Abstract
Purpose
Non-operative management of acute uncomplicated appendicitis has shown promising results but might carry the risk of delayed diagnosis of premalignant or malignant appendiceal tumors found by chance in 0.7–2.5% of appendiceal specimen after appendectomy. Purpose of this study was to analyze whether appendiceal tumors are associated with a complicated appendicitis and to determine risk factors for appendiceal neoplasm and malignancy in patients with acute appendicitis.
Methods
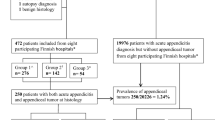
We performed a retrospective analysis of 1033 adult patients, who underwent appendectomy for acute appendicitis from 2010 to 2016 at the University hospital Erlangen. Data included patients’ demographics; comorbidities; pre-, intra- and postoperative findings; and histopathological results. Complicated appendicitis was defined in the presence of perforation or abscess.
Results
Appendiceal neoplasm respectively malignancy rate was 2.8% respectively 1.5%. Using univariate analysis, we identified seven risk factors at least for appendiceal neoplasm or malignancy: age, ASA, C-reactive protein, appendiceal diameter, perforation, intraoperative perithyphilitic abscess, and complicated appendicitis. Risk for appendiceal neoplasm or malignancy was 4.4% respectively 2.7% in complicated acute appendicitis compared to 2.0% respectively 1.0% in uncomplicated appendicitis (p = 0.043 respectively p = 0.060). In multivariate analysis, age ≥ 50 years and a diameter of the appendix in the sonography ≥ 13 mm were independent risk factors predicting the presence of appendiceal neoplasm and malignancy.
Conclusion
Among patients with appendicitis, there are relevant risk factors predicting appendiceal tumors, especially age and appendiceal diameter in sonography. But the identified risk factors have a low sensitivity and specificity, so obtaining a confident preoperative diagnosis is challenging.
Similar content being viewed by others
References
Stewart B, Khanduri P, McCord C et al (2014) Global disease burden of conditions requiring emergency surgery. Br J Surg 101:9–22
Birnbaum BA, Wilson SR (2000) Appendicitis at the millennium. Radiology 215:337–348
Wilms IM, de Hoog DE, de Visser DC, Janzing HM (2011) Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane DatabaseSyst Rev 11:CD008359.
Varadhan KK, Neal KR, Lobo DN (2012) Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ 344:e2156
Hansson J, Korner U, Khorram-Manesh A, Solberg A, Lundholm K (2009) Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg 96:473–481
McCutcheon BA, Chang DC, Marcus LP, Inui T, Noorbakhsh A, Schallhorn C, Parina R, Salazar FR, Talamini MA (2014) Long-term outcomes of patients with nonsurgically managed uncomplicated appendicitis. J Am Coll Surg 218(5):905–913
Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, Karoui M, Alves A, Dousset B, Valleur P, Falissard B, Franco D (2011) Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377(9777):1573–1579
Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Tuominen R, Hurme S, Virtanen J, Mecklin JP, Sand J, Jartti A, Rinta-Kiikka I, Grönroos JM (2015) Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 313(23):2340–2348
Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT (2015) Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 386(10000):1278–1287
Charfi S, Sellami A, Affes A, Yaïch K, Mzali R, Boudawara TS (2014) Histopathological findings in appendectomy specimens: a study of 24,697 cases. Int J Color Dis 29(8):1009–1012
Marudanayagam R, Williams GT, Rees BI (2006) Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol 41(8):745–749
Connor SJ, Hanna GB, Frizelle FA (1998) Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 41(1):75–80
Loftus TJ, Raymond SL, Sarosi GA Jr, Croft CA, Smith RS, Efron PA, Moore FA, Brakenridge SC, Mohr AM, Jordan JR (2017) Predicting appendiceal tumors among patients with appendicitis. J Trauma Acute Care Surg 82(4):771–775
Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH (2015) Is there truly an oncologic indication for interval appendectomy? Am J Surg 209(3):442–446
FurmanMJ CM, Cohen P, Lambert LA (2013) Increased risk of mucinous neoplasm of the appendix in adults undergoing interval appendectomy. JAMA Surg 148(8):703–706
Carpenter SG, Chapital AB, Merritt MV, Johnson DJ (2012) Increased risk of neoplasm in appendicitis treated with interval appendectomy: single-institution experience and literature review. Am Surg 78(3):339–343
Benedix F, Reimer A, Gastinger I, Mroczkowski P, Lippert H, Kube R, Study Group Colon/Rectum Carcinoma Primary Tumor (2010) Primary appendiceal carcinoma--epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol 36(8):763–771
Lietzén E, Grönroos JM, Mecklin JP, Leppäniemi A, Nordström P, Rautio T, Rantanen T, Sand J, Paajanen H, Kaljonen A, Salminen P (2019) Appendiceal neoplasm risk associated with complicated acute appendicitis-a population based study. Int J Color Dis 34(1):39–46
Sadot E, Keidar A, Shapiro R, Wasserberg N (2013) Laparoscopic accuracy in prediction of appendiceal pathology: oncologic and inflammatory aspects. Am J Surg 206(5):805–809
West NE, Wise PE, Herline AJ, Muldoon RL, Chopp WV, Schwartz DA (2007) Carcinoid tumors are 15 times more common in patients with Crohn’s disease. Inflamm Bowel Dis 13(9):1129–1134
Todd RD, Sarosi GA, Nwariaku F, Anthony T (2004) Incidence and predictors of appendiceal tumors in elderly males presenting with signs and symptoms of acute appendicitis. Am J Surg 188(5):500–504
Reich B, Zalut T, Weiner SG (2011) An international evaluation of ultrasound vs. computed tomography in the diagnosis of appendicitis. Int J Emerg Med 4:68
Acknowledgments
The present work was performed in partial fulfillment of the requirements for obtaining the degree “Dr. med” for P. Lapins.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
For this type of study formal consent is not required.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
This study contains no information that would enable individual patient identity.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brunner, M., Lapins, P., Langheinrich, M. et al. Risk factors for appendiceal neoplasm and malignancy among patients with acute appendicitis. Int J Colorectal Dis 35, 157–163 (2020). https://doi.org/10.1007/s00384-019-03453-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03453-5