Abstract
Purpose
The efficacy of the novel SphinKeeper® procedure for the treatment of fecal incontinence (FI) is not yet well defined. This study aimed to assess long-term functional outcomes after SphinKeeper® surgery.
Methods
We included 32 patients with FI (28 female), who were operated at a tertiary referral center between August 2018 and September 2021. Functional outcome and quality of life were evaluated prospectively using validated questionnaires before and after surgery. Additionally, endoanal ultrasound and anal manometry were conducted prior and after SphinKeeper® implantation. Predictive parameters for treatment success were defined.
Results
The mean follow-up time was 22.62 ± 8.82 months. The St. Mark’s incontinence score decreased significantly after surgery (median preoperative = 19 (IQR 17–22) versus median last follow-up = 12 (IQR 8–16), p = 0.001). Similarly, physical short-form health survey showed a significant improvement after SphinKeeper® implantation (p = 0.011).
Patients with a higher degree of internal sphincter defect showed an improved objective therapy success (r = 0.633, p = 0.015) after SphinKeeper® operation, whereas the type and severity of FI had no impact on the functional outcome. Notably, a higher number of dislocated prostheses (r = 0.772, p = 0.015) showed a significant correlation with reduced improvement of incontinence.
Conclusion
The SphinKeeper® procedure showed a significant long-term functional improvement in over half of the patients. Patients with a higher internal sphincter defect benefited most, whereas dislocation of the prostheses was associated with less favorable results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fecal incontinence (FI) represents a devastating condition with a prevalence ranging from 1 to 20% in the general population [1,2,3]. The wide range can be explained by the heterogeneity of available studies and by its taboo topic.
If conservative treatment fails, surgical therapy can improve patients’ complaints and quality of life. Although FI occurs frequently, the number of potential operations is limited and often associated with disappointing outcomes. Surgical procedures comprise the injection of bulking agents, sphincteroplasty or, most effectively, sacral neuromodulation.
The GateKeeper® was introduced as a novel operation defined by the implantation of up to 4 solid prostheses into the intersphincteric grove in 2011 [4]. Early data were promising, showing success rates of above 50% with only a low number of perioperative complications [5]. Subsequently, the technique was further modified by using slightly longer and more (up to 10) prostheses and was renamed SphinKeeper®. Recent short-term publications described a significant improvement in incontinence episodes and quality of life [6,7,8,9,10,11].
Notably, several studies described a migration and dislocation tendency of implanted prostheses. Ratto et al. included ten patients and found a dislocation of a single prosthesis in only one patient [6]. Another investigation by Trenti et al. found a migration rate in 51% of patients using the GateKeeper® with a higher number of migrated prostheses in the non-responder group [12].
The purpose of this long-term cohort study was to evaluate the clinical success rate of SphinKeeper® implantation. In addition, predictive parameters for treatment success were analyzed.
Methods
Thirty-two patients with FI, who underwent SphinKeeper® procedure at a single tertiary referral center, were enrolled prospectively.
The local Ethics Committee of the Medical University of Vienna granted approval. This study was registered at ClinicalTrials.gov (NCT04992429).
Patients were included, who were older than 18 years and reported incontinence for liquid and/or solid stool and flatus incontinence for at least 6 months. All patients were refractory to conservative management including diet changes, stool regulative medication, pelvic floor exercises, and biofeedback therapy for 3 months. Exclusion criteria were local malignant diseases, inflammatory bowel disease, chronic diarrhea without responsiveness to medical treatment and anal fistula disease. A sphincter defect was not regarded as a contraindication for SphinKeeper® therapy.
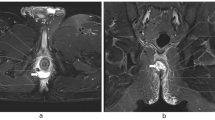
Patients received an endoanal ultrasound examination (EAUS; Flex Focus 500, BK Medical Holding Company, Inc.) to assess internal anal sphincter (IAS) and external anal sphincter (EAS) configurations. Anorectal manometry (ARM) was conducted (THD® Anopress, Pressprobe, Sensyprobe) to analyze resting, squeezing and straining pressure. Anorectal compliance and sensations were recorded by the balloon test.
Functional outcome was assessed using validated standardized questionnaires before surgery, after 3, 6 months and at the last follow-up appointment. The St. Mark’s incontinence score was used to measure FI [13], and obstructive defecation syndrome (ODS) was evaluated by the Wexner constipation score [14]. Quality of life was measured by the short-form health survey (SF-12) [15].
Surgical technique
The surgical implantation was performed in the lithotomy position as described previously [8]. All operations were conducted or supervised by one colorectal surgeon. Patients received a preoperative enema (Klistier® Fressenius, 130 ml) and a single-antibiotic prophylaxis (cefuroxime 1.5 g and metronidazole 1.5 g). In addition, a urinary catheter was installed to allow patients to maintain 24 h of bed rest postoperatively. Subsequently, 9–10 2-mm skin incisions were made at a 2–3 cm distance from the anus. The intersphincteric space was then entered using the delivery system, and the position was checked by endoanal ultrasound. The same procedure was repeated for all ten prostheses around the entire circumference. The skin wounds were closed with absorbable sutures.
Outcome measurements
The primary outcome was defined as a change of FI assessed by St. Mark’s incontinence score at each follow-up visit. In order to evaluate the objective treatment effect and to quantify the dynamic of FI severity, the delta of St. Mark’s incontinence score from prior to SphinKeeper® implantation to the last follow-up was calculated (deltaSMS). Of note, an amelioration of FI severity over time is expressed as a negative value for deltaSMS.
Secondary, dislocation and migration of the implants were recorded, and their impact on functional outcomes was analyzed. The position was considered correct if more than 50% of the prostheses showed correct placement (no dislocation or migration) at the same vertical level (at least two-thirds of the prostheses within the target area as reported by Litta et al. [11]).
The movement of each prothesis along the intersphincteric space was defined as dislocation, the movement through the sphincteric muscle or out of the intersphincteric space as migration.
Statistical analysis
Statistical analysis was performed using the SPSS statistical software package (IBM SPSS Statistics for Mac, Version 26.0). For descriptive statistics, the Shapiro–Wilk test was applied to evaluate normal distribution of the data. Whenever a normal distribution was identified, the mean and standard deviation were reported. Otherwise, the range and the median were mentioned. Accordingly, Student’s t-test or the Wilcoxon signed rank tests were applied as appropriate. Consequently, non-parametric tests were used for the exploratory statistics due to the sample size of n = 32. Here, continuous variables are expressed as median and interquartile range (IQR). Categorical variables are presented as numbers with percentages. Quantitative variables were compared using the Mann–Whitney U test or Wilcoxon test. To explore dichotomous variables, chi-squared test was used. A p-value < 0.05 was considered to denote statistical significance.
Results
Patient characteristics
Between August 2018 and September 2021, 32 patients (28 women and 4 men) suffering from fecal incontinence were treated using the SphinKeeper®. The mean follow-up time was 22.62 ± 8.82 months. Patients’ characteristics are outlined in Table 1.
Surgical outcome
The median number of implanted prostheses was 10 (IQR 9–10), and the median operative time was 37.5 min (IQR 34–48.75). The median postoperative length of hospital stay for patients was 2 days, with an interquartile range of 2–3.
No intraoperative or in-hospital complications were reported. One patient reported perianal discomfort due to the subcutaneous migration of two prostheses after 3 months postoperatively. Those two very superficial located protheses were explanted uneventfully, resulting in resolving of his complaints. This patient experienced functional impairment following the removal and was subsequently subjected to a Re-Do SphinKeeper® implantation using two prostheses [16].
Functional outcome
The St. Mark’s incontinence score decreased significantly comparing preoperative values to the evaluation at last follow-up (median preoperative = 19 (IQR 17–22) versus median last follow-up = 12 (IQR 8–16), p = 0.001; Fig. 1A), demonstrating an amelioration of FI after SphinKeeper® implantation. Similarly, physical SF-12 as an indicator of quality of life significantly improved during the follow-up (median preoperative = 39.4 (IQR 28.6–49.7) versus median last follow-up = 52.0 (IQR 45.9–54.2), p = 0.011; Fig. 1B). In contrast, the SF-12’s mental component did not show a significant difference (median preoperative = 48.2 (IQR 36.7–54.6) versus median last follow-up = 56.9 (IQR 44.6–58.8), p = 0.893; Fig. 1C). The Wexner constipation score at the last follow-up did not differ significantly from preoperative controls (data not shown).
In addition, subjective therapy response was evaluated at the last follow-up visit. Here, 53.8% of patients reported having experienced a symptom relief of at least 50%.
Regarding anal manometry, no significant dynamics were observed after surgery (Table 2). Furthermore, the evaluation of anal sensitivity using the balloon test was comparable between each visit (Table 2).
Prostheses displacement and treatment success
The occurrence of prostheses migration and dislocation is further described in Table 3. During their most recent follow-up visit, 14 patients (43.8%) had dislocated prostheses, and 13 patients (40.6%) had migrated prostheses (at least one). In 20 patients, more than 50% of the prostheses showed correct placement, thus located inside the targeted area (Fig. 2).
Determination of treatment success
In regards to objective treatment response, deltaSMS was significantly lower in patients who reported a subjective treatment response at last follow-up (median no subjective response = − 3.0, median subjective response = − 8.0, p = 0.005).
In order to evaluate whether patients with severe FI might eventually display an increased benefit from SphinKeeper® operation, the cohort was further divided according to the preoperative St. Mark’s incontinence score (cut-off at 12 points). No difference in deltaSMS was observed between patients with high or low preoperative St. Mark’s incontinence scores (median low = − 6.5, median high = − 8.0, p = 0.958).
Next, the effect in association with the type of FI was evaluated. Here, no differences were observed between patients with active, passive or mixed FI (median active = − 6.0, median passive = − 7.5, median mixed = − 4.5; active vs passive: p = 0.641, active vs mixed: p = 0.733, passive vs mixed: p = 1.000).
No correlation was observed between external sphincter damage in degrees and deltaSMS (r = − 0.367, p = 0.266; Fig. 3A). However, the degree of damage of internal sphincter defects showed a strong correlation with deltaSMS (r = − 0.633, p = 0.015), indicating an improved outcome specifically for patients with high degrees of internal sphincter damage (Fig. 3B).
Lastly, the cohort was divided according to respective cut-offs for parameters gathered via rectal manometric examination. Patients with a low preoperative resting sphincter pressure showed a non-significant numeric trend towards improved deltaSMS over time of follow-up when compared with patients with high resting pressure at baseline (cut-off = 22 mmHg; median low resting pressure = − 6.0, median high resting pressure = − 3.0, p = 0.310).
A similar pattern was observed for patients with high or low squeezing pressures in anorectal manometric tests (cut-off = 34 mmHg, median low squeezing pressure = − 6.0, median high squeezing pressure = − 3.0, p = 0.667). In regards to straining pressure, a median at 26 mmHg was used as cut-off. Here, patients with a low straining pressure displayed a trend towards improved deltaSMS, which did not reach statistical significance (median low straining pressure = − 7.0, median high straining pressure = − 2.0, p = 0.114).
The number of dislocated prostheses (r = 0.772, p = 0.015) showed a significant correlation with subjective treatment response in terms of deltaSMS until last follow-up, which indicates the relevance of correct placement of prostheses (Fig. 4).
Discussion
The current analysis revealed a significant improvement of functional parameters and quality of life after the SphinKeeper® surgery. Notably, no effect on anorectal manometry dynamics could be detected. In addition, we were able to define parameters for selecting appropriate candidates for this new device.
The SphinKeeper® device has been the subject of a few studies, whereby most of them reported favorable results with significant improvements of clinical symptoms similar to our findings [6,7,8,9,10,11, 17]. All of them showed a safe implantation with hardly any short- and long-term complications.
La Torre et al. assessed 13 patients, who received SphinKeeper® treatment and measured the anal manometric resting and squeeze pressures, the Cleveland Clinic Fecal Incontinence Score (CCFIS), and the Fecal Incontinence Quality of Life scale (FIQOL) before and 6 months after surgery [9]. They showed that after the procedure, the total number of FI episodes per week and the anal maximal resting pressure improved significantly. Noteworthy, 61.5% of comprised patients had anal sphincter defects with a maximum extension of up to 82°.
Grossi et al. did not include patients with internal or external anal sphincter defects greater than 60° or 90° when comparing the postoperative anal sphincter muscle contractility and tension in 10 patients after SphinKeeper® implantation to those receiving the predecessor (GateKeeper®) [17]. They observed that the SphinKeeper® led to higher muscular tension and similar morpho-functional remodelling of the anal sphincter complex as compared to the GateKeeper®.
The effect of prostheses movement on anal sphincter function remains controversial [18]. Noteworthy, even the exact definition of the type of dislocation varied among studies, making accurate comparison difficult. We have proposed a clear categorization to make future studies comparable [19]. Initially, Ratto et al. identified prostheses migration as an adverse event in one patient (10%), without leading to clinical consequences. In contrast, Grossi et al. found misplaced prostheses in 40% of included patients [17]. However, they did not categorize the patients according to success and prostheses displacement. Accordingly, the impact of dislocation on functional outcome was not discussed. Similarly, Litta et al. reported on 19 patients (45%) with insufficient prostheses localization [11]. The target area was defined at the level of the upper and middle thirds of the anal canal. Notably, FI showed a higher improvement in those patients who had an adequate placement of SphinKeeper® implants.
In a retrospective multicenter audit, Leo et al. reported that despite 10 inserted implants, ultrasonography assessment could only detect a median of seven prostheses after surgery [10], with only five of them were positioned correctly. However, clinical benefit was unrelated to the rate of misplaced/migrated implants.
In the present analysis, we demonstrated that prostheses dislocation affected later functional improvement negatively. Thus, an adequate number of well-sided prostheses are necessary to obtain good outcome, highlighting the impact of careful surgical implantation [20].
The indication for choosing the SphinKeeper® surgery has not been clearly defined so far. In the early studies of the predecessor (GateKeeper®), mainly patients with passive FI were selected for surgery [5, 12]. In the following years, the indications were extended, and patients with urge incontinence or incontinence to flatus were included for SphinKeeper® treatment too, resulting in moderate treatment success [10, 17].
We included patients with active and passive incontinence types and did not exclude patients with even severe forms of incontinence either. Patients with a higher degree of internal sphincter muscle damage seemed to particularly benefit more from the SphinKeeper® surgery.
This can be used as a new selection parameter in the context of daily clinical practice, which till now was not established.
In the beginning of the implementation of this operation, only patients with IAS and EAS sphincter lesions less than 60° were chosen for therapy [5, 10, 17]. SphinKeeper® implantation was later expanded to include patients with IAS or EAS defects reaching 120° [7, 9, 11]. Notably, the only trial that included individuals with defects greater than 120° still showed a significant reduction in the St. Mark’s incontinence score after SphinKeeper® implantation [8]. As a consequence, it can be speculated that childbirth trauma as well as patients with iatrogenic injuries of the internal sphincter muscle are good candidates for SphinKeeper® surgery.
Few limitations of the study need to be addressed. Despite the fact that this study included the second-largest sample with the longest follow-up period published to date, a higher number of patients are needed to obtain further evidence. In addition, patients with all types of incontinence were comprised, resulting in a heterogeneous group of incontinent patients. However, all data were collected prospectively, and patients were carefully assessed by standardized questionnaires and rigorous functional diagnostic work up.
Conclusion
In our long-term study conducted over nearly 2 years, we observed that the SphinKeeper® procedure represents a safe option for patients with fecal incontinence (FI), resulting in a significant functional improvement in approximately 50% of the included patients. Interestingly, patients with a higher internal sphincter defect appeared to derive the most benefit from the SphinKeeper® operation, while the type and severity of FI had no impact on subsequent functional outcomes. However, it is worth noting that dislocation of the prostheses was associated with less favorable results.
Data availability
The raw datasets generated during and/or analyzed during the current study are not publicly available due to the sensitive nature of the questions asked in this study but are available from the corresponding author on reasonable request.
References
Ng KS, Sivakumaran Y, Nassar N, Gladman MA (2015) Fecal incontinence: community prevalence and associated factors–a systematic review. Dis Colon Rectum 58(12):1194–1209
Damon H, Schott AM, Barth X, Faucheron JL, Abramowitz L, Siproudhis L et al (2008) Clinical characteristics and quality of life in a cohort of 621 patients with faecal incontinence. Int J Colorectal Dis 23(9):845–851
Sharma A, Yuan L, Marshall RJ, Merrie AE, Bissett IP (2016) Systematic review of the prevalence of faecal incontinence. Br J Surg 103(12):1589–1597
Ratto C, Parello A, Donisi L, Litta F, De Simone V, Spazzafumo L et al (2011) Novel bulking agent for faecal incontinence. Br J Surg 98(11):1644–1652
Ratto C, Buntzen S, Aigner F, Altomare DF, Heydari A, Donisi L et al (2016) Multicentre observational study of the Gatekeeper for faecal incontinence. Br J Surg 103(3):290–299
Ratto C, Donisi L, Litta F, Campenni P, Parello A (2016) Implantation of SphinKeeper(TM): a new artificial anal sphincter. Tech Coloproctol 20(1):59–66
Colbran R, Gillespie C, Warwick A (2022) A prospective trial of the THD SphinKeeper(R) for faecal incontinence. Colorectal Dis 24(4):491–496
Dawoud C, Bender L, Widmann KM, Harpain F, Riss S (2021) SphinKeeper procedure for treating severe faecal incontinence-a prospective cohort study. J Clin Med. 10(21):4965
La Torre M, Lisi G, Milito G, Campanelli M, Clementi I (2020) SphinKeeper™ for faecal incontinence: a preliminary report. Colorectal Dis 22(1):80–85. https://doi.org/10.1111/codi.14801
Leo CA, Leeuwenburgh M, Orlando A, Corr A, Scott SM, Murphy J, Knowles CH, Vaizey CJ, Giordano P (2020) Initial experience with SphinKeeper™ intersphincteric implants for faecal incontinence in the UK: a two-centre retrospective clinical audit. Colorectal Dis 22(12):2161–2169. https://doi.org/10.1111/codi.15277
Litta F, Parello A, De Simone V, Campennì P, Orefice R, Marra AA et al (2020) Efficacy of SphinkeeperTM implant in treating faecal incontinence. Br J Surg 107:484–488
Trenti L, Biondo S, Noguerales F, Nomdedeu J, Coret A, Scherer R et al (2017) Outcomes of Gatekeeper(TM) prosthesis implantation for the treatment of fecal incontinence: a multicenter observational study. Tech Coloproctol 21(12):963–970
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44(1):77–80
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36(1):77–97
Ware JE, Kosinski M, Keller SD (1995) The SF-12 how to score the SF-12® physical and mental health summary scales, 2nd edn. The health Institute, New England Medical Center, Boston, MA
Dawoud C, Capek B, Bender L, Widmann KM, Riss S (2021) Re-Do Sphinkeeper procedure for treating recurrent faecal incontinence - a video vignette. Colorectal Dis 23(4):1020
Grossi U, Brusciano L, Tolone S, Del Genio G, Di Tanna GL, Gambardella C et al (2020) Implantable agents for fecal incontinence: an age-matched retrospective cohort analysis of GateKeeper versus SphinKeeper. Surg Innov 27(6):608–613
Gassner L, Wild C, Walter M (2022) Clinical effectiveness and safety of self-expandable implantable bulking agents for faecal incontinence: a systematic review. BMC Gastroenterol 22(1):389
Dawoud C, Gidl D, Widmann KM, Pereyra D, Harpain F, Kama B, Riss S (2023) Endosonographic monitoring of Sphinkeeper® prostheses movements: does physical activity have an impact? Updates Surg. https://doi.org/10.1007/s13304-023-01636-y. Epub ahead of print
Dawoud C, Felsenreich DM, Harpain F, Riss S (2023) Surgical technique for SphinKeeper® implantation. Surg Technol Int 43:sti43/1712. Epub ahead of print
Acknowledgements
We thank Andreas Scheuba, M.D. for proofreading this article.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: CD and SR conceived and designed the analysis; CD, KMW and FH collected the data; CD, DP and SR performed the data analysis and interpretation of the results; CD, DP, and SR wrote the manuscript. All authors reviewed the results, critically revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. The ethics committee of the Medical University of Vienna approved this study (no. 1814/2020). This study was registered at ClinicalTrials.gov (NCT04992429) June 18, 2021.
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guarantor.
Associate Professor Stefan Riss, FRCS.
Provenance and peer.
Not commissioned, externally peer-reviewed.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dawoud, C., Widmann, K.M., Pereyra, D. et al. Long-term outcome after SphinKeeper® surgery for treating fecal incontinence—who are good candidates?. Langenbecks Arch Surg 408, 456 (2023). https://doi.org/10.1007/s00423-023-03188-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03188-6