Abstract
Congenital diaphragmatic hernia (CDH) is a malformation that continues to cause significant morbidity and mortality and can be difficult to clinically manage. Determination of prognosis can greatly add to the decision-making process in prenatally recognized CDH, predominantly by the recognition of specific ultrasound findings. Ultrasound findings that are important include hernia type, laterality, lung size, position of the fetal liver and stomach, and the presence or absence of other anomalies. In general, prognosis is best in cases where CDH is an isolated anomaly, the liver and stomach remain within the abdominal cavity, and the lung size corresponds to a lung area to head circumference ratio of ≥1. Position of the stomach also corresponds with prognosis, is easier to reliably determine with ultrasound, and can indirectly predict the position of the liver. The following is a review of the literature and experience in the care of fetuses with CDH at the University of California, San Francisco, a large tertiary referral center, in using these ultrasound findings to predict prognosis.






Similar content being viewed by others
References
Skari H, et al. Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg. 2000;35(8):1187–97.
Downard CD, et al. Analysis of an improved survival rate for congenital diaphragmatic hernia. J Pediatr Surg. 2003;38(5):729–32.
Bouchghoul H, et al. Congenital diaphragmatic hernia: does gestational age at diagnosis matter when evaluating morbidity and mortality? Am J Obstet Gynecol. 2015;213(4):535 e1–7.
Russo FM, Eastwood M, Keijzer R, Al-Maary J, Toelen J, Mieghem TV, Deprest JA. Lung size and liver herniation predict the need for extra corporeal membrane oxygenation but not pulmonary hypertension in isolated congenital diaphragmatic hernia. Ultrasound Obstet Gynecol. 2016. doi:10.1002/uog.16000 (Epub ahead of print).
Grivell RM, Andersen C, Dodd JM. Prenatal interventions for congenital diaphragmatic hernia for improving outcomes. Cochrane Database Syst Rev. 2015;11:CD008925.
Kays DW, et al. Long-term maturation of congenital diaphragmatic hernia treatment results: toward development of a severity-specific treatment algorithm. Ann Surg. 2013;258(4):638–44 discussion 644–5.
Sandstrom CK, Stern EJ. Diaphragmatic hernias: a spectrum of radiographic appearances. Curr Probl Diagn Radiol. 2011;40(3):95–115.
Slepov O, et al. Congenital retrosternal hernias of Morgagni: manifestation and treatment in children. Afr J Paediatr Surg. 2016;13(2):57–62.
Clark RH, et al. Current surgical management of congenital diaphragmatic hernia: a report from the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg. 1998;33(7):1004–9.
Seetharamaiah R, et al. Factors associated with survival in infants with congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: a report from the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg. 2009;44(7):1315–21.
Tibboel D, Gaag AV. Etiologic and genetic factors in congenital diaphragmatic hernia. Clin Perinatol. 1996;23(4):689–99.
Akinkuotu AC, et al. An evaluation of the role of concomitant anomalies on the outcomes of fetuses with congenital diaphragmatic hernia. J Pediatr Surg. 2016;51(5):714–7.
Hidaka N, et al. Associated anomalies in congenital diaphragmatic hernia: perinatal characteristics and impact on postnatal survival. J Perinat Med. 2015;43(2):245–52.
Graziano JN, G. Congenital Diaphragmatic Hernia Study. Cardiac anomalies in patients with congenital diaphragmatic hernia and their prognosis: a report from the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg. 2005;40(6):1045–9 discussion 1049–50.
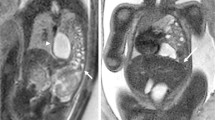
Leung JW, et al. Prenatal MR imaging of congenital diaphragmatic hernia. AJR Am J Roentgenol. 2000;174(6):1607–12.
Kays DW, et al. Improved survival in left liver-up congenital diaphragmatic hernia by early repair before extracorporeal membrane oxygenation: optimization of patient selection by multivariate risk modeling. J Am Coll Surg. 2016;222(4):459–70.
Akinkuotu AC, et al. Revisiting outcomes of right congenital diaphragmatic hernia. J Surg Res. 2015;198(2):413–7.
Wright JC, et al. Epidemiology and outcome of congenital diaphragmatic hernia: a 9-year experience. Paediatr Perinat Epidemiol. 2011;25(2):144–9.
Schaible T, et al. Right- versus left-sided congenital diaphragmatic hernia: postnatal outcome at a specialized tertiary care center. Pediatr Crit Care Med. 2012;13(1):66–71.
Colvin J, et al. Outcomes of congenital diaphragmatic hernia: a population-based study in Western Australia. Pediatrics. 2005;116(3):e356–63.
Fisher JC, et al. Redefining outcomes in right congenital diaphragmatic hernia. J Pediatr Surg. 2008;43(2):373–9.
Slavotinek AM, et al. Population-based analysis of left- and right-sided diaphragmatic hernias demonstrates different frequencies of selected additional anomalies. Am J Med Genet A. 2007;143A(24):3127–36.
Losty PD, et al. Congenital diaphragmatic hernia–does the side of the defect influence the incidence of associated malformations? J Pediatr Surg. 1998;33(3):507–10.
Iqbal CW, et al. Outcomes for prenatally diagnosed right congenital diaphragmatic hernia. Fetal Diagn Ther. 2015 (Epub ahead of print).
Mullassery D, et al. Value of liver herniation in prediction of outcome in fetal congenital diaphragmatic hernia: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2010;35(5):609–14.
Lusk LA, et al. Fetal ultrasound markers of severity predict resolution of pulmonary hypertension in congenital diaphragmatic hernia. Am J Obstet Gynecol. 2015;213(2):216 e1–8.
Lazar DA, et al. Defining “liver-up”: does the volume of liver herniation predict outcome for fetuses with isolated left-sided congenital diaphragmatic hernia? J Pediatr Surg. 2012;47(6):1058–62.
Harrison MR, et al. Fetoscopic temporary tracheal occlusion for congenital diaphragmatic hernia: prelude to a randomized, controlled trial. J Pediatr Surg. 2003;38(7):1012–20.
Knox E, et al. Prenatal detection of pulmonary hypoplasia in fetuses with congenital diaphragmatic hernia: a systematic review and meta-analysis of diagnostic studies. J Matern Fetal Neonatal Med. 2010;23(7):579–88.
Yang SH, et al. Reliability of the lung-to-head ratio as a predictor of outcome in fetuses with isolated left congenital diaphragmatic hernia at gestation outside 24–26 weeks. Am J Obstet Gynecol. 2007;197(1):30 e1–7.
Jani J, et al. Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007;30(1):67–71.
Paek BW, et al. Congenital diaphragmatic hernia: prenatal evaluation with MR lung volumetry–preliminary experience. Radiology. 2001;220(1):63–7.
Cordier AG, et al. Stomach position in prediction of survival in left-sided congenital diaphragmatic hernia with or without fetoscopic endoluminal tracheal occlusion. Ultrasound Obstet Gynecol. 2015;46(2):155–61.
Basta AM, et al. Fetal stomach position predicts neonatal outcomes in isolated left-sided congenital diaphragmatic hernia. Fetal Diagn Ther. 2016;39(4):248–55.
Cordier AG, et al. Stomach position versus liver-to-thoracic volume ratio in left-sided congenital diaphragmatic hernia. J Matern Fetal Neonatal Med. 2015;28(2):190–5.
Sista AK, Filly RA. Paradoxical movement of abdominal contents: a real-time sonographic finding indicating a congenital diaphragmatic hernia. J Ultrasound Med. 2007;26(11):1617–9.
Morgan TA, Basta A, Filly RA. Fetal stomach and gallbladder in contact with the bladder wall is a common ultrasound sign of stomach-down left congenital diaphragmatic hernia. J Clin Ultrasound. 2017;45(1):8–13.
Le LD, et al. The congenital diaphragmatic hernia composite prognostic index correlates with survival in left-sided congenital diaphragmatic hernia. J Pediatr Surg. 2012;47(1):57–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Morgan, T.A., Shum, D.J., Basta, A.M. et al. Prognosis in Congenital Diaphragmatic Hernia Diagnosed During Fetal Life. J. Fetal Med. 4, 57–63 (2017). https://doi.org/10.1007/s40556-017-0124-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40556-017-0124-4