Abstract
Purpose
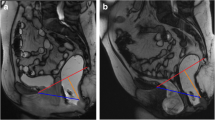
Extra-levator abdominoperineal excision for rectal cancer includes resection of the levator ani muscle and therefore makes pelvic reconstruction advisable. The aim of our study was to evaluate morphologic and functional long-term results of pelvic floor augmentation with porcine dermal collagen mesh by dynamic magnetic resonance imaging and clinical examination.
Methods
Twenty consecutive patients underwent perineal reconstruction with porcine dermal collagen mesh following extra-levator abdominoperineal excision for primary rectal adenocarcinoma with curative intent between 2009 and 2012. Patient perioperative and postoperative data were collected prospectively. There were one cancer-related and two noncancer-related deaths in the follow-up period, and another three patients refused the dynamic magnetic resonance imaging.
Results
Fourteen patients were included in the study. The median time period from surgery to dynamic magnetic resonance imaging and clinical examination was 31 months (range 19–56). Wound infections were observed in 43 % (6 of 14) of these patients in the postoperative period, but no mesh had to be removed. No focal mesh defect, no damage on the suture line, and no perineal hernia were detected on dynamic magnetic resonance imaging. Clinical examination revealed no pathological findings in any patient.
Conclusions
The implantation of a porcine dermal collagen mesh is an effective and reliable option for pelvic floor reconstruction after extra-levator abdominoperineal excision. Despite a high incidence of primary wound infections, the healing rate was satisfactory, no mesh had to be removed, and long-term stability could be achieved.



Similar content being viewed by others
References
Martling A, Holm T, Rutqvist LE, Johansson H, Moran BJ, Heald RJ, Cedermark B (2005) Impact of a surgical training programme on rectal cancer outcomes in Stockholm. Br J Surg 92(2):225–229. doi:10.1002/bjs.4834
Wibe A, Syse A, Andersen E, Tretli S, Myrvold HE, Soreide O, Norwegian Rectal Cancer G (2004) Oncological outcomes after total mesorectal excision for cure for cancer of the lower rectum: anterior vs. abdominoperineal resection. Dis Colon Rectum 47(1):48–58. doi:10.1007/s10350-003-0012-y
Heald RJ, Smedh RK, Kald A, Sexton R, Moran BJ (1997) Abdominoperineal excision of the rectum—an endangered operation. Norman Nigro Lectureship. Dis Colon Rectum 40(7):747–751
Holm T, Ljung A, Haggmark T, Jurell G, Lagergren J (2007) Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 94(2):232–238. doi:10.1002/bjs.5489
Miles WE (1971) A method of performing abdomino-perineal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon (1908). CA Cancer J Clin 21(6):361–364
Huang A, Zhao H, Ling T, Quan Y, Zheng M, Feng B (2014) Oncological superiority of extralevator abdominoperineal resection over conventional abdominoperineal resection: a meta-analysis. Int J Color Dis 29(3):321–327. doi:10.1007/s00384-013-1794-6
Klein M, Fischer A, Rosenberg J, Gogenur I, the Danish Colorectal Cancer G (2014) ExtraLevatory AbdominoPerineal Excision (ELAPE) does not result in reduced rate of tumor perforation or rate of positive circumferential resection margin: a Nationwide Database Study. Ann Surg. doi:10.1097/SLA.0000000000000910
Ortiz H, Ciga MA, Armendariz P, Kreisler E, Codina-Cazador A, Gomez-Barbadillo J, Garcia-Granero E, Roig JV, Biondo S, Spanish Rectal Cancer P (2014) Multicentre propensity score-matched analysis of conventional versus extended abdominoperineal excision for low rectal cancer. Br J Surg 101(7):874–882. doi:10.1002/bjs.9522
Prytz M, Angenete E, Ekelund J, Haglind E (2014) Extralevator abdominoperineal excision (ELAPE) for rectal cancer—short-term results from the Swedish Colorectal Cancer Registry. Selective use of ELAPE warranted. Int J Color Dis 29(8):981–987. doi:10.1007/s00384-014-1932-9
West NP, Anderin C, Smith KJ, Holm T, Quirke P, European Extralevator Abdominoperineal Excision Study G (2010) Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg 97(4):588–599. doi:10.1002/bjs.6916
Asplund D, Haglind E, Angenete E (2012) Outcome of extralevator abdominoperineal excision compared with standard surgery: results from a single centre. Color Dis 14(10):1191–1196. doi:10.1111/j.1463-1318.2012.02930.x
Dalton RS, Smart NJ, Edwards TJ, Chandler I, Daniels IR (2012) Short-term outcomes of the prone perineal approach for extra-levator abdomino-perineal excision (elAPE). Surg J R Coll Surg Edinb Irel 10(6):342–346. doi:10.1016/j.surge.2011.10.001
Jensen KK, Rashid L, Pilsgaard B, Moller P, Wille-Jorgensen P (2014) Pelvic floor reconstruction with a biological mesh after extralevator abdominoperineal excision leads to few perineal hernias and acceptable wound complication rates with minor movement limitations: single-centre experience including clinical examination and interview. Color Dis Off J Assoc Coloproctol G B Irel 16(3):192–197. doi:10.1111/codi.12492
Peacock O, Pandya H, Sharp T, Hurst NG, Speake WJ, Tierney GM, Lund JN (2012) Biological mesh reconstruction of perineal wounds following enhanced abdominoperineal excision of rectum (APER). Int J Color Dis 27(4):475–482. doi:10.1007/s00384-011-1325-2
Welsch T, Mategakis V, Contin P, Kulu Y, Buchler MW, Ulrich A (2013) Results of extralevator abdominoperineal resection for low rectal cancer including quality of life and long-term wound complications. Int J Color Dis 28(4):503–510. doi:10.1007/s00384-012-1611-7
Christensen HK, Nerstrom P, Tei T, Laurberg S (2011) Perineal repair after extralevator abdominoperineal excision for low rectal cancer. Dis Colon Rectum 54(6):711–717. doi:10.1007/DCR.0b013e3182163c89
Horch RE, Hohenberger W, Eweida A, Kneser U, Weber K, Arkudas A, Merkel S, Gohl J, Beier JP (2014) A hundred patients with vertical rectus abdominis myocutaneous (VRAM) flap for pelvic reconstruction after total pelvic exenteration. Int J Color Dis 29(7):813–823. doi:10.1007/s00384-014-1868-0
Han JG, Wang ZJ, Gao ZG, Xu HM, Yang ZH, Jin ML (2010) Pelvic floor reconstruction using human acellular dermal matrix after cylindrical abdominoperineal resection. Dis Colon Rectum 53(2):219–223. doi:10.1007/DCR.0b013e3181b715b5
Oberwalder M, Margreiter R, Maier HT, Zitt M, Ofner D (2009) Acellular porcine cross-linked dermal collagen may be a valuable graft for pelvic floor reconstruction after extended resection. Int J Color Dis 24(3):357–358. doi:10.1007/s00384-008-0629-3
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Kavanagh DO, Imran H, Almoudaris A, Ziprin P, Faiz O (2012) Dynamic magnetic resonance imaging demonstrates the integrity of perineal reconstruction following cylindrical abdominoperineal excision with reconstruction of the pelvic floor using porcine collagen. Case Rep Med 2012:752357. doi:10.1155/2012/752357
Lienemann A, Anthuber C, Baron A, Kohz P, Reiser M (1997) Dynamic MR colpocystorectography assessing pelvic-floor descent. Eur Radiol 7(8):1309–1317. doi:10.1007/s003300050294
Singh K, Reid WM, Berger LA (2001) Assessment and grading of pelvic organ prolapse by use of dynamic magnetic resonance imaging. Am J Obstet Gynecol 185(1):71–77. doi:10.1067/mob.2001.113876
Musters GD, Buskens CJ, Bemelman WA, Tanis PJ (2014) Perineal wound healing after abdominoperineal resection for rectal cancer: a systematic review and meta-analysis. Dis Colon Rectum 57(9):1129–1139. doi:10.1097/DCR.0000000000000182
Aboian E, Winter DC, Metcalf DR, Wolff BG (2006) Perineal hernia after proctectomy: prevalence, risks, and management. Dis Colon Rectum 49(10):1564–1568. doi:10.1007/s10350-006-0669-0
Haapamaki MM, Pihlgren V, Lundberg O, Sandzen B, Rutegard J (2011) Physical performance and quality of life after extended abdominoperineal excision of rectum and reconstruction of the pelvic floor with gluteus maximus flap. Dis Colon Rectum 54(1):101–106. doi:10.1007/DCR.0b013e3181fce26e
Hsu PW, Salgado CJ, Kent K, Finnegan M, Pello M, Simons R, Atabek U, Kann B (2009) Evaluation of porcine dermal collagen (Permacol) used in abdominal wall reconstruction. J Plast Reconstr Aesthet Surg JPRAS 62(11):1484–1489. doi:10.1016/j.bjps.2008.04.060
Rentsch M, Paetzel C, Lenhart M, Feuerbach S, Jauch KW, Furst A (2001) Dynamic magnetic resonance imaging defecography: a diagnostic alternative in the assessment of pelvic floor disorders in proctology. Dis Colon Rectum 44(7):999–1007
Pannu HK, Kaufman HS, Cundiff GW, Genadry R, Bluemke DA, Fishman EK (2000) Dynamic MR imaging of pelvic organ prolapse: spectrum of abnormalities. Radiogr Rev Publ Radiol Soc N Am Inc 20(6):1567–1582. doi:10.1148/radiographics.20.6.g00nv311567
Schmidt J, Redwan B, Koesek V, Heitplatz B, Bedetti B, Aebert H, Wiebe K (2014) Thoracic wall reconstruction with acellular porcine dermal collagen matrix. Thorac Cardiovasc Surg. doi:10.1055/s-0034-1383512
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG Int J Obstet Gynaecol 107(12):1460–1470
Conflict of interest
We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dinnewitzer, A., Meissnitzer, M., Meissnitzer, T. et al. Dynamic magnetic resonance imaging evaluation of pelvic reconstruction with porcine dermal collagen mesh following extra-levator abdominoperineal excision for primary rectal cancer. Int J Colorectal Dis 30, 491–496 (2015). https://doi.org/10.1007/s00384-015-2169-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2169-y