Abstract
Background
Non-obese patients with diabetes mellitus (DM) are becoming more prevalent, but their cardiovascular risk (CV) especially when accompanied with cardio-renal-metabolic co-morbidities (hypertension, chronic kidney disease, hyperlipidemia) is not well characterised. The aim of the study was to assess the CV risk among patients with DM in relation to obesity and cardio-renal-metabolic co-morbidities.
Materials and methods
This was a cohort study of all patients with DM without a history of major adverse cardiovascular event who were hospitalized for any reason in France in 2013 with at least 5 years of follow-up. They were categorized by the presence of obesity vs no obesity, as well as three cardio–renal–metabolic co-morbidities: hypertension, chronic kidney disease, hyperlipidemia. ‘Extremely unhealthy’ patients with DM were defined as those having all 3 co-morbidities.
Results
There were 196,112 patients (mean age 65.7 (SD 13.7) years; 54.3% males) included into the analysis. During a mean follow-up of 4.69 ± 1.79 years, when adjusted for multiple covariates, the non-obese and ‘extremely unhealthy’ obese patients had the highest risk of CV death [aHR 1.40 (95% CI, 1.22–1.61) and 1.48 (95% CI, 1.25–1.75), respectively]. The ‘extremely unhealthy’ obese had the highest risk of MACE-HF [aHR 1.84 (95% CI, 1.72–1.97)] and new-onset AF [aHR 1.64 (95% CI, 1.47–1.83)].
Conclusion
Both non-obese and obese patients with DM with associated cardio-renal-metabolic co-morbidities are an ‘extremely unhealthy’ phenotype with the highest risk of CV death and CV events.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decades, cardiovascular disease (CVD) risk is increased in obese patients with diabetes mellitus (DM) [1]. However, nowadays, there is an increasing prevalence of type 2 DM (T2DM) with lean/normal body mass index (BMI), which was for decades thought to be the minority of patients with DM [2]. In a recent study from the United States, ‘lean’ populations showed an approximately ninefold higher growth in the prevalence of DM over the last 5 years, when compared with overweight/obese populations [3]. Indeed, the metabolically obese normal weight (MONW) phenotype was first described more than 40 years ago [4], yet T2DM with normal weight remains an understudied DM phenotype.
There is the so-called ‘obesity paradox’ indicating that there is reduced mortality or incidence of CV events in patients with obesity comparing to the ones who are not obese [5,6,7,8]. The obesity paradox may be present in patients with DM [9,10,11,12,13], but not all the studies have reported the same outcomes [14, 15]. However, the impact of obesity in DM may not be binary (i.e. yes/no), given the comorbidities associated with DM. Indeed, the contradictory results in relation to the obesity paradox in patients with DM may be linked to different populations studied and those with and without coronary artery disease. In addition, the CV risk in obesity vs no obesity may be intimately linked to cardio-renal-metabolic co-morbidities i.e. hypertension, chronic kidney disease (CKD) and hyperlipidemia.
In this longitudinal nationwide French cohort study, we aimed to evaluate CV risks in patients with DM in relation to the presence of obesity vs no obesity, as well as the presence of one or more concomitant cardio-renal-metabolic co-morbidities.
Research design and methods
Study design
This was a longitudinal cohort study based on the database of national hospitalization which covered hospital care for the entire French population. The details of this study population was described elsewhere [16]. In brief, the data was collected from the national administrative Programme de Médicalisation des Systèmes d’Information (PMSI) for all patients admitted to French hospitals for any reason in the year 2013 with at least 5 years of complete follow-up (unless death). The following data has been collected: demographics, diabetes mellitus (DM), obesity and any other co-morbidities, medical history and events during hospitalization and follow up. Each diagnosis was identified with International Classification of Diseases tenth revision (ICD-10) codes. Diabetes was identified with the following ICD-10 codes: E10 for diabetes type 1 (T1DM), E11 for diabetes type 2 (T2DM), E13 and E14 for other types of DM, and obesity was identified with ICD-10 code E65. Exclusion criteria were as follows: age < 18 years, previous hospitalization for myocardial infarction (MI), ischemic stroke (IS) or new-onset HF (major adverse cardiac event [MACE]-HF) as well as atrial fibrillation (AF) recorded during 2010–2013, or underweight and malnutrition (identified with the following ICD-10 codes: E41, E43, E44, E46, F50.8, K91.2 and R63.6), and those without DM.
Cardio-reno-metabolic phenotypes
We divided the cohort into eight groups depending on the presence of obese/non-obese phenotype, and the number of cardio-renal-metabolic comorbidities defined as hypertension (HA) and/or CKD and/or hyperlipidemia with their respective ICD-10 codes (Supplementary Table 1). CKD was incorporated as a cardio-renal-metabolic comorbidity alongside hypertension and hyperlipidemia, to offer a comprehensive understanding of CV risks. This inclusion is predicated on CKD being considered a modifiable risk factor, as its progression and associated CV risks can be mitigated through targeted pharmacological interventions. Group 1, group 2 and group 3 consisted of non-obese patients with DM and zero, one or two other cardio-reno-metabolic comorbidities (ie. hypertension, CKD, hyperlipidemia) respectively; Group 4 was categorised as “non-obese extremely unhealthy” consisting of non-obese patients with DM and 3 additional cardio–renal–metabolic co-morbidities. Group 5, group 6 and group 7 consisted of patients with obesity, DM and 0, 1 or 2 other cardio-renal-metabolic co-morbidities respectively. Group 8 were “extremely unhealthy obese” consisting of obese patients with DM plus 3 additional cardio-reno-metabolic comorbidities.
Outcomes
The primary outcome was the occurrence of all-cause death, MACE-HF (CV death, MI, IS, new-onset HF) and new-onset AF during follow up. We identified these outcomes with their respective ICD-10 codes. The patients were followed from the first hospitalization in 2013 till 31 December 2019 or until death.
Information on outcomes during the follow-up was obtained by analyzing the PMSI codes for each patient. The mode of death (CV or non-CV) was identified based on the main diagnosis during hospitalization resulting in in-hospital death. Patients were also analyzed according to number of cardio–renal–metabolic comorbidities namely patients with zero additional abnormalities were those with DM (obese or non-obese) excluding hypertension, CKD and hyperlipidemia after which, we investigated DM patients with 1, 2 or 3 additional comorbidities.
Ethics
The medical information used in the database was anonymized, and the analysis was conducted retrospectively. Therefore, neither patient consent nor ethics committee approval was required for this study. The study was however approved by the institutional review board of the Pole Coeur Thorax Vaisseaux from the Trousseau University Hospital (Tours, France) on 1 December 2015, and registered as a clinical audit. The French Data Protection Authority granted access to the PMSI data. Moreover, procedures for data collection and management were approved by the Commission Nationale de lʼInformatique et des Libertés (CNIL), the independent National Ethical Committee protecting human rights in France, which ensures that all information is kept confidential and anonymous, in compliance with the Declaration of Helsinki (authorization number 1897139).
Statistical analysis
Qualitative variables are presented as frequency and percentages and quantitative variables as means (standard deviations [SDs]). Comparisons were made using chi-square tests for categorical variables and Studentʼs t test for continuous variables. Incidence rates (IRs) with 95% confidence interval (95% CI) were calculated for outcomes of interest in each of four subgroups. A multivariable analysis for clinical outcomes during the whole follow-up in each subgroup was performed using a Cox regression model to calculate the adjusted hazard ratio (aHR) and 95% CI for each subgroup, the reference category were individuals with DM and normal weight (zero additional cardiorenal–metabolic comorbidities). In the first model we adjusted for age at baseline and sex, while in the second model we adjusted for the following variables: age, sex, type of diabetes, smoking status, alcohol-related diagnoses, valve disease, coronary artery disease, previous percutaneous coronary intervention, previous coronary artery bypass grafting, vascular disease, previous pacemaker or implantable cardioverter defibrillator, lung disease, sleep apnoea syndrome, liver disease, thyroid disease, inflammatory disease, anaemia, previous cancer, cognitive impairment and illicit drug use. Kaplan–Meier curves were plotted with the duration from the enrollment to either the last follow-up date or occurrence of outcome of interest. All analyses were performed with STATA version 16.1 (Stata Corp., College Station, TX, USA).
Results
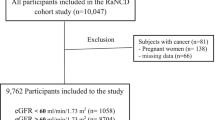
Of 3,381,472 patients hospitalized in France in the year 2013 we included 341,049 patients who had DM in this analysis. Subsequently, we excluded those with previous MACE-HF (112,905 patients), previous AF (59,812 patients) and underweight or under nutrient (12,475 patients). We finally included 196,112 patients (mean age 65.7 (13.7) years; 54.3% male) (Fig. 1).
Among these individuals, 138,350 (70.5%) were classified as non-obese and 57,762 (29.5%) as obese subjects. Population characteristics at baseline showed significant differences across all compared features between eight subgroups of individuals with obesity or no obesity, based on the number of cardio–renal–metabolic comorbidities (Table 1). Those with more CV comorbidities were older, with higher proportion of males and higher rate of non-metabolic comorbidities than those without.
Mortality and CV outcomes
During a mean follow-up of 4.69 ± 1.79 years (median [IQR]: 5.47[4.74–5.82]) 61,787 (31.5%) patients died, including 10,981 (5.6) who died due to CV causes (Supplementary Table S4). The highest incidence of all-cause death and CV death, IS and MI was observed for the group of non-obese patients with three comorbidities (10.2%, 2.5%, 3.4%, 2.8% respectively). Both patients with obesity as well as those without obesity — but with 3 concomitant cardio-renal-metabolic abnormalities presented with the highest incidence of MACE-HF (16.5% and 16.2%) and new-onset AF (5.4% and 5.4%).
Obese patients with no additional cardio-renal-metabolic comorbidities besides DM had the lowest incidences of all-cause death, CV death, MACE-HF and AF (3.9%; 0.6%; 4.6% and 2.1%, respectively), even lower than non-obese without metabolic comorbidities (6.2%; 0.9%; 5.8% and 2.4%). Incidence rates per patient-year of major adverse events are presented in Table 2 with corresponding Kaplan–Meier survival curves shown in Fig. 2 (all Log-rank < 0.0001).
Kaplan–Meier curves of all cause-death (A), CV death (B), MACE-HF (C), and new-onset AF (D). Log rank p values all < 0.0001. AF atrial fibrillation, CRM cardio-renal-metabolic, CV cardiovascular, MACE-HF composite of cardiovascular death, ischemic stroke, myocardial infarction and new-onset heart failure
When stratified by sex, risk of all-cause death and CV death was higher among non-obese, regardless of sex. Conversely, for the MACE-HF and new AF, patient’s sex was of greater importance than the obesity status, with males having higher risk of these outcomes. Kaplan–Meier survival curves detailing these findings are available in Supplementary Figure S2.
Multivariate analysis
When adjusted for age and sex, both non-obese and obese extremely unhealthy patients had the highest risk of all-cause death with aHRs of 1.12 (95% CI, 1.05–1.19) and 1.12 (95% CI, 1.04–1.20) respectively; CV death with aHRs of 1.75 (95% CI, 1.54–1.99) and 1.89 (95% CI, 1.62–2.19), respectively; and HF with aHRs of 2.13 (95% CI, 2.00–2.27) and 2.66 (95% CI, 2.49–2.84), respectively (Supplementary Figure S3).
Similarly, the risk of stroke and MI (both as a component of MACE-HF), were the highest in the obese extremely unhealthy patients with aHRs of 1.53 (95% CI, 1.29–1.82) and 1.45 (95% CI, 1.24–1.68), respectively (Supplementary Figure S4). In the obese and non- obese extremely unhealthy patients, aHRs were 1.94 (95% CI 1.68–2.25) and 2.15 (95% CI 1.90–2.44), respectively. The risk of MACE-HF, and new-onset AF were the highest in extremely unhealthy obese patients with aHRs of 2.42 (95% CI, 2.28–2.58) and 1.98 (95% CI, 1.80–2.18), respectively.
After further adjustment for multiple covariates (see description of Fig. 3), both non-obese and obese extremely unhealthy patients still had the highest risk of CV death with aHRs of 1.40 (95% CI, 1.22–1.61) and 1.48 (95% CI, 1.26–1.75), respectively, and MACE-HF with aHRs of 1.56 (95% CI, 1.47–1.66) and 1.84 (95% CI, 1.72–1.97), respectively. Obese extremely unhealthy patients had the highest risk of incident AF with aHRs of 1.64 (95% CI, 1.47–1.83).
Adjusted hazard ratios for the associations between body size phenotypes and cardio-renal-metabolic comorbidities for all cause-death CV death, MACE-HF, and new-onset AF. Adjustment was made for age, sex, type of diabetes, smoking status, alcohol-related diagnoses, valve disease, coronary artery disease, previous PCI, previous CABG, vascular disease, previous pacemaker or ICD, lung disease, sleep apnoea syndrome, liver disease, thyroid disease, inflammatory disease, anaemia, previous cancer, cognitive impairment and illicit drug uses. AF atrial fibrillation, aHR adjusted hazard ratio, CABG coronary artery bypass grafting, CI confidence interval, CRM cardio-renal-metabolic, CV cardiovascular, ICD Implantable cardioverter defibrillator, MACE-HF composite of CV death, ischemic stroke, myocardial infarction and new-onset heart failure, PCI Percutaneous coronary intervention, ref. reference
Discussion
In the present study using data that were representative for the contemporary French national population, our principal findings are as follows: (i) approx. 70% of DM patients were non-obese; (ii) the highest incidence rate of all cause and CV- death as well as IS and MI was for non-obese, extremely unhealthy group (presenting with 3 cardio-renal-metabolic comorbidities); (iii) the highest incidence of MACE-HF, HF and AF was for both non-obese and obese, extremely unhealthy patients; (iv) the highest adjusted risk of CV- death and MACE-HF were for both non-obese and obese extremely unhealthy patients; and (v) the highest adjusted risk of new AF were for extremely unhealthy obese patients.
Epidemiological data related to obesity prevalence in DM are changing and the numbers are lowering nowadays when compared the data from other countries reported 17 years ago (approx. 50–60%) [17, 18]. For example, in a recent population study from France published in 2023, 788 (41.1%) of patients with known DM were obese [19]. In the present cohort of French patients with DM, the prevalence of obesity was only approx. 30%.
Our data show that non-obese patients with DM were commonly burdened with other cardio–renal–metabolic comorbidities (i.e. hypertension, CKD, hyperlipidemia), consistent with prior French National general population data (i.e. not focused solely on patients with DM) [16]. In everyday clinical scenario, DM itself is often related to other chronic comorbidities with the increasing prevalence of multimorbidity, defined as having two or more long-term conditions [20], especially cardiac, renal and metabolic diseases [21]. DM as well as obesity confers higher CV risk but neither diabetes nor obesity per se are “yes/no” diagnoses in term of CV health where not every patient who has diabetes or obesity presents the same CV risk [22].
There is ongoing controversy whether the obesity paradox exists in DM (9–13) or not [14, 15]. We found that the highest incidence of all-cause and CV- death as well as IS and MI was observed among patients without obesity, but this was linked to being burdened with 3 concomitant cardio–renal–metabolic abnormalities (which we termed an ‘extremely unhealthy’ phenotype). Those who were obese but had no additional comorbidities besides DM had the lowest incidence rate of these outcomes. While these findings might initially appear to support the obesity paradox, this does not reflect long-term health outcomes. Indeed, prior research indicates that obese individuals may have a lower overall life expectancy compared to their leaner counterparts [23, 24]. In addition, short-term follow-up may favor younger, obese patients with fewer immediate comorbidities, yielding more favorable prognosis. Subsequent adjustments for various comorbidities negated any significant difference in all-cause death and CV death risk between obese and non-obese individuals within the ‘extremely unhealthy’ category, with the obese having higher risk of MACE-HF.
Another explanation for the obesity paradox could be that lower body weight in the presence of cardio-renal-metabolic disorders which are to some extent obesity-related may reflect underlying illness that contributes to adverse cardiovascular events. Moreover one of the chronic conditions which was twice more prevalent in the extremely unhealthy phenotype of patients with DM was CKD, which is a well-recognized predictor of increased CV risk per se [25, 26]. When adjusted for age and sex, the extremely unhealthy DM patients, both with and without obesity, presented with higher risks of all cause death, CV- death, HF, IS and MI. The importance of associated comorbidities has been highlighted by Lassale et al. where metabolically unhealthy patients were associated with higher coronary heart disease risk than healthy people, irrespective of their BMI [27].
Obesity however still seems to be an important risk factor for MACE-HF and incident AF because as shown in the current analysis, an obese, extremely unhealthy phenotype was independently associated with the highest risk of these outcomes. Previously obese patients with DM had already been assessed as a group with the highest risk of AF incidence [28, 29]. Non-obese patients were not found to be at increased risk of AF compared to the obese ones, but contrary to our study no comorbidity has been taken into account [29].What is more, obese patients, comparing to non-obese ones, were more burdened with obstructive sleep apnoea syndrome which is one of acknowledged risk factors of poor CV prognosis [30, 31]. The present results draw attention to a group of patients with DM, both obese and non-obese but with additional cardio-renal-metabolic co-morbidities, and an extremely unhealthy phenotype resulting in an increased CV risk.
In our cohort, sex played a differential role in all studied outcomes. While obesity status influenced all-cause and cardiovascular death across both sexes with non-obese individuals being at higher risk of all-cause and CV death, it was less impactful than sex in relation to MACE-HF and new-onset AF. This finding confirms previously observed attenuation of gender differences in cardiovascular mortality [32] but does not explain the higher CV risk among non-obese individuals which definitely needs further investigation. This layered interaction between obesity and sex is further complicated when considering other data. A Norwegian longitudinal study reported that even though men had higher rates of incident AF similarly to our study, the influence of BMI was comparable between sexes with the lowest risk of AF among those with normal weight [33, 34]. Meanwhile, the ACCORD trial indicated a sex-BMI interaction among patients with diabetes, with higher BMI conferring a greater risk of incident AF for men [35].These multifaceted observations collectively accentuate the complex interplay between BMI, diabetes status, and sex in influencing long-term cardiovascular outcomes.
Our study confirms the importance of managing cardio–renal–metabolic status of patients with DM regardless of obesity and proves that cardio–renal–metabolic status modifies the relationship between patients’ body mass related phenotype and risk of CV events. Given that many patients with DM have associated comorbidities and lifestyle factors that should be addressed, this has also led to the evolution of more holistic or integrated multidisciplinary management approaches to improve patient care [36].
Limitations
This study had several limitations that should be addressed. It was observational in nature and based on administrative data with potential biases related to the study methodology. We based the outcomes on diagnoses obtained from ICD-10 codes so we cannot exclude inaccuracies in the diagnostic codes. On the other hand, disease coding is related to reimbursement that is why it is regularly controlled and expected to be of good quality. The large scale of the presented study may however partly compensate for some of the potential biases. Our statistical adjustments were made for numerous variables, however important for patients with DM confounders, namely recent weight change, abdominal obesity, duration and severity of diabetes could not be assessed due to administrative nature of the database. In addition, the absence of laboratory data in our study precludes the stratification of patients by CKD stage, a variable that could offer additional insights into the relationship between renal function and the outcomes observed. Due to the study design based on the ICD-10 codes we had no information related to overweight patients and so we compared only those who were obese to those who were not obese, although a proportion of the latter could be overweight. Moreover, obesity was defined based on BMI which does not fully capture body composition, especially abdominal distribution of body fat. Also, age-related loss of lean muscle mass and bone (sarcopenia) could be the reason for lower body weight especially in older adults.
Conclusion
Obese and non-obese patients with DM and three concomitant cardio-renal-metabolic co-morbidities are an ‘extremely unhealthy’ phenotype with the highest adjusted risk of CV death as well as MACE-HF. Focus should be not only be on diabetes or obesity as a single disease but attention at managing any concomitant comorbidities associated with them.
Data availability
Access to the PMSI (the French hospitalization database) is controlled by the CNIL, the independent national ethics committee protecting human rights in France. Due to the sensitive nature of the database, data sharing is not authorized according to the French legislation.
References
Ridderstråle M, Gudbjörnsdottir S, Eliasson B, Nilsson PM, Cederholm J (2006) Obesity and cardiovascular risk factors in type 2 diabetes: results from the Swedish National Diabetes Register. J Intern Med 259(3):314–322
Wu J, Feng Z, Duan J, Li Y, Deng P, Wang J et al (2023) Global burden of type 2 diabetes attributable to non-high body mass index from 1990 to 2019. BMC Public Health 23(1):1338
Adesoba TP, Brown CC (2023) Trends in the Prevalence of Lean Diabetes Among U.S. Adults, 2015–2020. Diabetes Care. 46(4):885–9
Ruderman NB, Schneider SH, Berchtold P (1981) The, “metabolically-obese”, normal-weight individual. Am J Clin Nutr 34(8):1617–1621
Luis G, Weissman NJ, Ron W, Shmuel F, Regina D, Ellen PE et al (2002) The impact of obesity on the short-term andlong-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 39(4):578–84
Uretsky S, Messerli FH, Bangalore S, Champion A, Cooper-DeHoff RM, Zhou Q et al (2007) Obesity paradox in patients with hypertension and coronary artery disease. Am J Med 120(10):863–870
Hainer V, Aldhoon-Hainerová I (2013) Obesity paradox does exist. Diabetes Care. 36(Suppl 2):S276–S281
Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE et al (2002) The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol 39(4):578–584
Carnethon MR, De Chavez PJD, Biggs ML, Lewis CE, Pankow JS, Bertoni AG et al (2012) Association of weight status with mortality in adults with incident diabetes. JAMA 308(6):581–590
Logue J, Walker JJ, Leese G, Lindsay R, McKnight J, Morris A et al (2013) Association between BMI measured within a year after diagnosis of type 2 diabetes and mortality. Diabetes Care 36(4):887–893
Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Li W, Johnson J et al (2014) Body mass index and the risk of all-cause mortality among patients with type 2 diabetes mellitus. Circulation 130(24):2143–2151
Tsujimoto T, Kajio H, Sugiyama T (2016) Risks for cardiovascular and cardiac deaths in nonobese patients with diabetes and coronary heart disease. Mayo Clin Proc 91(11):1545–1554
Thomas G, Khunti K, Curcin V, Molokhia M, Millett C, Majeed A et al (2014) Obesity paradox in people newly diagnosed with type 2 diabetes with and without prior cardiovascular disease. Diabetes Obes Metab 16(4):317–325
Tobias DK, Pan A, Jackson CL, O’Reilly EJ, Ding EL, Willett WC et al (2014) Body-mass index and mortality among adults with incident type 2 diabetes. N Engl J Med 370(3):233–244
Costanzo P, Cleland JGF, Pellicori P, Clark AL, Hepburn D, Kilpatrick ES et al (2015) The obesity paradox in type 2 diabetes mellitus: relationship of body mass index to prognosis a cohort study. Ann Intern Med 162(9):610–618
Fauchier G, Bisson A, Bodin A, Herbert J, Semaan C, Angoulvant D et al (2021) Metabolically healthy obesity and cardiovascular events: a nationwide cohort study. Diabetes Obes Metab 23(11):2492–2501
Thomas MC, Zimmet P, Shaw JE (2006) Identification of obesity in patients with type 2 diabetes from Australian primary care: the NEFRON-5 study. Diabetes Care 29(12):2723–2725
Daousi C, Casson IF, Gill GV, MacFarlane IA, Wilding JPH, Pinkney JH (2006) Prevalence of obesity in type 2 diabetes in secondary care: association with cardiovascular risk factors. Postgrad Med J 82(966):280–284
Hauguel-Moreau M, Hergault H, Cazabat L, Pépin M, Beauchet A, Aïdan V et al (2023) Prevalence of prediabetes and undiagnosed diabetes in a large urban middle-aged population: the CARVAR 92 cohort. Cardiovasc Diabetol 22(1):31
Diederichs C, Berger K, Bartels DB (2011) The measurement of multiple chronic diseases–a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci 66(3):301–311
Arnold SV, Kosiborod M, Wang J, Fenici P, Gannedahl G, LoCasale RJ (2018) Burden of cardio-renal-metabolic conditions in adults with type 2 diabetes within the Diabetes Collaborative Registry. Diabetes Obes Metab 20(8):2000–2003
Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, et al (2015) Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1 9 million people. Lancet Diabetes Endocrinol 3(2):105–113
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L et al (2003) Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 138(1):24–32
Vidra N, Trias-Llimós S, Janssen F (2019) Impact of obesity on life expectancy among different European countries: secondary analysis of population-level data over the 1975–2012 period. BMJ Open 9(7):e028086
Weiner DE, Tabatabai S, Tighiouart H, Elsayed E, Bansal N, Griffith J et al (2006) Cardiovascular outcomes and all-cause mortality: exploring the interaction between CKD and cardiovascular disease. Am J Kidney Dis Off J Natl Kidney Found 48(3):392–401
Matsushita K, Ballew SH, Wang AY-M, Kalyesubula R, Schaeffner E, Agarwal R (2022) Epidemiology and risk of cardiovascular disease in populations with chronic kidney disease. Nat Rev Nephrol 18(11):696–707
Lassale C, Tzoulaki I, Moons KGM, Sweeting M, Boer J, Johnson L et al (2018) Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur Heart J 39(5):397–406
Kim YG, Han K-D, Choi J-I, Boo KY, Kim DY, Oh S-K et al (2019) The impact of body weight and diabetes on new-onset atrial fibrillation: a nationwide population based study. Cardiovasc Diabetol 18(1):128
Dublin S, Glazer NL, Smith NL, Psaty BM, Lumley T, Wiggins KL et al (2010) Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J Gen Intern Med 25(8):853–858
Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE et al (2004) Association of atrial fibrillation and obstructive sleep apnea. Circulation 110(4):364–367
Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N et al (2021) Obstructive sleep apnea and cardiovascular disease: a scientific statement from the american heart association. Circulation 144(3):e56–e67
Song X, Tabák AG, Zethelius B, Yudkin JS, Söderberg S, Laatikainen T et al (2014) Obesity attenuates gender differences in cardiovascular mortality. Cardiovasc Diabetol 13(1):144
Ball J, Løchen M-L, Wilsgaard T, Schirmer H, Hopstock LA, Morseth B, et al. sex differences in the impact of body mass index on the risk of future atrial fibrillation: insights from the longitudinal population-based tromsø study
Malmborg M, Schmiegelow MDS, Nørgaard CH, Munch A, Gerds T, Schou M et al (2020) Does type 2 diabetes confer higher relative rates of cardiovascular events in women compared with men? Eur Heart J 41(13):1346–1353
Singleton MJ, German CA, Soliman EZ, Whalen SP, Bhave PD, Bertoni AG et al (2020) Body mass index, sex, and incident atrial fibrillation in diabetes: The ACCORD trial. Clin Electrophysiol 6(13):1713–1720
Field M, Kuduvalli M, Torella F, McKay V, Khalatbari A, Lip GYH (2022) Integrated care systems and the aortovascular hub. Thromb Haemost 122(2):177–180
Funding
None.
Author information
Authors and Affiliations
Contributions
KN, AB, GYHL: substantial contribution to the conception and design of the work; AB, LF: prepared the dataset for statistical analysis; KN, AB, GYHL: conceptualization of data analysis; AB: data analysis; KN, AB, KI: visualization of the results, preparation of the tables and figures; KN, AB, KI: drafted the manuscript; GF, PHD, GYHL, LF: substantively revised the work; KN, AB, KI, GF, PHD, GYHL, LF: review & editing of the original draft. AB, LF are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All of the authors have read and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Katarzyna Nabrdalik and Arnaud Bisson are Joint first authors.
Henri Ducluzeau, Gregory Y. H. Lip and Laurent Fauchier are Joint senior authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nabrdalik, K., Bisson, A., Irlik, K. et al. Metabolically ‘extremely unhealthy’ obese and non-obese patients with diabetes and the risk of cardiovascular events: a French nationwide cohort study. Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02344-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-023-02344-8