Abstract
Background
Dietary-based primary prevention guidelines for chronic kidney disease (CKD) treatment are lacking due to limited evidence. Single nutrient intake studies do not account for complex dietary interactions. We assessed associations between dietary patterns and renal function in the Northern Ireland Cohort for the Longitudinal Study of Ageing (NICOLA).
Design
A cross-sectional observational study used NICOLA baseline dietary data collected between February 2014 and March 2016 via a food frequency questionnaire for 2590 participants aged ≥ 50 years. Principal component analysis identified a posteriori dietary patterns. Renal function was characterised by estimated glomerular filtration rate (eGFR) using serum creatinine and cystatin-C. Associations were assessed according to quintiles of dietary pattern adherence and multivariable regression analysis examined associations with eGFR.
Results
Variation in three dietary patterns was significantly associated with eGFR. After adjustment for potential confounders, participants with least adherence to the ‘healthy’ dietary pattern 1 had a mean eGFR 3.4 ml/min/1.73m2 (95% confidence interval, [CI] − 5.0, − 1.7, p < 0.001) lower than the most adherent. Those with lowest adherence to the ‘unhealthy’ dietary pattern 2 had a mean eGFR 1.9 ml/min/1.73m2 (CI 0.2, 3.5, p = 0.03) higher than those with highest adherence. Participants with lowest adherence to dietary pattern 3, characterised by a high consumption of alcohol and coffee, had a mean eGFR 1.8 ml/min/1.73m2 (− 3.5, − 0.01, p = 0.05) lower than those with greatest adherence.
Conclusions
Our findings identify independent associations between dietary patterns and eGFR. These findings can inform the development of diet-related primary prevention advice for CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dietary contributions to the aetiology of chronic kidney disease (CKD) are not well characterised and, as a result, guidelines for primary prevention specific to CKD are lacking due to limited published evidence. Existing dietary guidelines target the primary prevention of important risk factors for CKD, including hypertension [1, 2] and type 2 diabetes, [3, 4] and the secondary prevention of hypertension, including factors related to vascular calcification, hyperkalaemia, and disease progression in CKD [5].
Diets in free-living populations are variable and complex and comprise a myriad of foods, eaten separately or together as meals. Given this complexity and the inherently multidimensional impact of foods (i.e. individual nutrient effects are co-dependent on other constituents of the diet), the association with health outcomes may depend on overall dietary pattern rather than single macro- or micronutrient intake [3]. Single nutrient intake studies do not sufficiently account for competitive, compositional and synergistic interactions between the constituent vitamins, minerals, phytonutrients, etc. found in foods, and may not confer observable benefits for free-living populations [3]. Dietary pattern approaches are now reflected in contemporary dietary recommendations for the prevention and management of conditions, such as cardiovascular disease [1, 2] and type 2 diabetes [3, 4].
Conceptually healthier interventions based on dietary patterns such as the Dietary Approaches to Stop Hypertension (DASH) diet have been shown to be associated with reduced CKD risk [6,7,8,9,10,11] and progression [12]. Likewise, traditional location-specific dietary patterns such as the Mediterranean diet, have also been associated with lower CKD risk [11, 13,14,15,16,17,18,19,20] and reduced CKD progression [21] in several populations. However, high levels of adherence to a-priori derived dietary patterns, such as the Mediterranean diet, can necessitate changes in food choice and food preparation methods that may present a barrier to adherence.
Studies to identify a posteriori dietary patterns in local populations and to examine the associations with renal health have been conducted in diverse populations including cohorts in the USA [6, 22, 23], Taiwan [19, 24], Brazil [18], and China [25]. A dietary pattern characterised by consumption of red meat, alcohol, sugar-sweetened beverages, and a low intake of fish, chicken, sweets, and salt was more common in those with CKD and those on haemodialysis in a Brazilian population [18]. In an American cohort (The Multi-Ethnic Study of Atherosclerosis), adherence to a dietary pattern characterised by consumption of fruits, vegetables, wholegrains, and low-fat dairy was associated with a lower urinary albumin/creatinine ratio [22]. Another study conducted in eight south-eastern US states identified a variety of local dietary patterns including a plant-based diet and a traditional “Southern” diet of meat, fried food, and sweetened beverages. Individuals with CKD and stronger adherence to the Southern dietary pattern had higher mortality rates compared to those with CKD consuming a plant-based dietary pattern [23].
In a Taiwanese population, a dietary pattern characterised primarily by a greater consumption of meat, offal, processed food, rice and flour products,, and low consumption of dark-coloured fruit and vegetables, was associated with a small, increased risk of poorer renal function [19]. In a Taiwanese population with diabetes, three dietary patterns were identified; a high-fat diet, a traditional Chinese diet, and a diet rich in fish and vegetables. The dietary pattern rich in fish and vegetables was associated with better renal function compared to the others [24]. In contrast, a Chinese population-based study of a posteriori dietary patterns in an area where industrial pollutants are commonly reported to contaminate fresh food products, identified an association between a traditional Chinese diet, resembling the Mediterranean diet, and increased risk of CKD [25].
These studies highlight the benefits of evaluating the effects of conceptually healthy and naturally existing dietary patterns in a region-specific manner. However, there is little evidence in British and Irish populations, which likely differ markedly in their dietary habits and the type and quality of available foods compared to other populations. In the Irish Nun Eye Study (INES [26]), greater adherence to an unhealthy dietary pattern was associated with a reduction in renal function equivalent to 14 years of the mean annual age-related renal decline as reported in the Cardiovascular Health Study [27]. However, the INES comprised cloistered nuns and generalisability to the wider population cannot be assumed. Therefore, this study aimed to identify associations between culturally relevant dietary patterns and renal function in a population of older adults from the Northern Ireland Cohort for the Longitudinal Study of Ageing (NICOLA). The findings will help to inform diet-related primary prevention advice for CKD in older people.
Methods
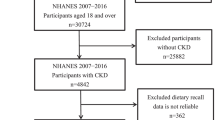
Data from Wave 1 of NICOLA were used to test associations between renal function and dietary patterns specific to the Northern Ireland population. This study collected health and lifestyle data from 8452 free-living individuals in Northern Ireland, aged 50 years and over with planned 10-year follow-up assessments for consenting participants. Baseline data were collected between December 2013 and March 2016 (NCT number: NCT01938898 [28]). The study adhered to principles outlined in the Declaration of Helsinki.
Data collection included a health assessment, a self-completion questionnaire and a computer-assisted personal interview. Blood samples were collected as part of the health assessment. Renal function was assessed as the estimated glomerular filtration rate (eGFR) calculated using the combined CKD-EPI equation for serum creatinine and cystatin-C from a blood sample collected at a single time point [5]. Dietary intake was assessed using the validated 130-item food frequency questionnaire (FFQ), previously used by the European Prospective Investigation of Cancer (EPIC) study [29]. For each food item on the FFQ, participants specified their frequency of consumption (in the previous 12 months) ranging from never or less than once per month, 1–3 times per month, once a week, 2–4 per week, 5–6 per week, once a day, 2–3 per day, 4–5 per day and 6 + times per day which were converted into estimated daily gram weights using standardised Food Portion Sizes [30].
Other variables
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) measurements were the average of two independent readings. Diabetic status was defined using a combination of participant percentage haemoglobin A1c (HbA1c > 6.5%), diabetic medication use or self-reported diabetes. Self-reported medication use was defined according to the Anatomical Therapeutic Chemical (ATC) Classification System based on the active ingredients of drugs according to the organ or system on which they act and their therapeutic, pharmacological and chemical properties. Educational attainment was classified as completing primary, secondary or tertiary level education. Smoking status was characterised as current, past or non-smoker. Alcohol consumption was categorised into three groups: non-drinker, drinker and ex drinker.
Statistical methods
Statistical analyses were conducted using SPSS v24 (IBM, Chicago, Illinois, USA). Continuous variables were summarised using means and standard deviations. Categorical variables were summarised using frequencies and percentages. The dietary pattern analysis has been described previously [29]. In brief, individual foods and drinks from the FFQ were clustered into 34 food groups based on food type. These food groups were used to generate dietary patterns using principal component analysis (PCA) with orthogonal (varimax) rotation. The PCA generated factor loadings for each food group. The number of factors retained was based on the number of points above the breakpoint on the scree plot. Food groups with factor loadings greater than 0.2 were retained as they were considered informative in describing the dietary pattern. Dietary pattern adherence scores were computed for each participant by summing the intakes of food groups weighted by their factor loading. Dietary pattern scores were categorised into quintiles of adherence to each dietary pattern. The highest quintile, reflecting greatest conformity to the pattern, was designated as the reference category for regression analyses.
Differences in mean eGFR between quintiles of dietary pattern adherence were assessed using one-way analysis of variance (ANOVA). Adjustment for multiple comparison was carried out using Student–Neuman–Keuls (SNK) post hoc test. Differences in categorical variables between quintiles of adherence were assessed using the Kruskal–Wallis test with post hoc pairwise Mann–Whitney U tests to determine the location of differences. Multivariable linear regression analysis was used to assess associations between eGFR and dietary pattern adherence. Adjusted models controlled for age, sex, diabetes status, SBP, smoking status, alcohol consumption, waist circumference, high-density lipoprotein (HDL), low-density lipoprotein (LDL), lipid-modifying agent use, antihypertensive and diabetes drug use, multiple-deprivation score, and education level. In a sensitivity analysis, we tested for associations of interactions between eGFR and dietary pattern adherence by BMI category and for those 65 < age ≤ 65 years. For all analyses, p < 0.05 was considered statistically significant. Study datasets are available from the corresponding author following reasonable request.
Results
NICOLA baseline characteristics for the 2590 participants with both dietary pattern and renal function data are shown in Table 1. The sample included 1224 (47%) males and 1366 (53%) females with a mean age of 64.4 years (SD = 9.3). Mean systolic/diastolic blood pressure was 133/81 mmHg (SD = 18/11), and mean waist circumference was 95.1 cm (SD = 13.9), which is above the healthy central adiposity threshold for both men and women. The mean BMI for all participants was 28.7 kg/m2 with 589 (23%) having a BMI < 25 kg/m2, 1139 (44%) BMI ≥ 25 kg/m2 but < 30 kg/m2 and 862 (23%) had a BMI ≥ 30 kg/m2. Mean HDL cholesterol was 1.61 mmol/L (SD = 0.44) and mean LDL cholesterol was 3.34 mmol/L (SD = 1.10). Nine percent of participants had diabetes mellitus and 40% were hypertensive (defined as a SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg or if use of antihypertensive medication was self-reported). The mean eGFR was 73.5 ml/min/1.73m2 (SD = 16.3). The majority (85%) of participants had completed at least secondary level education, 54% had never smoked, and 69% currently consumed alcohol. A lipid-modifying agent was being used by 34% of participants; 6% used medication to treat their diabetes, and 2% used antihypertensive medication.
Three dietary patterns met the retention criteria of Eigenvalues greater than 1 and above the scree plot breakpoint. The food components and factor loadings of each dietary pattern are described in Table 2. A healthy dietary pattern 1 was defined by high factor loadings for (and more frequent consumption of) vegetables, wholegrains, fruit, oily fish, dairy, and white fish. An unhealthy dietary pattern 2 was characterised by high factor loadings for (and greater intake of) processed meat, white bread, confectionary, fried potatoes, red meat, and added sugar. Dietary pattern 3 was characterised by high factor loadings for (and greater intake of) coffee, wine, beer, other alcohol, refined grains, crisps, and lasagne/pizza but negative factor loadings for (and low intake of) butter, margarine, confectionary, higher fibre breads, cereals, natural potatoes, and tea. Together, these three dietary patterns accounted for approximately 22.3% of the total variance in this population.
The difference in mean renal function for participants, divided by quintiles of adherence to dietary patterns is shown in Table 3. For the healthy dietary pattern 1, those in the lowest three quintiles of adherence had significantly poorer renal function (eGFR) than those with the highest intake of foods associated with this dietary pattern: least adherent: eGFR 71.3 ml/min/1.73m2 (SD: 16.6; p < 0.001) compared to the highest adherence eGFR 76.0 ml/min/1.73m2 (15.6; reference category). These differences remained significant in the adjusted model where the least adherent quintile had an eGFR mean difference of − 3.4 ml/min/1.73m2 (95% confidence interval − 5.0, − 1.7; p < 0.001) compared to the most adherent reference category. The association between adherence to dietary pattern 1 and eGFR was significant in both the unadjusted and adjusted models (p for trend < 0.001). In a sensitivity analysis dichotomised by 65 < age ≥ 65 years, the effect size was diminished in those aged ≥ 65 years but was no longer significant in the smaller sample size, although the trend remained the same (P = 0.09; supplementary Tables 1, 2 and 3).
For the unhealthy dietary pattern 2, those in the lowest quintile of adherence had significantly better renal function than those in the reference category, i.e. the highest intake of foods associated with dietary pattern 2. Least adherent quintile: eGFR 76.2 ml/min/1.73m2 (16.2; p = 0.02) compared to the most adherent eGFR 73.8 ml/min/1.73m2 (16.3; reference category). These differences remained significant in the adjusted model where the least adherent quintile had an eGFR mean difference 1.9 ml/min/1.73m2 (0.2, 3.5], p = 0.03) compared to the most adherent reference category. The association between adherence to dietary pattern 2 and eGFR was significant for both the unadjusted (p = 0.04) and adjusted models (p for trend = 0.02) and this effect was largely driven by those aged ≥ 65 years (P = 0.006; Supplementary tables 1, 2 and 3).
For dietary pattern 3, characterised by a high consumption of alcohol and coffee, those with lower adherence had significantly poorer renal function than those with the highest intake of foods associated with this dietary pattern (least adherent quintile: eGFR 70.0 ml/min/1.73m2 (15.9; p < 0.001) compared to the most adherent quintile: eGFR 78.1 ml/min/1.73m2 (15.3; reference category). These differences remained significant in the adjusted model where the least adherent quintile: eGFR − 1.8 ml/min/1.73m2 (− 3.5, − 0.01; p = 0.05) compared to the most adherent reference category. The association between adherence to dietary pattern 3 and eGFR was significant for both the unadjusted (p for trend < 0.001) and adjusted models (p for trend = 0.001). In a sensitivity analyses stratified by those aged < 65 years remained significant (P = 0.002), although the association with those aged ≥ 65 years was just above the significance threshold for (P = 0.06; Supplementary tables 1, 2 and 3).
Sensitivity analyses by BMI categories identified no significant interaction or deviation in the associations reported between eGFR and dietary pattern adherence (data not shown).
Discussion
In this free-living, population-based cohort, comprising adults ≥ 50 years old in Northern Ireland, three a posteriori dietary patterns were identified. Low adherence to a dietary pattern characterised by consumption of processed meats, white bread, confectionary, fried potatoes, red meat, added sugar, etc. (dietary pattern 2), was associated with higher eGFR and this effect was stronger in those aged < 65 years. In contrast, poor adherence to the two other dietary patterns were associated with lower eGFR. These were dietary pattern 1, characterised by consumption of vegetables, wholegrains, fruits, oily fish, dairy, white fish etc., and dietary pattern 3, characterised by high intakes of drinks such as coffee, wine, beer and other alcohol, but low intakes of butter, margarine, confectionary, higher fibre breads, cereals, natural potatoes and tea. These associations were independent of diabetes status, blood pressure and other measured potential confounding factors.
There was considerable overlap between the characteristics of the dietary patterns observed and the components of other conceptually healthy and unhealthy dietary patterns. The healthy dietary pattern 1 was characterised by consumption of foods similar to those found in the Mediterranean and DASH diets, while the unhealthy dietary pattern 2 was principally comprised of foods similar to those found in “Western diets” which have been associated with conditions such as diabetes and cardiovascular disease. Likewise, both of these dietary patterns were similar to those reported previously in the geographically overlapping INES [26], wherein the observed diets were labelled as the “unhealthy” and “healthy” dietary patterns. In the INES, the unhealthy pattern was associated with significantly poorer renal function, while no associations were detected between adherence to the healthy dietary pattern and kidney function. The INES provided evidence consistent with a detrimental effect of consumption of unhealthy food types but failed to support the beneficial effects for the consumption of what would be regarded as healthy foods. In contrast, the present study, conducted in a more generalizable and free-living, but geographically similar population, confirmed the association between consumption of a naturally occurring diet similar to those in the INES unhealthy dietary pattern but also showed a protective effect of a diet rich in fruits, vegetables, and fish. Of note, the NICOLA was more than twice the size of the INES, included both men and women and as such, had greater power to detect associations with improved sensitivity of the effect sizes observed. The effect size of the association for each dietary pattern was smaller than the effect size of the association observed between the unhealthy dietary pattern and renal function in the INES. Lowest adherence to dietary pattern 2 was associated with a 1.9 ml/min/1.73m2 increase in eGFR compared to a 6 ml/min/1.73m2 increase in renal function for those in the least adherent group for the unhealthy dietary pattern in the INES. The reductions in eGFR associated with low adherence to dietary patterns 1 and 3 were closer in magnitude at 3.4 ml/min/1.73m2 and 1.75 ml/min/1.73m2. The magnitude of these associations is equivalent to a year or more of annual age-related loss of renal function as reported in the Cardiovascular Health Study [27]. Although both studies undertook age-adjusted analyses, the smaller effect size observed between dietary pattern 2 adherence and eGFR in the present study, compared to the similarly unhealthy dietary pattern observed in the INES population, may be explained by the older mean age of participants in the INES and the associated age-related decline in eGFR. Furthermore, the sensitivity analyses stratified by age in the current study suggest an age-related effect which is perhaps unsurprising, given the gradual loss of renal function as we grow older, with a mean eGFR = 66 ml/min/1.73m2 in those aged ≥ 65 years versus 81 ml/min/1.73m2 in those aged < 65 years. Given the possibility of over adjustment for age (it was included as a potential confounder in the adjusted regression models, it was used to dichotomise the study sample (65 < age ≥ 65 years) thereby reducing statistical power, and given its role in estimating glomerular filtration rate, the findings from the sensitivity analyses should be interpreted with caution.
Dietary pattern 3 from the NICOLA study did not resemble any of the dietary patterns from the INES, despite the similar geographic location. This dietary pattern was characterised by a high intake of coffee, alcohol, crisps and pizza and a low intake of high-fibre breads, spreads and tea. The non-existence of this dietary pattern in the INES population may be unsurprising among those practicing a cloistered and religious lifestyle. Although conceptually unhealthy, low adherence to this dietary pattern was associated with poorer renal function in the current study. However, this finding may yet be related to confounding influences which were not controlled for, or, may result from the high intake of coffee [31] and alcohol [32,33,34,35], or greater total fluid intake [36, 37], which have been associated with better renal function, despite the associations between alcohol and other related conditions.
Several other active food constituents in the dietary patterns observed have been previously associated with renal function. Reduced endogenous antioxidant production has been reported in individuals with end-stage renal disease (ESRD) requiring haemodialysis [38], and antioxidant supplementation has been reported to reduce the rate of decline in renal function [39]. Interestingly, a wide variety of fruits and vegetables contain substances with antioxidant capacity including vitamins A, C and E, and poly-phenolics [40, 41] and associations between xanthophyll serum carotenoid and eGFR have been previously reported [42]. Similarly, fruits and vegetables contain a wide variety of anti-inflammatory substances which regulate nitric oxide production, the cyclooxygenase pathway, prostaglandin production and macrophage function such as poly-phenolics, triterpenoids, saponins, lectins, etc. [41]. The fibre found within fruits, vegetables and grains may also be beneficial, with every 5 g increase in daily fibre intake associated with an 11% reduction in CKD incidence [43].
Oily fish are rich in long-chain, n-3 polyunsaturated fatty acids which act on the cyclooxygenase pathway and arachidonic acid pathway to reduce the production of a variety of inflammatory mediators [44]. Moreover, animal models of fish derived dietary proteins were shown to have lower urine cystatin-C concentration compared to those from casein [45]. In contrast, meat intake has been associated with increased ESRD incidence [46] and in the Singapore Chinese Health Study, where red meat intake was considered separately from other protein sources, red meat, but not fish, poultry, eggs, or dairy intake, was associated with greater incidence of ESRD [47]. Similar results were reported in the Atherosclerosis Risk in Communities (ARIC) study, where processed meats were considered as an additional, separate category and both red and processed meats were associated with incident ESRD [48]. The monosaccharide sugar fructose, typically found in high concentrations in fruits, has been implicated in renal damage. Indeed, dehydration-induced endogenous fructose production has been found to increase renal inflammation and fibrosis in animal models [49], and low fructose diets in individuals with CKD have been reported to reduce blood pressure and inflammation [50]. Such findings provide mechanistic plausibility for empirically observed associations between dietary patterns and renal health.
The findings of this study add further support to previous studies reporting associations between conceptually healthy diets and CKD risk and provide novel evidence for the association between dietary patterns and eGFR in British and Irish populations, for which there is limited data, independent of the effect of diet on diabetes risk, blood pressure and other potential confounding factors.
These analyses had several strengths. A large, population-based cohort enabled the generalisation of the findings, and unlike a number of previous studies which were limited in their ability to adjust for important confounding factors, the current study included a wide range of biological and lifestyle covariates. Dietary patterns and CKD prevalence vary by region [51, 52], and we have previously reported significant associations [26] between dietary patterns and renal function in a local population, using a more representative generalizable sample. The primary outcome variable was quantified using the CKD-EPI equation for both SCr and SCys, this equation is less affected by variations in muscle mass and diet and better predicts mortality than GFR estimated on SCr alone [53]. Examining dietary patterns instead of individual nutrients provides additional benefits for public health practice considering the interaction between dietary factors [54, 55], and the conceptually simpler public messaging for a healthy diet, although conversely fails to account for the effects of individual nutrients of interest. A posteriori dietary patterns derived specifically from a study population may also provide necessary context and relevance to regional cultures, increasing the applicability of the findings locally. Furthermore, a posteriori approaches used to identify the dietary patterns are not constrained by predetermined hypotheses that link nutrients with potential health outcomes.
The study design has several limitations. NICOLA has an inherent sample bias resulting from the recruitment of individuals aged 50 years and older. In addition, the sample excluded institutionalised individuals and those with dementia. Therefore, the generalisability of the study results may not extend to younger individuals, who may commonly adhere to other dietary patterns not identified in the current study, or to individuals with dementia in whom dietary habits may be profoundly affected. Longitudinal and experimental study designs could provide evidence of cause and effect but, at the time of this analysis, only cross-sectional data were available and so firm causal inferences cannot be drawn. Furthermore, dietary data were only captured at one time-point which may not reflect changes in dietary intakes. Direct measurement of glomerular filtration rate would provide an assessment of renal function with smaller inherent error than eGFR measures, however, eGFR was estimated using the clinically relevant CKD-EPI estimating equation and made use of the more accurate SCys and SCr-based measures which also better predicts complications associated with CKD [53, 56]. Moreover, renal function was estimated at a single time point. Although common practice in epidemiological studies, at an individual level this cannot account for diurnal and acute variations in renal function in the same way that the clinical practice of using two measures of eGFR taken at least three months apart can [5]. However, the large sample size minimises the probability of false null findings.
In summary, the findings of this study provide novel evidence for associations between culturally existing eating patterns and renal function, relevant to British and Irish populations, independent of the effect of diet on diabetes risk, blood pressure and other potential confounding factors. The results of this study will support diet-related primary prevention advice for CKD and inform future longitudinal analyses within the NICOLA.
Availability of data and materials
The data that support the findings of this study are available from the Northern Ireland Cohort for the Longitudinal Study of Ageing but restrictions apply to the availability of this data, which was used under license for the current study, and so is not publicly available. Data may, however, be made available from the corresponding authors upon reasonable request and provided there is permission from NICOLA.
References
van Horn L, Carson JA, Appel LJ, Burke LE, Economos C, Karmally W, Lancaster K, Lichtenstein AH, Johnson RK, Thomas RJ, Vos M, Wylie-Rosett J, Kris-Etherton P. American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council (2016) Recommended Dietary Pattern to Achieve Adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A Scientific Statement from the American Heart Association. Circulation 134(22):e505-e529
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B (2019) ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140(11):e596–e646. https://doi.org/10.1161/CIR.0000000000000678
Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, Cypress M, Faulkner P, Fischl AH, Francis T, Kolb LE, Lavin-Tompkins JM, MacLeod J, Maryniuk M, Mensing C, Orzeck EA, Pope DD, Pulizzi JL, Reed AA, Rhinehart AS, Siminerio L, Wang J (2017) Standards Revision Task Force. 2017 National Standards for Diabetes Self-Management Education and Support. Diab Care 40(10):1409-1419.
Evidence-based nutrition guidelines for the prevention and management of diabetes. Diabetes UK https://www.diabetes.org.uk/professionals/position-statements-reports/food-nutrition-lifestyle/evidence-based-nutrition-guidelines-for-the-prevention-and-management-of-diabetes
Kidney Disease: Improving Global Outcomes (KDIGO)(2013) CKD Work Group KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1-150
Lin J, Fung TT, Hu FB, Curhan GC (2011) Association of dietary patterns with albuminuria and kidney function decline in older white women: a subgroup analysis from the Nurses’ Health Study. Am J Kidney Dis 57:245–254
Lee HS, Lee KB, Hyun YY, Chang Y, Ryu S, Choi Y (2017) DASH dietary pattern and chronic kidney disease in elderly Korean adults. Eur J Clin Nutr 71(6):755–761
Rebholz CM, Crews DC, Grams ME, Steffen LM, Levey AS, Miller ER 3rd, Appel LJ, Coresh J (2016) DASH (Dietary Approaches to Stop Hypertension) Diet and risk of subsequent kidney disease. Am J Kidney Dis 68:853–861
Asghari G, Yuzbashian E, Mirmiran P, Azizi F (2017) The association between dietary approaches to stop hypertension and incidence of chronic kidney disease in adults: the Tehran Lipid and Glucose Study. Nephrol Dial Transpl 32:ii224–ii230
de Carvalho CM, Gross LA, de Azevedo MJ, Viana LV (2019) Dietary fiber intake (supplemental or dietary pattern rich in fiber) and diabetic kidney disease: A systematic review of clinical trials. Nutrients 11(2):347
Ajjarapu AS, Hinkle SN, Li M, Francis EC, Zhang C (2019) Dietary patterns and renal health outcomes in the general population: a review focusing on prospective studies. Nutrients 11(8):1877
Banerjee T, Crews DC, Tuot DS, Pavkov ME, Burrows NR, Stack AG, Saran R, Bragg-Gresham J, Powe NR., Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team (2019) Poor accordance to a DASH dietary pattern is associated with higher risk of ESRD among adults with moderate chronic kidney disease and hypertension. Kidney Int 95(1433):1442
Chrysohoou C, Panagiotakos DB, Pitsavos C, Skoumas J, Zeimbekis A, Kastorini CM, Stefanadis C (2010) Adherence to the Mediterranean diet is associated with renal function among healthy adults: The ATTICA Study. J Renal Nutr 20:176–184
Khatri M, Moon YP, Scarmeas N, Gu Y, Gardener H, Cheung K, Wright CB, Sacco RL, Nickolas TL, Elkind MS (2014) The association between a Mediterranean-style diet and kidney function in the Northern Manhattan Study Cohort. Clin J Am Soc Nephrol 9:1868–1875
Huang X, Jiménez-Moleón JJ, Lindholm B, Cederholm T, Arnlöv J, Risérus U, Sjögren P, Carrero JJ (2013) Mediterranean diet, kidney function, and mortality in men with CKD. Clin J Am Soc Nephrol 8(9):1548–1555
Asghari G, Farhadnejad H, Mirmiran P, Dizavi A, Yuzbashian E, Azizi F (2017) Adherence to the Mediterranean diet is associated with reduced risk of incident chronic kidney diseases among Tehranian adults. Hypertens Res 40:96–102
Bach KE, Kelly JT, Palmer SC, Khalesi S, Strippoli GFM, Campbell KL (2019) Healthy Dietary patterns and incidence of CKD: a meta-analysis of cohort studies. Clin J Am Soc Nephrol 14:1441–1449
Santin F, Canella D, Borges C, Lindholm B, Avesani CM (2019) Dietary patterns of patients with Chronic Kidney Disease: the influence of treatment modality. Nutrients 11(8):1920
Kurniawan AL, Hsu CY, Rau HH, Lin LY, Chao JC (2019) Association of kidney function-related dietary pattern, weight status, and cardiovascular risk factors with severity of impaired kidney function in middle-aged and older adults with chronic kidney disease: a cross-sectional population study. Nutr J 18(1):27
Mazaraki A, Tsioufis C, Dimitriadis K, Tsiachris D, Stefanadi E, Zampelas A, Richter D, Mariolis A, Panagiotakos D, Tousoulis D, Stefanadis C (2011) Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: data from the Leontio Lyceum ALbuminuria (3L study). Eur J Clin Nutr 65:219–225
Hu EA, Coresh J, Anderson CAM, Appel LJ, Grams ME, Crews DC, Mills KT, He J, Scialla J, Rahman M, Navaneethan SD, Lash JP, Ricardo AC, Feldman HI, Weir MR, Shou H, Rebholz CM, CRIC Study Investigators (2020) Adherence to healthy dietary patterns and risk of CKD progression and all-cause mortality: findings from the CRIC (Chronic Renal Insufficiency Cohort) Study. Am J Kidney Dis. https://doi.org/10.1053/j.ajkd.2020.04.019
Nettleton JA, Steffen LM, Palmas W, Burke GL, Jacobs DR (2008) Associations between microalbuminuria and animal foods, plant foods, and dietary patterns in the Multiethnic Study of Atherosclerosis. Am J Clin Nutr 87:1825–1836
Gutiérrez OM, Muntner P, Rizk DV, McClellan WM, Warnock DG, Newby PK, Judd SE (2014) Dietary patterns and risk of death and progression to ESRD in individuals with CKD: a cohort study. Am J Kidney Dis 64:204–213
Hsu CC, Jhang HR, Chang WT, Lin CH, Shin SJ, Hwang SJ, Huang MC (2014) Associations between dietary patterns and kidney function indicators in type 2 diabetes. Clin Nutr 33:98–105
Shi Z, Taylor AW, Riley M, Byles J, Liu J, Noakes M (2018) Association between dietary patterns, cadmium intake and chronic kidney disease among adults. Clin Nutr 37:276–284
Paterson EN, Neville CE, Silvestri G, Montgomery S, Moore E, Silvestri V, Cardwell CR, MacGillivray TJ, Maxwell AP, Woodside JV, McKay GJ (2018) Dietary patterns and chronic kidney disease: a cross-sectional association in the Irish Nun Eye Study. Sci Rep 8(1):6654
Shlipak MG, Katz R, Kestenbaum B, Fried LF, Newman AB, Siscovick DS, Stevens L, Sarnak MJ (2009) Rate of kidney function decline in older adults: a comparison using creatinine and cystatin C. Am J Nephrol 30:171–178
O’Neill RA, Maxwell AP, Kee F, Young I, McGuinness B, Hogg RE, McKay GJ (2020) Association of retinal venular tortuosity with impaired renal function in the Northern Ireland Cohort for the Longitudinal Study of Ageing. BMC Nephrol 21(1):382
Neville CE, McKinley MC, Kee F, Young IS, Cardwell CR, Woodside JV (2017) Validity of fruit and vegetable intake assessed by a food frequency questionnaire (FFQ) in older adults: the Northern Ireland Cohort for the Longitudinal Study of Aging (NICOLA). P Nutr Soc 76:OCE3
Food Standards Agency, Alison Mills, Sejal Patel & Helen Crawley. Food Portion Sizes. (Publisher TSO, 2005; ISBN10 0112429610)
Velioglu YS, Mazza G, Gao L, Oomah BD (1998) Antioxidant activity and total phenolics in selected fruits, vegetables, and grain products. J Agr Food Chem 46:4113–4117
Funakoshi Y, Omori H, Onoue A, Mihara S, Ogata Y, Katoh T (2012) Association between frequency of drinking alcohol and chronic kidney disease in men. Environ Health Prev 17:199–204
Schaeffner ES, Kurth T, de Jong PE, Glynn RJ, Buring JE, Gaziano JM (2005) Alcohol consumption and the risk of renal dysfunction in apparently healthy men. Arch Intern Med 165:1048–1053
Koning SH, Gansevoort RT, Mukamal KJ, Rimm EB, Bakker SJ, Joosten MM, PREVEND Study Group (2015) Alcohol consumption is inversely associated with the risk of developing chronic kidney disease. Kidney Int. 87(1009):1016
Matsumoto A, Nagasawa Y, Yamamoto R, Shinzawa M, Hasuike Y, Kuragano T, Isaka Y, Nakanishi T, Iseki K, Yamagata K, Tsuruya K, Yoshida H, Fujimoto S, Asahi K, Moriyama T, Watanabe T (2017) The association of alcohol and smoking with CKD in a Japanese nationwide cross-sectional survey. Hypertens Res 40:771–778
Strippoli GF, Craig JC, Rochtchina E, Flood VM, Wang JJ, Mitchell P (2011) Fluid and nutrient intake and risk of chronic kidney disease. Nephrology 16:326–334
Lotan Y, Daudon M, Bruyère F, Talaska G, Strippoli G, Johnson RJ, Tack I (2013) Impact of fluid intake in the prevention of urinary system diseases: a brief review. Curr Opin Nephrol Hypertens 22(S1):S1–S10
Roehrs M, Valentini J, Paniz C, Moro A, Charão M, Bulcão R, Freitas F, Brucker N, Duarte M, Leal M, Burg G, Grune T, Garcia SC (2011) The relationships between exogenous and endogenous antioxidants with the lipid profile and oxidative damage in hemodialysis patients. BMC Nephrol 12:59
Jun M, Venkataraman V, Razavian M, Cooper B, Zoungas S, Ninomiya T, Webster AC, Perkovic V (2012) Antioxidants for chronic kidney disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008176.pub2
Cao G, Sofic E, Prior RL (1996) Antioxidant capacity of tea and common vegetables. J Agr Food Chem 44:3426–3431
Zhu F, Du B, Xu B (2018) Anti-inflammatory effects of phytochemicals from fruits, vegetables, and food legumes: A review. Crit Rev Food Sci Nutr 58:1260–1270
Browne D, Williams MA, Maxwell AP, McGuinness B, Passmore P, Silvestri G, Woodside JV, McKay GJ (2019) Serum xanthophyll carotenoids are associated with estimated glomerular filtration rate in an aged cohort. Sci Rep 9(1):17068
Mirmiran P, Yuzbashian E, Asghari G, Sarverzadeh S, Azizi F (2018) Dietary fibre intake in relation to the risk of incident chronic kidney disease. Br J Nutr 119:479–485
Calder PC (2006) Polyunsaturated fatty acids and inflammation. Prostaglandins Leukot Essent Fatty Acids 75:197–202
Drotningsvik A, Midttun Ø, McCann A, Ueland PM, Høgøy I, Gudbrandsen OA (2018) Dietary intake of cod protein beneficially affects concentrations of urinary markers of kidney function and results in lower urinary loss of amino acids in obese Zucker fa/fa rats. Br J Nut 120:740–750
Motokawa M, Fukuda M, Muramatsu W, Sengo K, Kato N, Usami T, Yoshida A, Kimura G (2007) Regional differences in end-stage renal disease and amount of protein intake in Japan. J Renal Nutr 17:118–125
Lew QJ, Jafar TH, Koh HW, Jin A, Chow KY, Yuan JM, Koh WP (2017) Red meat intake and risk of ESRD. J Am Soc Nephrol 28:304–312
Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, Steffen LM, Rebholz CM (2017) Dietary protein sources and risk for incident chronic kidney disease: results from the Atherosclerosis Risk in Communities (ARIC) study. J Renal Nutr 27:233–242
Roncal Jimenez CA, Ishimoto T, Lanaspa MA, Rivard CJ, Nakagawa T, Ejaz AA, Cicerchi C, Inaba S, Le M, Miyazaki M, Glaser J, Correa-Rotter R, González MA, Aragón A, Wesseling C, Sánchez-Lozada LG, Johnson RJ (2014) Fructokinase activity mediates dehydration-induced renal injury. Kidney Int 86:294–302
Brymora A, Flisiński M, Johnson RJ, Goszka G, Stefańska A, Manitius J (2012) Low-fructose diet lowers blood pressure and inflammation in patients with chronic kidney disease. Nephrol Dial Transplant 27:608–612
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, Hobbs FD (2016) Global prevalence of Chronic Kidney Disease – a systematic review and meta-analysis. PLoS ONE 11:e0158765
USRDS (2020) United States Renal Data System Annual Report. USRDS. https://adr.usrds.org/2020/chronic-kidney-disease/1-ckd-in-the-general-population
Shlipak MG, Coresh J, Gansevoort RT (2013) Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med 369:932–943
Sacks FM, Obarzanek E, Windhauser MM, Svetkey LP, Vollmer WM, McCullough M, Karanja N, Lin PH, Steele P, Proschan MA et al (1995) Rationale and design of the Dietary Approaches to Stop Hypertension trial (DASH). Ann Epidemiol 5:108–118
Jacques PF, Tucker KL (2001) Are dietary patterns useful for understanding the role of diet in chronic disease? Am J Clin Nutr 73:1–2
Hsu C, Bansal N (2011) Measured GFR as “Gold Standard” - all that glitters is not gold? Clin J Am Soc Nephrol 6:1813–1814
Acknowledgements
We are grateful to all the participants of the NICOLA Study, and the whole NICOLA team, which includes nursing staff, research scientists, clerical staff, computer and laboratory technicians, managers and receptionists. The Atlantic Philanthropies, the Economic and Social Research Council, the UKCRC Centre of Excellence for Public Health Northern Ireland, the Centre for Ageing Research and Development in Ireland, the Office of the First Minister and Deputy First Minister, the Health and Social Care Research and Development Division of the Public Health Agency, the Wellcome Trust/Wolfson Foundation and Queen’s University Belfast provide core financial support for NICOLA. The authors alone are responsible for the interpretation of the data and any views or opinions presented are solely those of the authors and do not necessarily represent those of the NICOLA Study team.
Funding
Euan Paterson was supported by funding from the Northern Ireland Kidney Research Fund. This work was supported by the following funders who provide core financial support for the NICOLA Study: the Atlantic Philanthropies; the Economic and Social Research Council; the UKCRC Centre of Excellence for Public Health Northern Ireland; the Centre for Ageing Research and Development in Ireland; the Office of the First Minister and Deputy First Minister; the Health and Social Care Research and Development Division of the Public Health Agency; the Wellcome Trust/Wolfson Foundation; and Queen’s University Belfast.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Written informed consent was obtained from participants prior to taking part following ethical approval from the Queen’s University Belfast School Research Ethics Committee in compliance with the Declaration of Helsinki (SREC 12/23).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Paterson, E.N., Neville, C.E., Wallace, S.M. et al. Dietary patterns associated with renal impairment in the Northern Ireland Cohort for the Longitudinal Study of Ageing (NICOLA). Eur J Nutr 60, 4045–4054 (2021). https://doi.org/10.1007/s00394-021-02579-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02579-z