it was not possible to investigate additional, potentially relevant parameters such as upper extremity versus lower extremity DVT. As mentioned earlier, we were not able to examine the effect of bilateral upper extremity injury on patient mobility, which may have an effect on VTE rate. Nevertheless, we do not believe that these limitations significantly affect our conclusions and believe that this study generates further questions regarding the effective utilization of anticoagulation in upper extremity trauma. Potential investigations include the rate of lower and upper extremity DVT in patients with isolated upper extremity injuries and possibly stratifying proximity of injury to increased or decreased VTE rate, similar to that which has been developed for the lower extremity.
Conclusions
VTE occurs at similar rates in patients sustaining upper extremity injury compared to those blunt trauma patients that do not. Of all patients that developed VTE in this study, no patient had sustained upper extremity injury in isolation. Major head injury, increased number of ventilator days, and longer duration of hospital stay were risk factors for lower extremity VTE. We conclude that in patients sustaining blunt trauma, changes to standard clinical management guidelines for prevention of VTE are not necessary. Major upper extremity orthopedic trauma does not appear to be an independent risk factor for lower extremity VTE that warrants special attention in management guidelines.
References
Sevitt S, Gallagher N (1961) Venous thrombosis and pulmonary embolism. A clinico-pathological study in injured and burned patients. Br J Surg 48:475–489
Geerts WH et al (1994) A prospective study of venous thromboembolism after major trauma. N Engl J Med 331(24):1601–1606
Hak DJ (2001) Prevention of venous thromboembolism in trauma and long bone fractures. Curr Opin Pulm Med 7(5):338–343
Moser KM et al (1994) Frequent asymptomatic pulmonary embolism in patients with deep venous thrombosis. JAMA 271(3):223–225
Knudson MM et al (2004) Thromboembolism after trauma: an analysis of 1602 episodes from the American College of Surgeons National Trauma Data Bank. Ann Surg 240(3):490–496 (discussion 496–8)
Azu MC et al (2007) Venous thromboembolic events in hospitalized trauma patients. Am Surg 73(12):1228–1231
Tuttle-Newhall JE et al (1997) Statewide, population-based, time-series analysis of the frequency and outcome of pulmonary embolus in 318,554 trauma patients. J Trauma 42(1):90–99
Menaker J, Stein DM, Scalea TM (2007) Incidence of early pulmonary embolism after injury. J Trauma 63(3):620–624
Geerts WH et al (1996) A comparison of low-dose heparin with low-molecular-weight heparin as prophylaxis against venous thromboembolism after major trauma. N Engl J Med 335(10):701–707
Rogers FB et al (2002) Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma 53(1):142–164
Frankel HL et al (1999) Strategies to improve compliance with evidence-based clinical management guidelines. J Am Coll Surg 189(6):533–538
Fisher CG et al (1995) Effectiveness of pneumatic leg compression devices for the prevention of thromboembolic disease in orthopaedic trauma patients: a prospective, randomized study of compression alone versus no prophylaxis. J Orthop Trauma 9(1):1–7
Tarnay TJ et al (1980) Pneumatic calf compression, fibrinolysis, and the prevention of deep venous thrombosis. Surgery 88(4):489–496
Rodriguez JL et al (1996) Early placement of prophylactic vena caval filters in injured patients at high risk for pulmonary embolism. J Trauma 40(5):797–802 (discussion 802–4)
Langan EM 3rd et al (1999) Prophylactic inferior vena cava filters in trauma patients at high risk: follow-up examination and risk/benefit assessment. J Vasc Surg 30(3):484–488
Rogers FB et al (1995) Routine prophylactic vena cava filter insertion in severely injured trauma patients decreases the incidence of pulmonary embolism. J Am Coll Surg 180(6):641–647
Sharma OP et al (2007) Venous thromboembolism in trauma patients. Am Surg 73(11):1173–1180
Nathens AB et al (2007) The practice of venous thromboembolism prophylaxis in the major trauma patient. J Trauma 62(3):557–562 (discussion 562–3)
Beam DM et al (2009) Risk of thromboembolism varies, depending on category of immobility in outpatients. Ann Emerg Med 54(2):147–152
Dalen JE (2002) Pulmonary embolism: what have we learned since Virchow? Natural history, pathophysiology, and diagnosis. Chest 122(4):1440–1456
Wells PS et al (2000) Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED d-dimer. Thromb Haemost 83(3):416–420
Meissner MH, Chandler WL, Elliott JS (2003) Venous thromboembolism in trauma: a local manifestation of systemic hypercoagulability? J Trauma 54(2):224–231
Engelman DT et al (1996) Hypercoagulability following multiple trauma. World J Surg 20(1):5–10
Conflict of interest statement
The authors are aware of no conflicts of interest, financial or otherwise, related to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsu, J.E., Namdari, S., Baldwin, K.D. et al. Is upper extremity trauma an independent risk factor for lower extremity venous thromboembolism? An 11-year experience at a Level I trauma center. Arch Orthop Trauma Surg 131, 27–32 (2011). https://doi.org/10.1007/s00402-010-1094-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-010-1094-3