Abstract
Purpose
This study was designed to evaluate the efficiency of anterior sphincteroplasty in preventing fecal incontinence relapsing in 85 female patients.
Methods
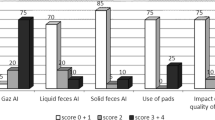
This observational study followed individuals for up to 10 years after intervention. Fecal incontinence relapse was analyzed using Generalized Linear Models and Kaplan-Meier tables. Bias due to informative censoring and missing data were assessed. Two postoperative cutoff Wexner scores (4 and 8) were used to classify individuals into continent or incontinent, and their model implications were examined.
Results
The hazard of relapsing appeared constant over time. This led to exponential time-to-relapse functions, and a linear increase of cumulative hazard over time. Predicted median relapsing time was 33 years, and overall risk 0.09 ± 0.03, when using a cutoff Wexner score of 8 (moderate), and 5 years, overall risk 0.45 ± 0.05, when using a cutoff of 4 (mild). There was a potential underestimation in parameters (bias) due to informative censoring, i.e., individual with better prognoses were more likely to drop out before relapsing compared to those with worse prognoses. Thus, true relapsing times may be longer than our current estimates.
Conclusions
The predictive model can be used in practice for individual prognosis after intervention, based on preoperative Wexner scores. The effect of anterior sphincteroplasty on fecal incontinence does not seem to deteriorate over time. A consensus Wexner cutoff is necessary to compare data and interventions.






Similar content being viewed by others
References
Parés D, Vial M, Bohle B, Maestre Y, Pera M, Roura M, Comas M, Sala M, Grande L (2011) Prevalence of faecal incontinence and analysis of its impact on quality of life and mental health. Color Dis 13:899–905
Bartlett L, Nowak M, Ho Y-H (2009) Impact of fecal incontinence on quality of life. World J Gastroenterol 15:3276–3282
Ho Y, Muller R, Veitch C, Rane A, Durrheim D (2005) Faecal incontinence: an unrecognised epidemic in rural North Queensland? Results of a hospital-based outpatient study. Aust J Rural Health 13:28–34
Siproudhis L, Pigot F, Godeberge P, Damon H, Soudan D, Bigard M (2006) Defecation disorders: a French population survey. Dis Colon Rectum 49:219–227
Kalantar J, Howell S, Talley N (2002) Prevalence of faecal incontinence and associated risk factors; an underdiagnosed problem in the Australian community? Med J Aust 176:54–57
Nelson R, Norton N, Cautley E, Furner S (1995) Community-based prevalence of anal incontinence. JAMA 274:559–561
Lam L, Kennedy M, Chen F (1999) Prevalence of faecal incontinence: obstetric and constipation risk factors: a population based study. Color Dis 1:197–203
Enck P, Bielefeldt K, Rathmann W, Purrmann J, Tschope D, Erckenbrecht J (1991) Epidemiology of faecal incontinence in selected patient groups. Int J Color Dis 6:143–146
Perry S, Shaw C, McGrother C, Matthews R, Assassa R, Dallosso H, Williams K, Brittain K, Azam U, Clarke M, Jagger C, Mayne C, Castleden C (2002) Prevalence of faecal incontinence in adults aged 40 years or more living in the community. Gut 50:480–484
Oom D, Gosselink M, Schouten W (2009) Anterior sphincteroplasty for faecal incontinence: a single centre experience in the era of sacral neuromodulation. Dis Colon Rectum 52:1681–1687
Altomare M, De Fazio M, Giuliani R, Catalano G, Cuccia F (2010) Sphincteroplasty for fecal incontinence in the era of sacral nerve modulation. World J Gastroenterol 16:5267–5271
Gilliland R, Altomare D, Moreira H Jr, Oliveira L, Gilliland J, Wexner S (1998) Pudendal neuropathy is predictive of failure following anterior overlapping sphincteroplasty. Dis Colon Rectum 41:1516–1522
Jorge J, Wexner S (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Haysmith J, Morkved S, Fairbrother A, Herbison GP (2008) Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev
Solomon M, Pager C, Rex J, Roberts R, Manning J (2003) Randomized, controlled trial of biofeedback with anal manometry, transanal ultrasound, or pelvic floorretraining with digital guidancealone in the treatment of mild to moderate fecal incontinence. Dis Colon Rectum 46:703–710
Singer JD, Willett JB (2003) Applied longitudinal data analysis. Oxford University Press
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53(282):457–481
Collett D (1994) Modelling survival data in medical research. Chapman & Hall
El-Gazzaz G, Zutshi M, Hannaway C, Gurland B, Hull T (2012) Overlapping sphincter repair: does age matter? Dis Colon Rectum 55:256–261
Evans C, Davis K, Kumar D (2006) Overlapping anal sphincter repair and anterior levatorplasty: effect of patient’s age and duration of follow-up. Int J Color Dis 21:795–801
Buie WD, Lowry AC, Rothenberg DA, Madoff RD (2001) Clinical rather than laboratory assessment predicts continence after anterior sphincteroplasty. Dis Colon Rectum 44:1255–1260
Ctercteko G, Fazio V, Jagelman D, Lavery I, Weakley FL, Melia M (1988) Anal sphincter repair: a report of 60 cases and review of the literature. Aust N Z J Surg 58:703–710
Oliveira L, Pfeiffer J, Wexner S (1996) Physiological and clinical outcome of anterior sphincteroplasty. Br J Surg 83:502–505
Young C, Mathur M, Eyers A, Solomon M (1998) Successful overlapping anal sphincter repair: relationship to patient age, neuropathy, and colostomy formation. Dis Colon Rectum 41:344–349
EngeI A, Kamm M, Sultan M-I, Bartram C, Nicholls R (1994) Anterior anal sphincter repair in patients with obstetrical tramna. Br J Surg 81:1231–1234
Simmang C, Birnbaum E, Kodner I, Fry R, Fleshman J (1994) Anal sphincter reconstruction in the elderly: does advancing age affect outcome? Dis Colon Rectum 37:1065–1069
Sitzler P, Thompson J (1996) Overlap repair of damaged anal sphincter: a single surgeon’s series. Dis Colon Rectum 39:1356–1360
Chen A, Luchtefeld M, Senagore A, MacKeigan J, Hoyt C (1998) Pudendal nerve latency: does it predict outcome of anal sphincter repair? Dis Colon Rectum 41:1005–1009
Malouf A, Norton C, Engel A, Nicholls R, Kamm M (2000) Long-term results of overlapping anterior anal-sphincter repair for obstetric trauma. Lancet 355:260–265
Felt-Bersma RJ, Cuesta MA, Koorevaar M (1996) Anal sphincter repair improves anorectal function and endosonographic image: a prospective clinical study. Dis Colon Rectum 39:878–885
Londono-Schimmer E, Garcia-Duperly R, Nicholls R, Ritchie J, Hawley P, Thomson J (1994) Overlapping anal sphincter repair for faecal incontinence due to sphincter trauma: five year follow-up functional results. Int J Color Dis 9:110–113
Nikiteas N, Korsgen S, Kumar D, Keighley M (1996) Audit of sphincter repair: factors associated with poor outcome. Dis Colon Rectum 39:1164–1170
Fleshman J, Dreznik Z, Fry R, Kodner I (1991) Anal sphincter repair for obstetric injury: manometric evaluation of functional results. Dis Colon Rectum 34:1061–1067
Rasmussen O, Puggard L, Christiansen J (1999) Anal sphincter repair in patients with obstetric trauma: age affects outcome. Dis Colon Rectum 42:193–195
Vaizey C, Carapeti E, Cahill J, Kamm M (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
American Medical Systems. Fecal incontinence scoring system. American Medical Systems, Minnetonka
Pescatori M, Anastasio G, Bottini C, Mentasti A (1992) New grading system and scoring for anal incontinence. Evaluation of 335 patients. Dis Colon Rectum 35:482–487
Acknowledgments
We acknowledge Dimitrios Vagenas (Ph.D.) and Edward Gosden (Ms.C.) for valuable comments that improved this manuscript. We also acknowledge Thomas Allison (Student of Brisbane Grammar School) for his skilled artwork displayed in the operative figures.
Ethical standards
This study has been approved by the local hospital ethical committee and has therefore been performed in accordance with ethical standards. All patients gave their informed consent prior to inclusion and prior to each phone questionnaire. All patient details that could disclose identity are omitted from this publication.
Conflict of interest
The authors declare that there are explicitly no relationships, financially or otherwise, which would lead to a conflict of interest.
Author contribution
Brendan Mcmanus—data acquisition and analysis and interpretation, drafting the article; Stephen Allison—conception and design + acquisition of data, revising and final approval; Julio Hernánchez-Sánchez—data analysis and interpretation, drafting, and revising.
Disclaimers
None
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Assuming a constant hazard (h) over time, the time-to-relapse function can be written as S(t) = e H(t) = e −ht, where H(t) is the cumulative hazard up to year t, and S(t) is the probability of survival or feacal continence (FC). Thus, the probability of FC after AS decreases exponentially at a rate of e −h per year [18]. An estimate of h can be obtained by regressing H(t) on t, where H(t) is the KM estimate given in Table 1. The resulting equation is H(t) = 0.12 + 0.12t, so S(t) = e −(0.12+0.12t) = 0.89e−0.12t, where t = 0,…,10. The factor 0.89 in S(t) accommodates the fact that S(0) = 0.93, and not 1, i.e., there were six mild FI relapses within the first year after AS, when t = 0. When the critical postoperative WS was 8, the regression of H(t) on t rendered equation H(t) = 0.04 + 0.02t, and thus S(t) = 0.96e−0.02t.
The model in Table 3 for critical WS = 4, predicts h as a function of preoperative WS as \( h=1-{e}^{-{e}^{\eta }} \), where η = −3.55 + 0.13WS, and WS is the preoperative WS. The time-to-relapse function can be shown to be \( S(t)={e}^{-ht}=\frac{e^{t{e}^{\omega }}}{e^t} \), where ω = −0.03 × 1.14WS.
Rights and permissions
About this article
Cite this article
McManus, B.P., Allison, S. & Hernánchez-Sánchez, J. Anterior sphincteroplasty for fecal incontinence: predicting incontinence relapse. Int J Colorectal Dis 30, 513–520 (2015). https://doi.org/10.1007/s00384-015-2162-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2162-5