Abstract
Background and aims
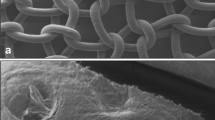
Polypropylene meshes (PPMs) are routinely used in the treatment of incisional hernias to achieve a tension-free closure of the abdominal wall. Severe adhesions are a common cause of intestinal obstruction, or even intestinal fistulas. Using a porcine model, we investigated whether applying a collagen foil (CF) to the undersurface of a PPM will reduce adhesion formation.
Methods
In ten domestic pigs (20–25 kg), a median laparotomy was performed. In each animal the abdominal wall was reconstructed using three types of closure: simple closure by a running suture (control), PPM only, and PPM covered with CF (PPM–CF). After 6 weeks, the abdominal wall with adherent tissue was resected en bloc for macroscopic (quality and quantity of adhesion formation) and histological work-up.
Results
The PPM–CF showed significantly less severe (1.9 vs 3.0 according to a scoring system), and also less extended (23.8 vs 55.9% total coverage of the mesh), adhesions to the resected abdominal wall. Histological examination revealed fewer and less severe inflammatory reactions, necrosis, and foreign body reactions for the mesh and CF (PPM–CF).
Conclusion
To combine meshes with the antiadhesion properties of a CF may be another option to achieve more physiological and more tolerable prosthetic materials.






Similar content being viewed by others
References
Bucknall TE, Cox PJ, Ellis H (1982) Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed) 284:931–933
Langer S, Christiansen J (1985) Long-term results after incisional hernia repair. Acta Chir Scand 151:217–219
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Wissing J, van Vroonhoven TJ, Schattenkerk ME, Veen HF, Ponsen RJ, Jeekel J (1987) Fascia closure after midline laparotomy: results of a randomized trial. Br J Surg 74:738–741
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171:80–84
Cahalane MJ, Shapiro ME, Silen W (1989) Abdominal incision: decision or indecision? Lancet 1:146–148
Hesselink VJ, Luijendijk RW, de Wilt JH, Heide R, Jeekel J (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133:378–382
Simmermacher RK, Schakenraad JM, Bleichrodt RP (1994) Reherniation after repair of the abdominal wall with expanded polytetrafluoroethylene. J Am Coll Surg 178:613–616
Paul A, Korenkov M, Peters S, Kohler L, Fischer S, Troidl H (1998) Unacceptable results of the Mayo procedure for repair of abdominal incisional hernias. Eur J Surg 164:361–367
Luijendijk RW, Lemmen MH, Hop WC, Wereldsma JC (1997) Incisional hernia recurrence following “vest-over-pants” or vertical Mayo repair of primary hernias of the midline. World J Surg 21:62–65, discussion 66
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel JA (2000) Comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398
Liakakos T, Karanikas I, Panagiotidis H, Dendrinos S (1994) Use of Marlex mesh in the repair of recurrent incisional hernia. Br J Surg 81:248–249
Klein P, Konzen G, Schmidt O, Hohenberger W (1996) Reconstruction of scar hernias—intraoperative tensiometry for objective determination of procedure of choice. Chirurg 67:1020–1027
Matapurkar BG, Bhargave A, Dawson L, Sonal B (1999) Regeneration of abdominal wall aponeurosis: new dimension in Marlex peritoneal sandwich repair of incisional hernia. World J Surg 23:446–450, discussion 451
Sauerland S, Schmedt CG, Lein S, Leibl BJ, Bittner R (2005) Primary incisional hernia repair with or without polypropylene mesh: a report on 384 patients with 5-year follow-up. Langenbecks Arch Surg 390:408–412
Schmidbauer S, Ladurner R, Hallfeldt KK, Mussack T (2005) Heavy-weight versus low-weight polypropylene meshes for open sublay mesh repair of incisional hernia. Eur J Med Res 10:247–253
Kaufman Z, Engelberg M, Zager M (1981) Fecal fistula: a late complication of Marlex mesh repair. Dis Colon Rectum 24:543–544
Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, McGuire A, Lower AM, Hawthorn RJ, O’Brien F, Buchan S, Crowe AM (1999) Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 353:1476–1480
DeGuzman LJ, Nyhus LM, Yared G, Schlesinger PK (1995) Colocutaneous fistula formation following polypropylene mesh placement for repair of a ventral hernia: diagnosis by colonoscopy. Endoscopy 27:459–461
Miller K, Junger W (1997) Ileocutaneous fistula formation following laparoscopic polypropylene mesh hernia repair. Surg Endosc 11:772–773
Seelig MH, Kasperk R, Tietze L, Schumpelick V (1995) Enterocutaneous fistula after Marlex net implantation. A rare complication after incisional hernia repair. Chirurg 66:739–741
Ruszczack Z, Calogne H (1998) Kollagen in der Gewebesubstitution: Histologische und immunhistochemische Untersuchungen. Literaturübersicht und eigene Erfahrungen mit einer nativen hochreinen Kollagenmembran (TissuFaszieR). Ellipse 14:33–44
Horch R, Stark G (1996) Kollagen-“Faszie” versus Polyurethanfolie bei der Heilung von Spalthautwunden. Ellipse 12:69–76
Jenkins SD, Klamer TW, Parteka JJ, Condon REA (1983) Comparison of prosthetic materials used to repair abdominal wall defects. Surgery 94:392–398
Tyrell J, Silberman H, Chandrasoma P, Niland J, Shull J (1989) Absorbable versus permanent mesh in abdominal operations. Surg Gynecol Obstet 168:227–232
Amid PK, Shulman AG, Lichtenstein IL, Hakakha M (1994) Biomaterials for abdominal wall hernia surgery and principles of their applications. Langenbecks Arch Chir 379:168–171
Bellon JM, Bujan J, Contreras LA, Carrera-San Martin A, Jurado F (1996) Comparison of a new type of polytetrafluoroethylene patch (Mycro Mesh) and polypropylene prosthesis (Marlex) for repair of abdominal wall defects. J Am Coll Surg 183:11–18
Klosterhalfen B, Junge K, Hermanns B, Klinge U (2002) Influence of implantation interval on the long-term biocompatibility of surgical mesh. Br J Surg 89:1043–1048
Riepe G, Loos J, Imig H, Schroder A, Schneider E, Petermann J, Rogge A, Ludwig M, Schenke A, Nassutt R, Chakfe N, Morlock M (1997) Long-term in vivo alterations of polyester vascular grafts in humans. Eur J Vasc Endovasc Surg 13:540–548
Riepe G, Schröder A, Imig H, Loos G (1995) Welchen Einfluss hat die Materialdegeneration bei der Indikation zur endovaskulären Prothesenimplantation. Zentralbl Chir 120:30
Schumpelick V, Klosterhalfen B, Muller M, Klinge U (1999) Minimized polypropylene mesh for preperitoneal net plasty (PNP) of incisional hernias. Chirurg 70:422–430
Baptista ML, Bonsack ME, Delaney JP (2000) Seprafilm reduces adhesions to polypropylene mesh. Surgery 128:86–92
Bleichrodt RP, Simmermacher RK, van der Lei B, Schakenraad JM (1993) Expanded polytetrafluoroethylene patch versus polypropylene mesh for the repair of contaminated defects of the abdominal wall. Surg Gynecol Obstet 176:18–24
Risberg B (1997) Adhesions: preventive strategies. Eur J Surg Suppl 577:32–39
Ellis H (1997) The clinical significance of adhesions: focus on intestinal obstruction. Eur J Surg Suppl 577:5–9
Porter JM, McGregor FH Jr, Mullen DC, Silver D (1969) Fibrinolytic activity of mesothelial surfaces. Surg Forum 20:80–82
Holmdahl L, al-Jabreen M, Risberg B (1994) Experimental models for quantitative studies on adhesion formation in rats and rabbits. Eur Surg Res 26:248–256
Buckxman RF Jr, Buckman PD, Hufnagel HV, Gervin AS (1976) A physiologic basis for the adhesion-free healing of deperitonealized surfaces. J Surg Res 21:67–76
Zachariou Z, Daum R (1995) Gewebereaktivität prosthetischer Materialien bei der Rekonstruktion von Defekten in der Chirurgie. Langenbecks Arch Chir (suppl II):1337–1344
Matapurkar BG, Gupta AK, Agarwal AK (1991) A new technique of “Marlex-peritoneal sandwich” in the repair of large incisional hernias. World J Surg 15:768–770
Schumpelick V, Conze J, Klinge U (1996) Preperitoneal mesh-plasty in incisional hernia repair. A comparative retrospective study of 272 operated incisional hernias. Chirurg 67:1028–1035
Diamond MP (1998) Reduction of de novo postsurgical adhesions by intraoperative precoating with Sepracoat (HAL-C) solution: a prospective, randomized, blinded, placebo-controlled multicenter study. The Sepracoat Adhesion Study Group. Fertil Steril 69:1067–1074
van ’t Riet M, de Vos van Steenwijk PJ, Bonthuis F, Marquet RL, Steyerberg EW, Jeekel J, Bonjer HJ (2003) Prevention of adhesion to prosthetic mesh: comparison of different barriers using an incisional hernia model. Ann Surg 237:123–128
Verco SJ, Peers EM, Brown CB, Rodgers KE, Roda N, diZerega G (2000) Development of a novel glucose polymer solution (icodextrin) for adhesion prevention: pre-clinical studies. Hum Reprod 15:1764–1772
Greenawalt KE, Butler TJ, Rowe EA, Finneral AC, Garlick DS, Burns JW (2000) Evaluation of sepramesh biosurgical composite in a rabbit hernia repair model. J Surg Res 94:92–98
Mutter D, Jamali FR, Moody DL, Rodeheaver JD, Therm M, Marescaux J (2000) The concept of protected mesh to minimize adhesion formation in intraperitoneal abdominal wall reinforcement. Preclinical evaluation of a new composite mesh. Hernia 4:S3–S9
van’t Riet M, Burger JW, Bonthuis F, Jeekel J, Bonjer HJ (2004) Prevention of adhesion formation to polypropylene mesh by collagen coating: a randomized controlled study in a rat model of ventral hernia repair. Surg Endosc 18:681–685
Gray MR, Curtis JM, Elkington JS (1994) Colovesical fistula after laparoscopic inguinal hernia repair. Br J Surg 81:1213–1214
Hume RH, Bour J (1996) Mesh migration following laparoscopic inguinal hernia repair. J Laparoendosc Surg 6:333–335
Acknowledgement
This work was supported by Baxter, Munich, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schönleben, F., Reck, T., Tannapfel, A. et al. Collagen foil (TissuFoil E) reduces the formation of adhesions when using polypropylene mesh for the repair of experimental abdominal wall defects. Int J Colorectal Dis 21, 840–846 (2006). https://doi.org/10.1007/s00384-006-0091-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-006-0091-z