Abstract
Purpose
Recent studies have reported alarming appendiceal tumor rates associated with complicated acute appendicitis, especially in patients presenting with a periappendicular abscess. However, the data on histology of appendiceal tumors among acute appendicitis patients is limited, especially in patient cohorts differentiating between uncomplicated and complicated acute appendicitis. We have previously reported the association of increased appendiceal tumor prevalence with complicated acute appendicitis in this population-based study. The objective of this secondary analysis was to evaluate the association of both appendicitis severity and patient age with appendiceal tumor histology.
Methods
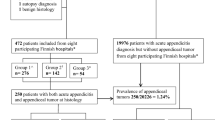
This nationwide population-based registry study (The Finnish Cancer Registry) was conducted from 2007 to 2013. All appendiceal tumors (n = 840) and available medical reports (n = 504) of these patients at eight study hospitals were previously evaluated, identifying altogether 250 patients with both acute appendicitis and appendiceal tumor.
Results
The severity of acute appendicitis was significantly associated with more malignant tumor histology. The risk of adenocarcinoma or pseudomyxoma was significantly higher among patients with periappendicular abscess (OR 15.05, CI 95% 6.98–32.49, p < 0.001) and patients presenting with perforated acute appendicitis (OR 4.09, CI 95% 1.69–9.90, p = 0.0018) compared to patients with uncomplicated acute appendicitis. Similarly, patient age over 40 years was significantly associated with the risk of adenocarcinoma and pseudomyxoma (OR 26.46, Cl 95% 7.95–88.09, p < 0.001). Patient sex was not associated with a more malignant appendiceal tumor histology (p = 0.67).
Conclusion
More malignant appendiceal tumor histology of adenocarcinoma or pseudomyxoma was significantly associated with patient age over 40 years and complicated acute appendicitis, especially periappendicular abscess.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis occurs in 7–12% of the general population, and appendectomy is one of the most common indications for emergency abdominal surgery [1,2,3]. Uncomplicated and complicated acute appendicitis seems to follow different epidemiological and clinical patterns, also suggesting potentially different pathophysiology behind these two different forms of appendicitis severity [2, 3]. In computed tomography (CT) confirmed uncomplicated acute appendicitis, antibiotic therapy has been proven to be safe, efficient, and feasible both at short- and long-term follow-up [4,5,6,7]. Uncomplicated acute appendicitis may even resolve with only symptomatic treatment [8, 9], and the over century-old treatment paradigm of appendectomy for all may not be necessary for the majority of patients with CT confirmed uncomplicated acute appendicitis [4,5,6,7,8,9]. Approximately 25 to 35% of acute appendicitis cases present as complicated [3]. Acute appendicitis presenting with gangrene, perforation, periappendicular abscess, or tumor has been traditionally considered complicated acute appendicitis usually requiring emergency appendectomy. In addition, the presence of an appendicolith has been shown to be associated with a more complicated course of acute appendicitis [7, 10]. CT is the gold standard in diagnosing acute appendicitis also able to quite accurately differentiate between uncomplicated and complicated acute appendicitis [11,12,13]. In 3 to 10% of patients, complicated appendicitis presents as a closed, circumscribed periappendicular abscess [14,15,16].
Management of periappendicular abscess usually involves the initial nonoperative treatment with antibiotics and drainage (if necessary), followed by interval appendectomy. Previously the rationale for promoting interval appendectomy has been the prevention of recurrent appendicitis, but the reported recurrence risk after initial successful nonoperative management of periappendicular abscess is quite low, varying between 5 and 20% [14,15,16]. The reported overall risk of an underlying malignant neoplasm in acute appendicitis is very low, varying between 0.7 and 3% [17,18,19,20,21]. However, there are many recent studies reporting an alarming rate of appendiceal neoplasms detected at interval appendectomy in patients with previous periappendicular abscess [22,23,24,25,26,27]. A recent randomized controlled trial comparing interval appendectomy to follow-up with magnetic resonance imaging in patients with initial successful antibiotic treatment of periappendicular abscess was prematurely terminated based on high tumor rate in the interval appendectomy group with an overall appendiceal neoplasm incidence of 20% (12 of 60), and all of these patients were over 40 years of age [24].
The World Health Organisation (WHO) classifies appendiceal tumors in two main groups: neuroendocrine tumors (NETs) [28, 29] and appendiceal carcinomas (colonic-type and mucinous-type) [30] ranging from NET 5-year survival rate of 100% for a localized and 85–100% for a regional disease [31] to 5-year survival of 40–75% of mixed type NETs (MANECs, mixed adeno-neuroendocrine carcinomas) [30, 32, 33] and goblet cell carcinomas and to the 5-year survival of 48–58% of colonic-type appendiceal adenocarcinomas [34, 35]. The 2010 WHO classification also recognizes three main categories of mucinous neoplasms: mucinous adenoma, low-grade appendiceal mucinous neoplasm (LAMN), and mucinous adenocarcinoma. Although mucinous tumors are considered to be benign, these appendiceal neoplasms can progress to peritoneal dissemination resulting in the condition defined as pseudomyxoma peritonei.
Data on the association of appendicitis severity with appendiceal neoplasm incidence is limited. To our knowledge, there are no population-based registry studies published on the tumor histology association with appendicitis severity. We have previously reported the association of appendiceal neoplasm risk with complicated acute appendicitis in this population-based study [36]. The objective of this secondary analysis was to evaluate the association of appendiceal tumor histology with both the severity of acute appendicitis and patient age and sex.
Methods
The study design, rationale, and methods for this nationwide population-based registry study have been previously reported [36]. Briefly, all appendiceal tumors in Finland during 2007–2013 were collected from the Finnish Cancer Registry (FCR), maintaining a nationwide database on all cancer cases in Finland. From this patient population of histologically proven appendiceal primary tumors, we collected hospital medical record data on patients treated at eight study hospitals: all five university hospitals (Turku, Helsinki, Tampere, Oulu, and Kuopio) and three larger central hospitals (Jyväskylä, Lahti, and Mikkeli) representing 70% of the whole population in Finland. This secondary analysis focused on evaluating detailed appendiceal tumor histology association with appendicitis severity and patient demographics of age and sex. Patients were divided into three groups based on the appendiceal neoplasm histology: group 1 NETs, group 2 MANECs and goblet cell carcinomas, and group 3 adenocarcinomas and pseudomyxomas (including mucinous adenoma, low-grade appendiceal mucinous neoplasm (LAMN), and mucinous adenocarcinoma). Diagnoses were classified according to the WHO International Classification of Disease year 2010 classification (ICD-10). This study was approved by the Turku University Hospital ethical committee.
Statistical methods
The data were presented as means with standard deviation (SD) for continuous variables (age) and counts with percentage for categorical variables (sex). The differences in background variables between the three groups (uncomplicated acute appendicitis vs perforated acute appendicitis vs periappendicular abscess) were tested for a numeric variable with one-way analysis of variance and for categorical variables using the chi-square test (Tables 1 and 2). Fisher’s exact test was used if the variable had low group frequencies.
The association between appendiceal tumor histology and the severity of acute appendicitis, sex, and age of the patient was examined using multinomial logistic regression. Age was also examined as a categorical variable (under 40 years vs 40 years and older). The explanatory factors were first modeled separately and then together in the same model. The level of significance was set at a p-value < 0.05. All of the statistical analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA).
Results
As previously reported [36], there were altogether 250 patients with available diagnostic and clinical data included in this study with both acute appendicitis and appendiceal tumor based on both surgical findings and histology (Fig. 1). Out of these, 148 (59%) had uncomplicated and 102 (41%) complicated acute appendicitis, with the latter group consisting of 36 patients with perforation and 66 patients with a periappendiceal abscess. Detailed patient characteristics of the study population are presented in Table 1. The majority of the patients (86%, 215/250) underwent emergency surgery, with the majority of patients (66%, 142/215) ending up with a diagnosis of uncomplicated acute appendicitis at histopathology in addition to the tumor. The main primary operation was laparoscopic or open appendectomy (91%, 229/250) regardless of the severity of appendicitis. There were altogether 35 elective operations, and 85% (29/35) of these were performed to patients presenting with a periappendicular abscess: 74% (26/35) of all elective operations were interval appendectomies, 11% (4/35) were ileocecal resections, and 14% (5/35) were right hemicolectomies. All hemicolectomies were performed in situations with intraoperative clinical suspicion of an appendiceal neoplasm. During the surgery, clinical tumor suspicion was aroused significantly more often in the case of periappendicular abscess (27%) compared with uncomplicated acute appendicitis (5%) and in patients with perforated (3%) acute appendicitis (p < 0.001). In the whole study population, no metastasis was found in 200 (80%) cases, but in case of metastasis, the disease was significantly more often disseminated in the case of periappendicular abscess (24/66, 36%) than in uncomplicated (9/148, 6%) or perforated (7/36, 19%) acute appendicitis (p < 0.001).
Out of the 250 patients with both appendiceal tumor and acute appendicitis, 142 patients (57%) had NET, 38 patients (15%) had MANEC or goblet cell carcinoma, and 70 patients (28%) presented with adenocarcinoma or pseudomyxoma (Table 2). Among patients with uncomplicated acute appendicitis (n = 110), the incidence of NETs was highest at 74%, and NETs were also the most common tumor in perforated acute appendicitis (17/36, 47%). In patients with periappendicular abscess, the most prevalent tumors (39/66, 59%) were adenocarcinomas and pseudomyxomas. The severity of acute appendicitis was associated with more malignant tumor histology. The risk of adenocarcinoma and pseudomyxoma was significantly higher among both patients with periappendicular abscess (OR 15.05, CI 95% 6.98–32.49, p < 0.001) and patients with perforated acute appendicitis (OR 4.09, CI 95% 1.69–9.90, p = 0.0018) compared to patients with uncomplicated acute appendicitis. The risk of MANEC and goblet cell carcinoma was higher in patients with periappendicular abscess (OR 4.63, CI 95% 1.88–11.41, p = 0.0009) compared with uncomplicated acute appendicitis, but not significantly higher in patients with perforated acute appendicitis (OR 2.38, CI 95% 0.87–6.52, p = 0.091).
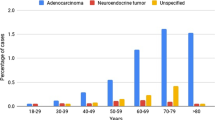
Patient age was significantly associated with appendiceal neoplasm histology. The risk of adenocarcinoma or peudomyxoma was significantly higher in older patients (OR 5.32, Cl 95% 3.34–8.46, p < 0.001). Among patients under the age of 40 years, almost all (91%) appendiceal tumors were NETs. In patients over 40 years, the risk for adenocarcinomas or pseudomyxomas was significantly higher than in patients under 40 years of age (41 vs. 3.5%) (OR 26.46, CI 95% 7.95–88.09, p < 0.001). Both the age of the patient and the severity of acute appendicitis were independent risk factors for more malignant tumor histology (p = 0.330). Out of the 250 patients, 56% (n = 139) were female and 44% (n = 111) were male. Patient sex was not associated with the appendiceal tumor histology (p = 0.670). The risk for more malignant tumor histology did not differ between women and men; for women, the risk of MANEC/goblet cell carcinoma and adenocarcinoma/pseudomyxoma was not higher compared with men (OR 0.94, CI 95% 0.46–1.92, p = 0.860, and OR 1.27, CI 95% 0.71–2.26, p = 0.430, respectively).
Discussion
In this study, both patient age and the severity of acute appendicitis ranging from uncomplicated acute appendicitis to perforated appendicitis and to periappendicular abscess were associated with more malignant histology of the appendiceal neoplasm. The risk of adenocarcinoma or pseudomyxoma was significantly higher among patients over 40 years of age and patients presenting with either periappendicular abscess or perforated acute appendicitis compared with uncomplicated acute appendicitis. Similarly, the higher risk of MANEC and goblet cell carcinoma was associated with periappendicular abscess. Patient sex was not associated with a more malignant appendiceal tumor histology.
The role of interval appendectomy after successful non-operative management of periappendicular abscess is still debated as the reported risk of appendicitis recurrence after the initial successful nonoperative management of periappendicular abscess is quite low [14, 37]. In a small randomized trial comparing emergency laparoscopic appendectomy with antibiotic therapy in the treatment of periappendicular abscess, they reported a 5% prevalence of appendiceal neoplasms [38]. However, other larger studies have reported contradictory alarming rates of appendiceal neoplasms in patients presenting with complicated acute appendicitis and especially associated with periappendicular abscess [23,24,25,26,27]. In this population-based registry study, we have previously reported a significantly higher risk of an appendiceal neoplasm associated with complicated acute appendicitis compared to an uncomplicated form of the disease (3.24 vs. 0.87%), and this risk was even higher in a subgroup analysis comparing periappendicular abscess to uncomplicated acute appendicitis (4.99 vs. 0.87%) [36]. A recent randomized clinical trial by our study group [24] compared interval appendectomy and follow-up with magnetic resonance imaging (MRI) after initial successful non-operative treatment of periappendicular abscess. This trial was prematurely terminated owing to the high rate (17% at interim analysis in the interval appendectomy group with a final rate of 20%) of appendiceal tumors associated with periappendicular abscess. All of the appendiceal tumors were diagnosed in patients over 40 years of age [24]. Similar alarming appendiceal neoplasm rates have been reported in other studies, with appendiceal tumor rates ranging from 10 to 29% [23, 25, 26]. The results of the current secondary analysis of our population-based study corroborate these findings and further support the need for interval appendectomy after initial non-operative management of complicated acute appendicitis. If the high rate of appendiceal neoplasms after periappendicular abscess is validated by future prospective cohorts, appendectomy in the initial acute phase should not be promoted as this would transform a restricted tumor perforation to an unlimited peritoneal spreading.
In addition to appendicitis severity, patient age was significantly associated with more malignant histology of the appendiceal neoplasm. Among patients over 40 years old, the risk of adenocarcinoma or pseudomyxoma was significantly higher compared with patients under 40 years (41 vs. 3.5%), corroborating the findings of previous studies [23,24,25,26].
The strong element of this secondary analysis of the nationwide population-based study [36] is the comprehensive analysis of appendiceal tumor risk and histology between uncomplicated and complicated acute appendicitis. To our knowledge, there are no other studies reporting the association of more malignant histology with increasing appendicitis severity from uncomplicated acute appendicitis to periappendicular abscess. A limitation of this study is that there are only eight study hospitals included instead of the whole Finnish Cancer registry. However, these study hospitals include all Finnish university hospitals and largest central hospitals, representing 70% of the Finnish population and 60% of the registry patient population.
Conclusion
More malignant appendiceal tumor histology of adenocarcinoma or pseudomyxoma was significantly associated with patient age over 40 years and complicated acute appendicitis, especially periappendicular abscess.
Availability of data and material
If interested in the study data and individual patient data, please contact the corresponding author and the principal investigator, and data sharing will be evaluated based on the request.
References
Hansson LE, Laurell H, Gunnarsson U (2008) Impact of time in the development of acute appendicitis. Dig Surg 25:394–399
Livingston EH, Fomby TB, Woodward WA, Haley RW (2011) Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg 146:308–314
Livingston EH, Woodward WA, Sarosi GA, Haley RW (2007) Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg 245:886–892
Salminen P, Paajanen H, Rautio T, Nordstrom P, Aarnio M, Rantanen T et al (2015) Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 313:2340–2348
Salminen P, Tuominen R, Paajanen H, Rautio T, Nordstrom P, Aarnio M et al (2018) Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA 320:1259–1265
Sippola S, Haijanen J, Viinikainen L, Gronroos J, Paajanen H, Rautio T et al (2020) Quality of life and patient satisfaction at 7-year follow-up of antibiotic therapy vs appendectomy for uncomplicated acute appendicitis: a secondary analysis of a randomized clinical trial. JAMA Surg 155:283–289
Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE et al (2020) A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med 383:1907–1919
Sippola S, Gronroos J, Sallinen V, Rautio T, Nordstrom P, Rantanen T et al (2018) A randomised placebo-controlled double-blind multicentre trial comparing antibiotic therapy with placebo in the treatment of uncomplicated acute appendicitis: APPAC III trial study protocol. BMJ Open 8:e023623
Park HC, Kim MJ, Lee BH (2017) Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg 104:1785–1790
Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B et al (2011) Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377:1573–1579
Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH (2018) Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology 287:104–115
Sippola S, Virtanen J, Tammilehto V, Gronroos J, Hurme S, Niiniviita H et al (2020) The accuracy of low-dose computed tomography protocol in patients with suspected acute appendicitis: the OPTICAP study. Ann Surg 271:332–338
Haijanen J, Sippola S, Tammilehto V, Gronroos J, Mantyoja S, Loyttyniemi E et al (2021) Diagnostic accuracy using low-dose versus standard radiation dose CT in suspected acute appendicitis: prospective cohort study. Br J Surg 108:1483–1490
Andersson RE, Petzold MG (2007) Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg 246:741–748
Meshikhes AW (2008) Management of appendiceal mass: controversial issues revisited. J Gastrointest Surg 12:767–775
Simillis C, Symeonides P, Shorthouse AJ, Tekkis pp. (2010) A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery 147:818–829
Whitfield CG, Amin SN, Garner JP (2012) Surgical management of primary appendiceal malignancy. Colorectal Dis 14:1507–1511
Bucher P, Mathe Z, Demirag A, Morel P (2004) Appendix tumors in the era of laparoscopic appendectomy. Surg Endosc 18:1063–1066
Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA (2008) Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol 34:196–201
Tchana-Sato V, Detry O, Polus M, Thiry A, Detroz B, Maweja S et al (2006) Carcinoid tumor of the appendix: a consecutive series from 1237 appendectomies. World J Gastroenterol 12:6699–6701
Charfi S, Sellami A, Affes A, Yaich K, Mzali R, Boudawara TS (2014) Histopathological findings in appendectomy specimens: a study of 24,697 cases. Int J Colorectal Dis 29:1009–1012
Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH (2015) Is there truly an oncologic indication for interval appendectomy?. Am J Surg 209:442–446
Furman MJ, Cahan M, Cohen P, Lambert LA (2013) Increased risk of mucinous neoplasm of the appendix in adults undergoing interval appendectomy. JAMA Surg 148:703–706
Mallinen J, Rautio T, Gronroos J, Rantanen T, Nordstrom P, Savolainen H et al (2019) Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-year outcomes of the peri-appendicitis acuta randomized clinical trial. JAMA Surg 154:200–207
Carpenter SG, Chapital AB, Merritt MV, Johnson DJ (2012) Increased risk of neoplasm in appendicitis treated with interval appendectomy: single-institution experience and literature review. Am Surg 78:339–343
Teixeira FJR Jr, Couto Netto SDD, Akaishi EH, Utiyama EM, Menegozzo CAM, Rocha MC (2017) Acute appendicitis, inflammatory appendiceal mass and the risk of a hidden malignant tumor: a systematic review of the literature. World J Emerg Surg 12:12
Brunner M, Lapins P, Langheinrich M, Baecker J, Krautz C, Kersting S et al (2020) Risk factors for appendiceal neoplasm and malignancy among patients with acute appendicitis. Int J Colorectal Dis 35:157–163
Hsu C, Rashid A, Xing Y, Chiang YJ, Chagpar RB, Fournier KF et al (2013) Varying malignant potential of appendiceal neuroendocrine tumors: importance of histologic subtype. J Surg Oncol 107:136–143
Pape UF, Niederle B, Costa F, Gross D, Kelestimur F, Kianmanesh R et al (2016) ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas). Neuroendocrinology 103:144–152
Landry CS, Woodall C, Scoggins CR, McMasters KM, Martin RC (2008) Analysis of 900 appendiceal carcinoid tumors for a proposed predictive staging system. Arch Surg 143:664–670; discussion 670
McGory ML, Maggard MA, Kang H, O’Connell JB, Ko CY (2005) Malignancies of the appendix: beyond case series reports. Dis Colon Rectum 48:2264–2271
Brathwaite S, Yearsley MM, Bekaii-Saab T, Wei L, Schmidt CR, Dillhoff ME et al (2016) Appendiceal mixed adeno-neuroendocrine carcinoma: a population-based study of the surveillance, epidemiology, and end results registry. Front Oncol 6:148
Tang LH (2010) Epithelial neoplasms of the appendix. Arch Pathol Lab Med 134:1612–1620
Son IT, Ahn S, Park KJ, Oh JH, Jeong SY, Park HC et al (2016) Comparison of long-term oncological outcomes of appendiceal cancer and colon cancer: a multicenter retrospective study. Surg Oncol 25:37–43
Benedix F, Reimer A, Gastinger I, Mroczkowski P, Lippert H, Kube R et al (2010) Primary appendiceal carcinoma–epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol 36:763–771
Lietzen E, Gronroos JM, Mecklin JP, Leppaniemi A, Nordstrom P, Rautio T et al (2019) Appendiceal neoplasm risk associated with complicated acute appendicitis-a population based study. Int J Colorectal Dis 34:39–46
Tekin A, Kurtoglu HC, Can I, Oztan S (2008) Routine interval appendectomy is unnecessary after conservative treatment of appendiceal mass. Colorectal Dis 10:465–468
Mentula P, Sammalkorpi H, Leppaniemi A (2015) Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg 262:237–242
Funding
Open Access funding provided by University of Turku (UTU) including Turku University Central Hospital. This study was supported by the Finnish Government Research Grant (EVO Foundation) awarded to Satasairaala Central Hospital, Pori, Finland.
Author information
Authors and Affiliations
Contributions
EL, PS, JG, and J-PM initiated the study, and PS is the principal investigator. JA, EL, JG, J-PM, AL, PN, TR, TuR, JS, HP, HO, and PS contributed to the implementation of the study, patient enrollment, and data collection. HO performed the statistical analyses. JA, EL, and PS had full access to all the data in the study and verified the data. The manuscript was drafted by JA and EL, which was refined by PS, JG, J-PM, AL, PN, TR, TuR, JS, HP, and HO. All authors approved the final version, and PS had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alajääski, J., Lietzén, E., Grönroos, J.M. et al. The association between appendicitis severity and patient age with appendiceal neoplasm histology—a population-based study. Int J Colorectal Dis 37, 1173–1180 (2022). https://doi.org/10.1007/s00384-022-04132-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04132-8