Abstract
This retrospective study reviews the medical records of 77 fetuses and babies with congenital diaphragmatic hernia (CDH) referred to two hospitals in Detroit from 1986 through 2000. The aims were to examine the effects on outcome of multiple variables, especially the type of CDH, associated anomalies, and ultrasound prognostic parameters. Ultrasound measurements of head (HC), chest (CC), and abdominal circumferences (AC) were obtained from videotapes. ANOVA and chi-square analysis were used to determine statistical significance between groups and proportions. Eighty-nine percent (65/73) of pregnancies resulted in live births, and 54% (35/65) of patients survived past 30 days. Liveborn patients with low APGAR scores were less likely to survive. Forty-three percent (30/70) had major associated anomalies, with cardiac anomalies constituting about 52% (33/64) of the major associated anomalies. Seventy percent of patients with isolated CDH survived versus 36% of patients with both CDH and cardiac anomalies. Sixty-seven percent (8/12) of fetuses antenatally diagnosed before 25 weeks of gestation survived past 30 days of birth. The survival rate of right-sided CDH with liver herniation was 80% (8/10), compared with 29% (4/14) for left-sided CDH with liver herniation ( p =0.088). There was a significant linear relationship ( r =0.603, p =0.029) between CC/AC and CC/HC among patients with CDH; survivors had higher CC/AC and CC/HC values than nonsurvivors. These results support the utility of CC/AC and CC/HC measurements and the presence of liver herniation as important prognostic factors that can be used in antenatal counseling and in planning clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Estimates of the incidence of congenital diaphragmatic hernia (CDH) range between 1 in 1,800 to 1 in 5,900 live births [1, 2, 3]. The higher incidence (1 in 1,800) accounts for the hidden mortality rate (i.e., factoring in estimates of stillbirths and abortions) [1, 2, 4]. The neonatal mortality rate of antenatally diagnosed isolated CDH is high, ranging from 50% to 76% [1, 4, 5]. About 90% of diaphragmatic defects occur posterolaterally, with the defect occurring on the left side about 90% of the time [6].
Understanding the pathophysiologic conditions associated with CDH has led to many innovative therapies for this condition, such as extracorporeal membrane oxygenation (ECMO), nitric oxide, and in utero fetal surgery, with significant enhancement of survival [7]. The study population (i.e., all cases in a defined geographic area and time span of a reporting center), however, also has a major influence on the mortality rates determined for CDH [1], with mortality rates as high as 83% among specific populations [8]. Thus, a review of CDH cases from our area’s healthcare facilities would aid in counseling our specific population as well as others, directing available therapy, developing new therapies, and identifying patients that may benefit from such therapies. Consequently, this study examines the effects on outcome of multiple variables, especially the type of CDH, associated anomalies, and ultrasound prognostic parameters of CDH fetuses and babies referred to two hospitals in Detroit.
Materials and methods
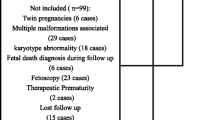
We reviewed the medical records of 77 patients with CDH presenting to two university teaching hospitals in Detroit from 1986 through 2000. This study was approved in advance by the Wayne State University IRB [Protocol #05-53-01(PO4)-ER]. The Children’s Hospital of Michigan is a freestanding children’s hospital with no inborn patients. Hutzel Hospital is less than one mile distant and has the same neonatology staff for its newborn intensive care unit. It also has the obstetric and primary antenatal diagnostic services for the Detroit Medical Center, to which both hospitals belong. Fifty-two percent of CDH cases presenting to Children’s Hospital were referred from Hutzel Hospital, with the remainder from other Detroit-area hospitals.
We collected data on associated anomalies in each patient, including the presence or absence of major associated anomalies. The major associated anomalies were placed in the following categories: syndrome, chromosome, cardiac, pulmonary (other than hypoplasia), central nervous system, musculoskeletal, gastrointestinal (other than malrotation), genitourinary, and other. We did not include minor or acquired anomalies such as pericardial and pleural effusions, ecchymosis of extremities, renal intraparenchymal hemorrhage, hypoxic/ischemic encephalopathy, bronchopleural fistula, and liver abscess. Data collected also included the following:
- (1):
-
The presence of several previously reported indicators of severity, including prematurity (defined as ≤36 weeks gestational age), polyhydramnios, pulmonary hypoplasia (reduced lung volume as noted during ultrasound or surgery), intrathoracic herniation of viscera (we chose any appearance of abdominal viscera as an indication of its presence in the chest; although many of our patients did have several studies, we did not distinguish the different studies for each patient in our data collection), mediastinal shift, prenatal ultrasound diagnosis at <25 weeks, ultrasound chest circumference to abdominal circumference ratio (CC/AC), and ultrasound chest circumference to head circumference ratio (CC/HC)
- (2):
-
Maternal and infant demographics and history
- (3):
-
Mode and place of neonatal delivery
- (4):
-
Outcome of pregnancy, including stillbirth and voluntary interruption of pregnancy (VIP)
- (5):
-
Infant hospital course, including days on ECMO and/or the ventilator, length of stay, inpatient tests, and surgical procedures
CDH types included diaphragmatic eventration and left-sided, right-sided, and anterior CDH. Not all data were available in all charts; therefore, when cases are expressed as a fraction, the denominator is the number of total cases for which data were available.
All ultrasound scans were performed by registered diagnostic medical sonographers and reviewed by a physician (one of the authors). Only complete examinations performed at Hutzel Hospital were included. Freeze-frame capabilities were available, and on-screen calipers were used for determining cross-sectional measurements. For measurement of circumferences, the tracing of each cross-sectional fetal ultrasound image was converted to an actual length using the on-screen calipers as the metric conversion factor. Standard planes were used for measurement of circumferences. The abdominal circumference was determined from a cross-section of the fetal abdomen at well below the heart level but at or above the level of the kidneys. The head circumference was determined at the level of the splenium of the corpus callosum. Ultrasound data were not available for all CDH cases.
Statistical analysis was performed by one-way analysis of variance (ANOVA) using SPSS version 10.0. SPSS was also used for linear regression analysis and the corresponding correlation coefficient and p value. The chi-square analysis was used to test the significance of survival with relation to the laterality of CDH. The Yates correction was applied when the expected frequency was <20. A p value of <0.05 was considered significant. Data in the text are mean ± standard deviation (SD).
Results
Maternal history and patient demographics
Of the 77 records of patients with CDH between 1986 and 2000, there were 72 in the past 11 years (6.5±1.9 cases per year; range 3–9 cases per year). Maternal obstetric history is summarized in Table 1. There was no maternal history of stillbirths. Pregnancy outcomes are shown in Table 2. Eighty-nine percent (65/73) of pregnancies resulted in live births, and 54% (35/65) of patients survived >30 days.
Table 3 displays factors related to survival. Because the presence of a major associated anomaly was of particular importance, we analyzed this group separately. Liveborn patients with low APGAR scores were less likely to survive. Excluding the voluntary interruptions of pregnancies (VIPs) and stillbirths (i.e., restricting the analysis to only live newborns), the birth weight (BW) and gestational age (GA) of survivors and nonsurvivors were not significantly different (Table 3). In contrast, including VIPs and stillbirths significantly alters the BW and GA between survivors and nonsurvivors (Table 3 legend). Sixty-six percent (40/61) of the CDH cases were males. Sixty percent (24/40) of male and 48% (10/21) of female newborns survived past 30 days.
Sixty-three percent (30/48) of the patients for whom data were available went on ECMO. There were no significant differences in BW, GA, or APGAR scores between all live newborns and the subset of patients placed on ECMO (data not shown). Furthermore, 77% (13/17) of newborns not placed on ECMO survived past 30 days, compared with only 52% (14/27) of newborns placed on ECMO. There was no significant difference between survivors and nonsurvivors as to the number of days they were on ECMO (Table 3). Newborns who went on ECMO and survived past 30 days were on ECMO for 12.4±4.3 days ( n =13), whereas nonsurvivors remained on ECMO for 16.7±10.3 days ( n =9, p =0.193) (Table 3). Similarly, there was no significant difference ( p =0.317) between newborns with isolated CDH and those with CDH and other anomalies as to the number of days they were on ECMO (Table 3).
CDH types, associated anomalies, and laterality
Seventy-two percent (48/67) of our patients had left-sided, posterolateral or Bochdalek defects. Twenty-four percent (16/67) of CDH cases were right-sided, 2% (1/67) were anterior, and 3% (2/67) were described as eventrations. In the remaining 10 cases, the description was not sufficient for us to classify the defect. Forty-three percent (30/70) of cases had associated major anomalies. Table 4 lists these anomalies as well as their frequencies. Cardiac anomalies were the most frequent (33/64), followed by musculoskeletal anomalies (13/64). Patent ductus arteriosus (PDA) represented 36% (12/33) of all cardiac anomalies, and ventricular septal defect was the second most frequent cardiac anomaly (5/33). Sixty-seven percent (8/12) of CDH cases with PDA did not survive past 30 days. Cases with associated musculoskeletal and gastrointestinal (nonmalrotation) anomalies did not survive. There was no relationship between the side of the defect or its type and the incidence of major associated anomalies (data not shown).
Indicators of severity and survival
Patients with CDH and major associated anomalies had a poorer outcome than patients with isolated CDH (Table 5). Survival for isolated CDH cases was twice that for those with an associated cardiac anomaly. The worst indicators of severity were pulmonary hypoplasia and the presence of liver, stomach, or spleen in the chest; the survival of these cases ranged from 41% to 48% (45.1±3.1, n =4). The average survival of patients with herniation of liver, stomach, or spleen was 46%, significantly less than the 61% survival of CDH cases with bowel herniation. The more favorable prognostic indicators included bowel herniation, prenatal diagnosis, and prematurity. There was no statistically significant survival advantage for right-sided compared with left-sided CDH cases. In examining the relationship of survival with laterality of CDH, however, the relationship closest to the arbitrarily assigned threshold of statistical significance ( p =0.05) was the combination of liver herniation and laterality. The survival rate of right-sided CDH with liver herniation was 80% (8/10), compared with 29% (4/14) for left-sided CDH with liver herniation ( p =0.088).
Sixty-seven percent (8/12) of fetuses antenatally diagnosed with CDH by ultrasound before 25 weeks of gestation survived past 30 days of birth (Table 5). However, 25% (7/28) of mothers antenatally diagnosed by ultrasound to have a fetus with CDH elected to terminate their pregnancy. This may be an overestimate because the status of the antenatal diagnosis of the remaining 49 cases was not clearly documented in the records.
There was a significant linear relationship between the ultrasound parameters CC/AC and CC/HC among patients with CDH. CC/AC = 0.369 + [0.729 × (CC/HC)] with the coefficient of correlation r =0.603, p =0.029, and n =13 (Fig. 1). The mean ± SD was 0.95±0.07 for CC/AC (range 0.80–1.06, n =13) and 0.80±0.06 for CC/HC (range 0.68–0.87, n =13). As expected, CC and HC, and AC and HC were linearly related: AC = −14.268 + (0.912 × HC) with r =0.972 and p <0.001, and CC = −10.271 + (0.844 × HC) with r =0.957 and p <0.001. The slope of the AC versus HC regression among CDH cases (0.972) is very close to what is reported for normal fetuses (0.979) [9]; because HC and AC in CDH patients are the same as in normal patients, CC/HC and CC/AC reflect the degree of difference between CDH and normal patients. Ultrasound parameters in survivors and nonsurvivors are shown in Fig. 2. Note that Fig. 2 data do not include VIPs or stillbirths. All cases (3/3) with CC/AC <0.95 and CC/HC ≤0.80 died (not including the VIP case). In contrast, two-thirds of the cases with CC/AC ≥0.95 and CC/HC >0.80 survived. The positive and negative predictive values for CC/AC ( n =7) were 75% and 14%, respectively, and for CC/HC ( n =7) were 50% and 67%, respectively. The final status of four cases with complete ultrasound data was not known, and two mothers elected VIP. Thus, survivors had higher CC/AC and CC/HC values, and there was no significant difference between the ultrasound parameters HC/AC or femur length/AC and survival.
Relationship between the ultrasound parameters chest circumference to abdominal circumference ratio (CC/AC) and chest circumference to head circumference ratio (CC/HC) among patients with CDH. Thick line represents a linear regression through the 13 data points, with y = 0.369 + (0.729 × x), coefficient of correlation r =0.603, p =0.029. Solid circles represent nonsurvivors ( VIP, voluntary interruption of pregnancy); open circles represent survivors; and open squares represent patients with final status unknown. Thin lines represent CC/AC and CC/HC mean values, 0.95 and 0.80 respectively
Antenatal ultrasound characteristics as prognostic indicators in CDH. Open and solid circles represent survivors and nonsurvivors, respectively. Ultrasound data from stillbirths and voluntary interruptions of pregnancy were not included here. Numbers indicate number of data points coinciding with that value
Discussion
Our results are consistent with those from a recent CDH meta-analysis of mortality factors [1] (compared in Table 6). The survival rates of isolated CDH and CDH with major associated anomalies in this study were higher than the pooled values in the meta-analysis study (70.0 and 43.5% in this study versus 56.8 and 18.6% in the meta-analysis study, respectively). In this study, the ratio of survival rates of isolated CDH to CDH with major associated anomalies was about two-fold, compared with the three-fold ratio from pooled data reported by Skari et al. [1] Our overall survival rate (54%) was higher than the pooled value of 42% from the meta-analysis and more representative of the upper range of values referred to in the study (range 17–55%). The survival rate observed here is consistent with other recent retrospective reviews of CDH cases from the United Kingdom (a 13-year study) and France (a 5-year study), in which overall survival rates of 50% [10] and 56% [11] were observed, respectively. It has been reported, however, that survival rates at many centers are approaching 90% or higher [12].
In this study the overall percentage of VIP was 10%, about two-fold higher than the pooled percentage in the meta-analysis of Skari et al. [1] but within the range of 0.8–20.5% from references used in the meta-analysis. Furthermore, in this study 25% (7/28) of mothers antenatally diagnosed prior to 25 weeks of gestation to have a fetus with CDH elected to terminate the pregnancy. This value is close to the 32% (12/37) observed by Dillon et al. [10] for mothers under similar circumstances referred to the Northern Region Congenital Abnormality Survey in the UK between the years 1985 and 1997.
Associated major congenital anomalies are reported to occur in 40% of infants, with cardiac abnormalities the most prevalent [6]. In the present series, associated major anomalies were also frequent (43% of patients), with cardiac anomalies still the most common (52% of major associated anomalies). In several population-based studies, the mortality in CDH infants with major associated anomalies was about twice that seen in those with isolated CDH [1], similar to rates observed in this series (56% and 30%). In addition, there was no relationship between the side of the defect or its type and the incidence of major associated anomalies (data not shown), consistent with the conclusion of others [13].
Ultrasound is now successfully used to diagnose fetuses with CDH and to define the natural history and pathophysiologic features of this lesion. Significant effort has been directed toward identifying ultrasound parameters that will predict fetal and ultimately neonatal outcome in affected pregnancies. Among the prognostic parameters investigated are fetal cardiac ventricular disproportion, cardiac weight, lung area to head circumference ratio (LHR), liver and stomach herniation, degree of polyhydramnios, degree of mediastinal shift, right lung to thorax transverse area ratio, fetal breathing movements, and nasal fluid flow velocities [4, 14, 15, 16, 17]. Metkus et al. [15] examined fetuses with isolated left-sided CDH and concluded that LHR was highly predictive of survival. Although the usefulness of many of the above-mentioned parameters appears to be unpredictable when examined by others [4], two sonographic parameters, namely the LHR and the degree of liver herniation, appear promising, and further confirmation has been recommended. Furthermore, the usefulness of thoracic circumference to abdominal circumference ratio for evaluating fetal pulmonary hypoplasia suggests that it may also be useful for evaluation in CDH [18].
The linear relationship observed ( r =0.603, p =0.029) between CC/AC and CC/HC in our population, along with the way individual cases fared along this relationship, suggests that cases with CC/AC ≥0.95 and CC/HC >0.80 have a better chance of survival than those with low values for CC/AC and CC/HC, a finding that is consistent with the conclusions of others [4, 15, 18, 19,20]. This is of prognostic value and could aid in counseling mothers with CDH fetuses. The CC/HC range in this study (0.68–0.87) was narrower than that reported in Metkus et al. [15], who obtained values of <0.6 and >1.35 for the LHR equivalent to CC/HC in this study. However, the survival rate reported by Metkus at al. [15] for the CDH fetuses with LHR >0.6 and ≤1.35 was 57% (16/28), which is comparable to the 43% (3/7) obtained in this study. Others have found an overall survival of 47%, with LHR ranging from 0.62 to 1.86 (reviewed in Muratore and Wilson [12]).
The presence or absence of abdominal viscera in the chest is a dynamic process. Liver herniation is believed to be a poor prognostic indicator, with a 57% survival rate if present [4]. In addition, fetuses with a left-sided CDH who have liver herniation and a low LHR are at higher risk of neonatal demise and benefit from newer surgical therapies [19]. Our finding of a higher survival rate of right-sided CDH with liver herniation compared with patients with left-sided CDH and liver herniation (80% versus 29%, respectively) may reflect the fact that repairing herniation of the left lobe of the liver is a technically more challenging obstacle and is associated with a higher mortality risk.
The remarkable finding in this study is that the more favorable prognostic indicators included prenatal diagnosis and prematurity, both of which have been previously found to be particularly poor prognostic factors, even in our own previous reports [21, 22, 23]. This difference is probably explained, at least in part, by the fact that antenatal diagnosis has become almost routine with the advent of frequent screening ultrasounds during pregnancy and that many mothers chose termination of pregnancy once the diagnosis was made antenatally (but this still does not select for those more likely to survive). It is also possible that the limited number of recorded premature patients in this study (eight) may not accurately represent the CDH population. This study does, however, indicate the importance of continuing to reevaluate our experience with CDH so that we are not making treatment plans for tomorrow’s patients based entirely on data from yesterday’s patients.
References
Skari H, Bjornland K, Haugen G, et al. (2000) Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg 35:1187–1197
Adzick NS, Harrison MR (1997) The fetus as patient. In: Oldham KT, Colombani PM, Foglia RP (eds) Surgery of infants and children: scientific principles and practice. Philadelphia, Lippincott-Raven, pp 48–64
Stolar CJH (1997) Congenital diaphragmatic hernia. In: Oldham KT, Colombani PM, Foglia RP (eds) Surgery of infants and children: scientific principles and practice. Philadelphia, Lippincott-Raven, pp 883–895
Flake AW (1996) Fetal surgery for congenital diaphragmatic hernia. Semin Pediatr Surg 5:266–274
Clark RH, Hardin WDJ, Hirschl RB (1998) Current surgical management of congenital diaphragmatic hernia: a report from the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg 33:1004–1009
Greenholz SK (1996) Congenital diaphragmatic hernia: an overview. Semin Pediatr Surg 5:216–223
Klein MD (1996) Congenital diaphragmatic hernia: an introduction. Semin Pediatr Surg 5:213–215
Puri P, Gorman F (1984) Lethal nonpulmonary anomalies associated with congenital diaphragmatic hernia: implications for early intrauterine surgery. J Pediatr Surg 19:29–32
Gordon JD, Rydfors JT, Druzin ML, Tadir Y (2001) Obstetrics, gynecology and infertility (5th edn). Arlington, VA, Scrub Hill Press
Dillon E, Renwick M, Wright C (2000) Congenital diaphragmatic herniation: antenatal detection and outcome. Br J Radiol 73:360–365
Dubois A, Storme L, Jaillard S, et al. (2000) Congenital hernia of the diaphragm. A retrospective study of 123 cases recorded in the Neonatal Medicine Department, URHC in Lille between 1985 and 1996. Arch Pediatr 7:132–142
Muratore CS, Wilson JM (2000) Congenital diaphragmatic hernia: where are we and where do we go from here? Semin Perinatol 24:418–428
Losty PD, Vanamo K, Rintala RJ, et al. (1998) Congenital diaphragmatic hernia: does the side of the defect influence the incidence of associated malformations? J Pediatr Surg 33:507–510
Karamanoukian HL, O’Toole SJ, Rossman JR, et al. (1996) Can cardiac weight predict lung weight in patients with congenital diaphragmatic hernia? J Pediatr Surg 31:823–825
Metkus AP, Filly RA, Stringer MD, et al. (1996) Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg 31:148–151, discussion 151–152
Hatch EI, Jr., Kendall J, Blumhagen J (1992) Stomach position as an in utero predictor of neonatal outcome in left- sided diaphragmatic hernia. J Pediatr Surg 27:778–779
Kamata S, Hasegawa T, Ishikawa S, et al. (1992) Prenatal diagnosis of congenital diaphragmatic hernia and perinatal care: assessment of lung hypoplasia. Early Hum Dev 29:375–379
Yoshimura S, Masuzaki H, Gotoh H, et al. (1996) Ultrasonographic prediction of lethal pulmonary hypoplasia: comparison of eight different ultrasonographic parameters. Am J Obstet Gynecol 175:477–483
Harrison MR, Mychaliska GB, Albanese CT, et al. (1998) Correction of congenital diaphragmatic hernia in utero IX: fetuses with poor prognosis (liver herniation and low lung-to-head ratio) can be saved by fetoscopic temporary tracheal occlusion. J Pediatr Surg 33:1017–1022, discussion 1022–1023
Harrison MR, Adzick NS, Bullard KM, et al. (1997) Correction of congenital diaphragmatic hernia in utero VII: a prospective trial. J Pediatr Surg 32:1637–1642
Sreenan C, Etches P, Osiovich H (2001) The western Canadian experience with congenital diaphragmatic hernia: perinatal factors predictive of extracorporeal membrane oxygenation and death. Pediatr Surg Int 17:196–200
Lessin MS, Thompson IM, Deprez MF, et al. (1995) Congenital diaphragmatic hernia with or without extracorporeal membrane oxygenation: are we making progress? J Am Coll Surg 181:65–71
Adzick NS, Harrison MR, Glick PL, et al. (1985) Diaphragmatic hernia in the fetus: prenatal diagnosis and outcome in 94 cases. J Pediatr Surg 20:357–361
Acknowledgments
We thank Dr. Erawati Bawle for critically reading this manuscript and Yin Hu and Dr. Ron Thomas for making the SPSS software available for this study. This study was supported in part by the ENSURE Foundation and by a Medical Student Summer Research Grant from Wayne State University School of Medicine to JKB. This work received honorable mention as a poster presentation at the 8th Annual Meeting of the Michigan Chapter of the American College of Physicians/American Society of Internal Medicine, Traverse City, MI, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
JKB dedicates this manuscript to the memory of his father, Krikor O. Bedoyan.
Rights and permissions
About this article
Cite this article
Bedoyan, J.K., Blackwell, S.C., Treadwell, M.C. et al. Congenital diaphragmatic hernia: associated anomalies and antenatal diagnosis. Ped Surgery Int 20, 170–176 (2004). https://doi.org/10.1007/s00383-004-1138-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1138-2