Abstract
Purpose
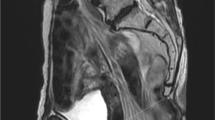
We analysed the outcomes of a series of 100 consecutive patients with anorectal cancer with neoadjuvant radiochemotherapy and abdominoperineal exstirpation or total pelvic exenteration, who received a transpelvic vertical rectus abdominis myocutaneous (VRAM) flap for pelvic, vaginal and/or perineal reconstruction and compare a cohort to patients without VRAM flaps.
Methods
Within a 10-year period (2003–2013) in our institution 924 patients with rectal cancer stage y0 to y IV were surgically treated. Data of those 100 consecutive patients who received a transpelvic VRAM flap were collected and compared to patients without flaps.
Results
In 100 consecutive patients with transpelvic VRAM flaps, major donor site complications occurred in 6 %, VRAM-specific perineal wound complications were observed in 11 % of the patients and overall 30-day mortality was 2 %.
Conclusions
The VRAM flap is a reliable and safe method for pelvic reconstruction in patients with advanced disease requiring pelvic exenteration and irradiation, with a relatively low rate of donor and recipient site complications. In this first study, to compare a large number of patients with VRAM flap reconstruction to patients without pelvic VRAM flap reconstruction, a clear advantage of simultaneous pelvic reconstruction is demonstrated.



Similar content being viewed by others
References
Wong AA, Delclos ME, Wolff RA, Evans DB, Abbruzzese JL, Tamm EP, Xiong HQ, Ho L, Crane CH (2005) Radiation dose considerations in the palliative treatment of locally advanced adenocarcinoma of the pancreas. Am J Clin Oncol 28(3):227–233
Wong CS, Cummings BJ, Brierley JD, Catton CN, McLean M, Catton P, Hao Y (1998) Treatment of locally recurrent rectal carcinoma—results and prognostic factors. Int J Radiat Oncol Biol Phys 40(2):427–435
Sugiyama T, Yakushiji M, Noda K, Ikeda M, Kudoh R, Yajima A, Tomoda Y, Terashima Y, Takeuchi S, Hiura M, Saji F, Takahashi T, Umesaki N, Sato S, Hatae M, Ohashi Y (2000) Phase II study of irinotecan and cisplatin as first-line chemotherapy in advanced or recurrent cervical cancer. Oncology 58(1):31–37
Gerard JP, Romestaing P, Chapet O (2003) Radiotherapy alone in the curative treatment of rectal carcinoma. lancet Oncol 4(3):158–166
Ferrand F, Malka D, Bourredjem A, Allonier C, Bouche O, Louafi S, Boige V, Mousseau M, Raoul JL, Bedenne L, Leduc B, Deguiral P, Faron M, Pignon JP, Ducreux M (2013) Impact of primary tumour resection on survival of patients with colorectal cancer and synchronous metastases treated by chemotherapy: results from the multicenter, randomised trial Federation Francophone de Cancerologie Digestive 9601. Eur J Cancer 49(1):90–97. doi:10.1016/j.ejca.2012.07.006
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidberger H, Raab R (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351(17):1731–1740. doi:10.1056/NEJMoa040694
Hohenberger W, Lahmer G, Fietkau R, Croner RS, Merkel S, Gohl J, Sauer R (2009) Neoadjuvant radiochemotherapy for rectal cancer. Chir Z alle Geb Oper Med 80(4):294–302. doi:10.1007/s00104-009-1707-y
West NP, Anderin C, Smith KJ, Holm T, Quirke P (2010) Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg 97(4):588–599. doi:10.1002/bjs.6916
Nielsen MB, Rasmussen PC, Lindegaard JC, Laurberg S (2012) A 10-year experience of total pelvic exenteration for primary advanced and locally recurrent rectal cancer based on a prospective database. Color Dis Off J Assoc Coloproctol Great Brit Ireland 14(9):1076–1083. doi:10.1111/j.1463-1318.2011.02893.x
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 255(5):922–928. doi:10.1097/SLA.0b013e31824f1c21
Christensen HK, Nerstrom P, Tei T, Laurberg S (2011) Perineal repair after extralevator abdominoperineal excision for low rectal cancer. Dis Colon Rectum 54(6):711–717. doi:10.1007/DCR.0b013e3182163c89
Nielsen MB, Laurberg S, Holm T (2011) Current management of locally recurrent rectal cancer. Color Dis Off J Assoc Coloproctol Great Brit Ireland 13(7):732–742. doi:10.1111/j.1463-1318.2009.02167.x
Wolmark N, Wieand HS, Hyams DM, Colangelo L, Dimitrov NV, Romond EH, Wexler M, Prager D, Cruz AB Jr, Gordon PH, Petrelli NJ, Deutsch M, Mamounas E, Wickerham DL, Fisher ER, Rockette H, Fisher B (2000) Randomized trial of postoperative adjuvant chemotherapy with or without radiotherapy for carcinoma of the rectum: National Surgical Adjuvant Breast and Bowel Project Protocol R-02. J Natl Cancer Inst 92(5):388–396
Zarate AJ, Alonso FT, Garmendia ML, Lopez-Kostner F (2013) Increasing crude and adjusted mortality rates for colorectal cancer in a developing South American country. Color Dis Off J Assoc Coloproctol Great Brit Ireland 15(1):47–51. doi:10.1111/j.1463-1318.2012.03110.x
Lopez-Kostner F, Fazio VW, Vignali A, Rybicki LA, Lavery IC (2001) Locally recurrent rectal cancer: predictors and success of salvage surgery. Dis Colon Rectum 44(2):173–178
Yu HH, Leong CH, Ong GB (1976) Pelvic exenteration for advanced pelvic malignancies. Aust N Z J Surg 46(3):197–201
Emmertsen KJ, Laurberg S (2008) Bowel dysfunction after treatment for rectal cancer. Acta Oncol 47(6):994–1003. doi:10.1080/02841860802195251
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Buchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351. doi:10.1016/j.surg.2009.10.012
Touran T, Frost DB, O'Connell TX (1990) Sacral resection. Operative technique and outcome. Arch Surg 125(7):911–913
Milne T, Solomon MJ, Lee P, Young JM, Stalley P, Harrison JD (2013) Assessing the impact of a sacral resection on morbidity and survival after extended radical surgery for locally recurrent rectal cancer. Ann Surg. doi:10.1097/SLA.0b013e318283a5b6
Colibaseanu DT, Mathis KL, Abdelsatter ZM, Larson DW, Haddock MG, Dozois EJ (2013) Is curative resection and long-term survival possible for locally re-recurrent colorectal cancer in the pelvis? Dis Colon Rectum 56(1):14–19. doi:10.1097/DCR.0b013e3182741929
Horch RE, D'Hoore A, Holm T, Kneser U, Hohenberger W, Arkudas A (2012) Laparoscopic abdominoperineal resection with open posterior cylindrical excision and primary transpelvic VRAM flap. Ann Surg Oncol 19(2):502–503. doi:10.1245/s10434-011-1977-8
Gao XH, Zhang W, Fu CG, Liu LJ, Yu ED, Meng RG (2011) Local recurrence after intended curative excision of presacral lesions: causes and preventions. World J Surg 35(9):2134–2142. doi:10.1007/s00268-011-1155-y
Han SL, Zeng QQ, Shen X, Zheng XF, Guo SC, Yan JY (2010) The indication and surgical results of local excision following radiotherapy for low rectal cancer. Color Dis Off J Assoc Coloproctol Great Brit Ireland 12(11):1094–1098. doi:10.1111/j.1463-1318.2009.02078.x
Jarrett ME, Matzel KE, Stosser M, Christiansen J, Rosen H, Kamm MA (2005) Sacral nerve stimulation for faecal incontinence following a rectosigmoid resection for colorectal cancer. Int J Color Dis 20(5):446–451. doi:10.1007/s00384-004-0729-7
Turk PS, Wanebo HJ (1993) Results of surgical treatment of nonhepatic recurrence of colorectal carcinoma. Cancer 71(12 Suppl):4267–4277
Goligher JC (1986) Sphincter-saving excision for cancers of the middle and lower parts of the rectum. Ann Gastroenterol Hepatol 22(6):361–363
Arnold PG, Lovich SF, Pairolero PC (1994) Muscle flaps in irradiated wounds: an account of 100 consecutive cases. Plast Reconstr Surg 93(2):324–327, discussion 328–329
Bognar G, Novak A, Istvan G, Loderer Z, Ledniczky G, Ondrejka P (2012) Perineal soft-tissue reconstruction with vertical rectus abdominis myocutan (VRAM) flap following extended abdomino-perineal resection for cancer. Magyar sebeszet 65(5):388–395. doi:10.1556/MaSeb.65.2012.5.10
Barker JA, Blackmore AE, Owen RP, Rate A (2012) Prone cylindrical abdominoperineal resection with subsequent rectus abdominis myocutaneous flap reconstruction performed by a colorectal surgeon. Int J Color Dis. doi:10.1007/s00384-012-1586-4
John HE, Jessop ZM, Di Candia M, Simcock J, Durrani AJ, Malata CM (2012) An algorithmic approach to perineal reconstruction after cancer resection—experience from two international centers. Ann Plast Surg. doi:10.1097/SAP.0b013e3182414485
McMenamin DM, Clements D, Edwards TJ, Fitton AR, Douie WJ (2011) Rectus abdominis myocutaneous flaps for perineal reconstruction: modifications to the technique based on a large single-centre experience. Ann R Coll Surg Engl 93(5):375–381. doi:10.1308/003588411X572268
Villa M, Saint-Cyr M, Wong C, Butler CE (2011) Extended vertical rectus abdominis myocutaneous flap for pelvic reconstruction: three-dimensional and four-dimensional computed tomography angiographic perfusion study and clinical outcome analysis. Plast Reconstr Surg 127(1):200–209. doi:10.1097/PRS.0b013e3181f95a54
Shukla HS, Tewari M (2010) An evolution of clinical application of inferior pedicle based rectus abdominis myocutaneous flap for repair of perineal defects after radical surgery for cancer. J Surg Oncol 102(3):287–294. doi:10.1002/jso.21605
Lefevre JH, Parc Y, Kerneis S, Shields C, Touboul E, Chaouat M, Tiret E (2009) Abdomino-perineal resection for anal cancer: impact of a vertical rectus abdominis myocutaneus flap on survival, recurrence, morbidity, and wound healing. Ann Surg 250(5):707–711. doi:10.1097/SLA.0b013e3181bce334
Petrie N, Branagan G, McGuiness C, McGee S, Fuller C, Chave H (2009) Reconstruction of the perineum following anorectal cancer excision. Int J Color Dis 24(1):97–104. doi:10.1007/s00384-008-0557-2
Butler CE, Gundeslioglu AO, Rodriguez-Bigas MA (2008) Outcomes of immediate vertical rectus abdominis myocutaneous flap reconstruction for irradiated abdominoperineal resection defects. J Am Coll Surg 206(4):694–703. doi:10.1016/j.jamcollsurg.2007.12.007
Buchel EW, Finical S, Johnson C (2004) Pelvic reconstruction using vertical rectus abdominis musculocutaneous flaps. Ann Plast Surg 52(1):22–26. doi:10.1097/01.sap.0000099820.10065.2a
Tei TM, Stolzenburg T, Buntzen S, Laurberg S, Kjeldsen H (2003) Use of transpelvic rectus abdominis musculocutaneous flap for anal cancer salvage surgery. Br J Surg 90(5):575–580. doi:10.1002/bjs.4073
Hurst RD, Gottlieb LJ, Crucitti P, Melis M, Rubin M, Michelassi F (2001) Primary closure of complicated perineal wounds with myocutaneous and fasciocutaneous flaps after proctectomy for Crohn's disease. Surgery 130(4):767–772. doi:10.1067/msy.2001.117100, discussion 772–763
Ooi BS, Nyam DC, Cheng C, Tan KC, Koo WH, Lee KS (1999) Transpelvic rectus abdominis flap for perineal reconstruction following abdominal perineal resection with en bloc partial cystectomy and prostatectomy for locally advanced rectal cancer. Singap Med J 40(10):654–655
Smith HO, Genesen MC, Runowicz CD, Goldberg GL (1998) The rectus abdominis myocutaneous flap: modifications, complications, and sexual function. Cancer 83(3):510–520
Jain AK, DeFranzo AJ, Marks MW, Loggie BW, Lentz S (1997) Reconstruction of pelvic exenterative wounds with transpelvic rectus abdominis flaps: a case series. Ann Plast Surg 38(2):115–122, discussion 122–113
de Haas WG, Miller MJ, Temple WJ, Kroll SS, Schusterman MA, Reece GP, Skibber JM (1995) Perineal wound closure with the rectus abdominis musculocutaneous flap after tumor ablation. Ann Surg Oncol 2(5):400–406
Erdmann MW, Waterhouse N (1995) The transpelvic rectus abdominis flap: its use in the reconstruction of extensive perineal defects. Ann R Coll Surg Engl 77(3):229–232
Pena MM, Drew GS, Smith SJ, Given KS (1992) The inferiorly based rectus abdominis myocutaneous flap for reconstruction of recurrent pressure sores. Plast Reconstr Surg 89(1):90–95
Tobin GR, Pursell SH, Day TG Jr (1990) Refinements in vaginal reconstruction using rectus abdominis flaps. Clin Plast Surg 17(4):705–712
Giampapa V, Keller A, Shaw WW, Colen SR (1984) Pelvic floor reconstruction using the rectus abdominis muscle flap. Ann Plast Surg 13(1):56–59
Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD (2010) Postoperative complications following surgery for rectal cancer. Ann Surg 251(5):807–818. doi:10.1097/SLA.0b013e3181dae4ed
El-Gazzaz G, Kiran RP, Lavery I (2009) Wound complications in rectal cancer patients undergoing primary closure of the perineal wound after abdominoperineal resection. Dis Colon Rectum 52(12):1962–1966. doi:10.1007/DCR.0b013e3181b71ef9
Chokshi RJ, Kuhrt MP, Arrese D, Martin EW Jr (2013) Reconstruction of total pelvic exenteration defects with rectus abdominus myocutaneous flaps versus primary closure. Am J Surg 205(1):64–70. doi:10.1016/j.amjsurg.2012.04.010
Horch RE, Gitsch G, Schultze-Seemann W (2002) Bilateral pedicled myocutaneous vertical rectus abdominus muscle flaps to close vesicovaginal and pouch-vaginal fistulas with simultaneous vaginal and perineal reconstruction in irradiated pelvic wounds. Urology 60(3):502–507
D'Souza DN, Pera M, Nelson H, Finical SJ, Tran NV (2003) Vaginal reconstruction following resection of primary locally advanced and recurrent colorectal malignancies. Arch Surg 138(12):1340–1343. doi:10.1001/archsurg.138.12.1340
Horch RE, Kneser U, Weber K, Hohenberger W, Dragu A (2013) The transpelvic vertical rectus abdominis flap: one interdisciplinary approach to reduce postoperative complications following surgery for rectal cancer. Ann Surg 257:e16
Gohl J, Merkel S, Rodel C, Hohenberger W (2003) Can neoadjuvant radiochemotherapy improve the results of multivisceral resections in advanced rectal carcinoma (cT4a). Color Dis off J Assoc Coloproctol Great Brit Ireland 5(5):436–441
Hohenberger W, Bittorf B (2003) Quality of life after rectal excision. Color Dis off J Assoc Coloproctol Great Brit Ireland 5(3):214–217
Hohenberger W, Merkel S, Matzel K, Bittorf B, Papadopoulos T, Gohl J (2006) The influence of abdomino-peranal (intersphincteric) resection of lower third rectal carcinoma on the rates of sphincter preservation and locoregional recurrence. Color Dis off J Assoc Coloproctol Great Brit Ireland 8(1):23–33. doi:10.1111/j.1463-1318.2005.00839.x
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Color Dis off J Assoc Coloproctol Great Brit Ireland 11(4):354–364. doi:10.1111/j.1463-1318.2008.01735.x, discussion 364–355
Merkel S, Wang WY, Schmidt O, Dworak O, Wittekind C, Hohenberger W, Hermanek P (2001) Locoregional recurrence in patients with anastomotic leakage after anterior resection for rectal carcinoma. Color Dis off J Assoc Coloproctol Great Brit Ireland 3(3):154–160
Rodel C, Grabenbauer GG, Matzel KE, Schick C, Fietkau R, Papadopoulos T, Martus P, Hohenberger W, Sauer R (2000) Extensive surgery after high-dose preoperative chemoradiotherapy for locally advanced recurrent rectal cancer. Dis Colon Rectum 43(3):312–319
Siassi M, Weiss M, Hohenberger W, Losel F, Matzel K (2009) Personality rather than clinical variables determines quality of life after major colorectal surgery. Dis Colon Rectum 52(4):662–668. doi:10.1007/DCR.0b013e31819ecf2e
Bittorf B, Stadelmaier U, Gohl J, Hohenberger W, Matzel KE (2004) Functional outcome after intersphincteric resection of the rectum with coloanal anastomosis in low rectal cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Brit Assoc Surg Oncol 30(3):260–265. doi:10.1016/j.ejso.2003.11.011
Hohenberger W (1998) Quality criteria of surgical treatment of rectal carcinoma: preservation of continence, and local recurrence. G Chir 19(5):197–198
Hohenberger W, Merkel S, Hermanek P (2012) Volume and outcome in rectal cancer surgery: the importance of quality management. Int J Color Dis. doi:10.1007/s00384-012-1596-2
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol Off J Am Soc Clin Oncol 30(15):1763–1769. doi:10.1200/JCO.2011.38.3992
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, Becker H, Raab HR, Villanueva MT, Witzigmann H, Wittekind C, Beissbarth T, Rodel C (2012) Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11years. J Clin Oncol Off J Am Soc Clin Oncol 30(16):1926–1933. doi:10.1200/JCO.2011.40.1836
Rodel C, Liersch T, Becker H, Fietkau R, Hohenberger W, Hothorn T, Graeven U, Arnold D, Lang-Welzenbach M, Raab HR, Sulberg H, Wittekind C, Potapov S, Staib L, Hess C, Weigang-Kohler K, Grabenbauer GG, Hoffmanns H, Lindemann F, Schlenska-Lange A, Folprecht G, Sauer R (2012) Preoperative chemoradiotherapy and postoperative chemotherapy with fluorouracil and oxaliplatin versus fluorouracil alone in locally advanced rectal cancer: initial results of the German CAO/ARO/AIO-04 randomised phase 3 trial. Lancet Oncol 13(7):679–687. doi:10.1016/S1470-2045(12)70187-0
Merkel S, Mansmann U, Hohenberger W, Hermanek P (2011) Time to locoregional recurrence after curative resection of rectal carcinoma is prolonged after neoadjuvant treatment: a systematic review and meta-analysis. Color Dis Off J Assoc Coloproctol Great Brit Ireland 13(2):123–131. doi:10.1111/j.1463-1318.2009.02110.x
Hohenberger W (2007) Open surgery of the rectum. Chir Z Alle Geb Oper Med 78(8):739–747. doi:10.1007/s00104-007-1322-8
Shukla HS, Hughes LE (1984) The rectus abdominis flap for perineal wounds. Ann R Coll Surg Engl 66(5):337–339
Creagh TA, Dixon L, Frizelle FA (2012) Reconstruction with vertical rectus abdominus myocutaneous flap in advanced pelvic malignancy. J Plast Rconstr Aesthet Surg JPRAS 65(6):791–797. doi:10.1016/j.bjps.2011.11.063
Sunesen KG, Buntzen S, Tei T, Lindegaard JC, Norgaard M, Laurberg S (2009) Perineal healing and survival after anal cancer salvage surgery: 10-year experience with primary perineal reconstruction using the vertical rectus abdominis myocutaneous (VRAM) flap. Ann Surg Oncol 16(1):68–77. doi:10.1245/s10434-008-0208-4
Nigriny JF, Wu P, Butler CE (2010) Perineal reconstruction with an extrapelvic vertical rectus abdominis myocutaneous flap. Int J Gynecol Cancer Off J Int Gynecol Cancer Soc 20(9):1609–1612. doi:10.1111/IGC.0b013e3181fc11ee
Roe AM, Mortensen NJ (1989) Perineal reconstruction with rectus abdominis flap after resection of anal carcinoma in Crohn's disease. J R Soc Med 82(6):369–370
Houvenaeghel G, Ghouti L, Moutardier V, Buttarelli M, Lelong B, Delpero JR (2005) Rectus abdominis myocutaneous flap in radical oncopelvic surgery: a safe and useful procedure. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 31(10):1185–1190. doi:10.1016/j.ejso.2005.07.004
Hinojosa MW, Parikh DA, Menon R, Wirth GA, Stamos MJ, Mills S (2009) Recent experience with abdominal perineal resection with vertical rectus abdominis myocutaneous flap reconstruction after preoperative pelvic radiation. Am Surg 75(10):995–999
Nelson RA, Butler CE (2009) Surgical outcomes of VRAM versus thigh flaps for immediate reconstruction of pelvic and perineal cancer resection defects. Plast Reconstr Surg 123(1):175–183. doi:10.1097/PRS.0b013e3181904df7
Chan S, Miller M, Ng R, Ross D, Roblin P, Carapeti E, Williams AB, George ML (2010) Use of myocutaneous flaps for perineal closure following abdominoperineal excision of the rectum for adenocarcinoma. Color Dis Off J Assoc Coloproctol Great Br Ireland 12(6):555–560. doi:10.1111/j.1463-1318.2009.01844.x
Nisar PJ, Scott HJ (2009) Myocutaneous flap reconstruction of the pelvis after abdominoperineal excision. Color Dis Off J Assoc Coloproctol Great Br Ireland 11(8):806–816. doi:10.1111/j.1463-1318.2008.01743.x
Hui K, Zhang F, Pickus E, Rodriguez LF, Teng N, Lineaweaver WC (2003) Modification of the vertical rectus abdominis musculocutaneous (VRAM) flap for functional reconstruction of complex vulvoperineal defects. Ann Plast Surg 51(6):556–560. doi:10.1097/01.sap.0000096444.59573.87
Peacock O, Pandya H, Sharp T, Hurst NG, Speake WJ, Tierney GM, Lund JN (2012) Biological mesh reconstruction of perineal wounds following enhanced abdominoperineal excision of rectum (APER). Int J Color Dis 27(4):475–482. doi:10.1007/s00384-011-1325-2
Skipworth RJ, Smith GH, Anderson DN (2007) Secondary perineal hernia following open abdominoperineal excision of the rectum: report of a case and review of the literature. Hernia J Hernias Abdom Wall Surg 11(6):541–545. doi:10.1007/s10029-007-0234-3
Campbell CA, Butler CE (2011) Use of adjuvant techniques improves surgical outcomes of complex vertical rectus abdominis myocutaneous flap reconstructions of pelvic cancer defects. Plast Reconstr Surg 128(2):447–458. doi:10.1097/PRS.0b013e31821e6fd2
Dragu A, Birkholz T, Kleinmann JA, Schnurer S, Munch F, Cesnjevar R, Schmidt J, Taeger C, Kneser U, Horch RE (2011) Extracorporeal perfusion of free muscle flaps in a porcine model using a miniaturized perfusion system. Arch Orthop Trauma Surg 131(6):849–855. doi:10.1007/s00402-010-1251-8
Dragu A, Kleinmann JA, Taeger CD, Birkholz T, Schmidt J, Geppert CI, Prabst K, Unglaub F, Munch F, Weyand M, Kneser U, Horch RE (2012) Immunohistochemical evaluation after ex vivo perfusion of rectus abdominis muscle flaps in a porcine model. Plast Reconstr Surg 130(2):265e–273e. doi:10.1097/PRS.0b013e3182589c2d
Dragu A, Taeger CD, Buchholz R, Sommerfeld B, Hubner H, Birkholz T, Kleinmann JA, Munch F, Horch RE, Prabst K (2012) Online oxygen measurements in ex vivo perfused muscle tissue in a porcine model using dynamic quenching methods. Arch Orthop Trauma Surg 132(5):655–661. doi:10.1007/s00402-011-1458-3
Dragu A, Unglaub F, Wolf MB, Beier JP, Schnabl SM, Kneser U, Leffler M, Horch RE (2010) Scars and perforator-based flaps in the abdominal region: a contraindication? Can J Surg J Can chir 53(2):137–142
Schmidt VJ, Horch RE, Dragu A, Weber K, Gohl J, Mehlhorn G, Kneser U (2012) Perineal and vaginal wall reconstruction using a combined inferior gluteal and pudendal artery perforator flap: a case report. J Plast Reconstr Aesthet Surg JPRAS 65(12):1734–1737. doi:10.1016/j.bjps.2012.04.055
Schmidt VJ, Horch RE, Dragu A, Beier JP, Eyupoglu IY, Hirsch A, Kneser U (2012) Myocutaneous propeller flap based on the superior gluteal artery (SGA) for closure of large lumbosacral meningomyelocoele defects: a case report. J Plast Reconstr Aesthet Surg JPRAS 65(4):521–524. doi:10.1016/j.bjps.2011.08.018
Wong S, Garvey P, Skibber J, Yu P (2009) Reconstruction of pelvic exenteration defects with anterolateral thigh-vastus lateralis muscle flaps. Plast Reconstr Surg 124(4):1177–1185. doi:10.1097/PRS.0b013e3181b5a40f
Kyriazi MA, Stafyla VK, Kondi-Pafiti A, Arkadopoulos N, Dafnios N, Hasiakos D, Fotiou S, Mastorakos D, Smyrniotis V (2010) A novel technique for surgical reconstruction of the perineal floor following anteroposterior exenteration of the pelvis—case report and review of the literature. Eur J Gynaecol Oncol 31(2):201–205
Friedman JD, Reece GR, Eldor L (2010) The utility of the posterior thigh flap for complex pelvic and perineal reconstruction. Plast Reconstr Surg 126(1):146–155. doi:10.1097/PRS.0b013e3181da8769
Abbott DE, Halverson AL, Wayne JD, Kim JY, Talamonti MS, Dumanian GA (2008) The oblique rectus abdominal myocutaneous flap for complex pelvic wound reconstruction. Dis Colon Rectum 51(8):1237–1241. doi:10.1007/s10350-008-9359-4
Bell SW, Dehni N, Chaouat M, Lifante JC, Parc R, Tiret E (2005) Primary rectus abdominis myocutaneous flap for repair of perineal and vaginal defects after extended abdominoperineal resection. Br J Surg 92(4):482–486. doi:10.1002/bjs.4857
Kroll SS, Pollock R, Jessup JM, Ota D (1989) Transpelvic rectus abdominis flap reconstruction of defects following abdominal–perineal resection. Am Surg 55(10):632–637
Stechl NM, Baumeister S, Grimm K, Kraus TW, Bockhorn H, Exner KE (2011) Microsurgical reconstruction of the pelvic floor after pelvic exenteration. Reduced morbidity and improved quality of life by an interdisciplinary concept. Chir Z Alle Geb Oper Med 82(7):625–630. doi:10.1007/s00104-010-2022-3
Goi T, Koneri K, Katayama K, Hirose K, Takashima O, Mizutani Y, Baba H, Yamaguchi A (2003) Modified gluteus maximus V–Y advancement flap for reconstruction of perineal defects after resection of intrapelvic recurrent rectal cancer: report of a case. Surg Today 33(8):626–629
van der Wal BC, Cleffken BI, Gulec B, Kaufman HS, Choti MA (2001) Results of salvage abdominoperineal resection for recurrent anal carcinoma following combined chemoradiation therapy. J Gastrointest Surg Off J Soc Surg Aliment Tract 5(4):383–387
Di Benedetto G, Siquini W, Bertani A, Grassetti L (2010) Vulvo-perineal reconstruction with a reverse sensitive rectus abdominis salvage flap in a multirecurrent anal carcinoma. J Plast Reconstr Aesthet Surg JPRAS 63(2):e127–e129. doi:10.1016/j.bjps.2009.05.055
Daigeler A, Simidjiiska-Belyaeva M, Drucke D, Goertz O, Hirsch T, Soimaru C, Lehnhardt M, Steinau HU (2011) The versatility of the pedicled vertical rectus abdominis myocutaneous flap in oncologic patients. Langenbeck's Arch Surg Deut Ges Chir 396(8):1271–1279. doi:10.1007/s00423-011-0823-6
Baumann DP, Butler CE (2010) Component separation improves outcomes in VRAM flap donor sites with excessive fascial tension. Plast Reconstr Surg 126(5):1573–1580. doi:10.1097/PRS.0b013e3181ef8d00
Soper JT, Havrilesky LJ, Secord AA, Berchuck A, Clarke-Pearson DL (2005) Rectus abdominis myocutaneous flaps for neovaginal reconstruction after radical pelvic surgery. Int J Gynecol Cancer Off J Int Gynecol Cancer Soc 15(3):542–548. doi:10.1111/j.1525-1438.2005.15322.x
Deo SV, Nootan KS, Niranjan B, Dinesh K (2001) Vertical rectus abdominis myocutaneous flap cover for lower abdomen, chest wall, groin and thigh defects following resection of malignant tumours. Indian J Cancer 38(1):33–37
Hsiao WC, Young KC, Wang ST, Lin PW (2000) Incisional hernia after laparotomy: prospective randomized comparison between early-absorbable and late-absorbable suture materials. World J Surg 24(6):747–751, discussion 752
Zimmer S, Fendrich V, Heverhagen J, Rothmund M (2009) [Perineal hernia. A rare complication following abdominoperineal rectal amputation]. Chir Z Alle Geb Oper Med 80(5):462–464–465. doi:10.1007/s00104-008-1637-0
Horch RE, Kneser U, Polykandriotis E, Schmidt VJ, Sun J, Arkudas A (2012) Tissue engineering and regenerative medicine—where do we stand? J Cell Mol Med 16(6):1157–1165. doi:10.1111/j.1582-4934.2012.01564.x
Rath SN, Strobel LA, Arkudas A, Beier JP, Maier AK, Greil P, Horch RE, Kneser U (2012) Osteoinduction and survival of osteoblasts and bone-marrow stromal cells in 3D biphasic calcium phosphate scaffolds under static and dynamic culture conditions. J Cell Mol Med 16(10):2350–2361. doi:10.1111/j.1582-4934.2012.01545.x
Bleiziffer O, Hammon M, Naschberger E, Lipnik K, Arkudas A, Rath S, Pryymachuk G, Beier JP, Sturzl M, Horch RE, Kneser U (2011) Endothelial progenitor cells are integrated in newly formed capillaries and alter adjacent fibrovascular tissue after subcutaneous implantation in a fibrin matrix. J Cell Mol Med 15(11):2452–2461. doi:10.1111/j.1582-4934.2010.01247.x
Boos AM, Loew JS, Deschler G, Arkudas A, Bleiziffer O, Gulle H, Dragu A, Kneser U, Horch RE, Beier JP (2011) Directly auto-transplanted mesenchymal stem cells induce bone formation in a ceramic bone substitute in an ectopic sheep model. J Cell Mol Med 15(6):1364–1378. doi:10.1111/j.1582-4934.2010.01131.x
Dragu A, Schnurer S, Surmann-Schmitt C, von der Mark K, Sturzl M, Unglaub F, Wolf MB, Leffler M, Beier JP, Kneser U, Horch RE (2011) Gene expression analysis of ischaemia and reperfusion in human microsurgical free muscle tissue transfer. J Cell Mol Med 15(4):983–993. doi:10.1111/j.1582-4934.2010.01061.x
Hammon M, Herrmann M, Bleiziffer O, Pryymachuk G, Andreoli L, Munoz LE, Amann KU, Mondini M, Gariglio M, Airo P, Schellerer VS, Hatzopoulos AK, Horch RE, Kneser U, Sturzl M, Naschberger E (2011) Role of guanylate binding protein-1 in vascular defects associated with chronic inflammatory diseases. J Cell Mol Med 15(7):1582–1592. doi:10.1111/j.1582-4934.2010.01146.x
Leffler M, Derrick KL, McNulty A, Malsiner C, Dragu A, Horch RE (2011) Changes of anabolic processes at the cellular and molecular level in chronic wounds under topical negative pressure can be revealed by transcriptome analysis. J Cell Mol Med 15(7):1564–1571. doi:10.1111/j.1582-4934.2010.01147.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horch, R.E., Hohenberger, W., Eweida, A. et al. A hundred patients with vertical rectus abdominis myocutaneous (VRAM) flap for pelvic reconstruction after total pelvic exenteration. Int J Colorectal Dis 29, 813–823 (2014). https://doi.org/10.1007/s00384-014-1868-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1868-0