Abstract
Background
Posterior ring apophysis fracture (PRAF), accompanied with lumbar disc herniation (LDH), is a rare occurrence. Owing to its rarity, there is no consensus on the treatment strategy for this condition. Differences mainly encompass the type of decompression method, the need for additional spinal fusion, the need for apophysis fragments or/and disc materials removal, and long-term efficacy, particularly, compared to LDH alone. Hence, the aim of this study was to describe a rare instance of PRAF with LDH in a 12-year-old professional diver, who was successfully treated with percutaneous endoscopic interlaminar discectomy (PEID), and to initiate a discussion involving several meaningful and related factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior ring apophysis fractures (PRAF), accompanied with lumbar disc herniation (LDH), is relatively uncommon [1]. Severe PRAF will increase the risk of spinal deformity in growing children [2]. Due to the persistence of bone compression, the outcome of conservative treatment is often poor [3]. When conservative therapy is considered ineffective, surgical intervention is advocated [3]. The goal of a PRAF with LDH-correcting operation is to relieve symptoms, with minimal surgical trauma, while enabling the patient to rapidly return to normal physical activity [3, 4]. However, the unique physiological characteristics of pediatric patients mandate the PRAF treatment to possess certain distinctive characteristics, and be more minimally invasive. Therefore, here, we report a rare case of PRAF with LDH in a 12-year-old professional diver, who was successfully treated with PEID.
Case presentation
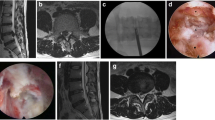
A 12-year-old male professional diver suffered from lower back pain and right lower limb radiculopathy for over 9 months. Apart from his father, who experienced LDH, there were no other diseases reported in the family. Physical examination: The right-straight-leg-raise test was positive and muscle strength of the right lower limb decreased slightly. The preoperative imaging demonstrated obvious L5/S1 level ring apophysis fractures with LDH (Fig. 1).
Surgical intervention
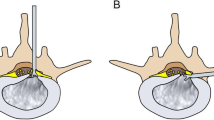
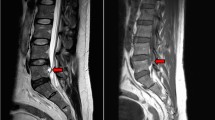
The patient was placed in a prone position on a radiolucent operating table and was provided with local anesthesia. The C-arm X-ray fluoroscopy was used to confirm the operative segment (Fig. 2a). The 18 G needle trajectory was introduced with its tip pointed at the lateral edge of the interlaminar window (Fig. 2b, c). Once the puncture needle reached the appropriate location, the contrast medium was injected (Fig. 2d). The needle was then removed, with a 1-mm-diameter guide wire inserted, and a dilator was introduced with its tip puncturing through the surface of the ligamentum flavum (Fig. 2e). A beveled working sheath was then inserted through the dilator with its beveled opening toward the spinal canal (Fig. 2f, g). Subsequently, an endoscope was introduced through the working cannula. Different types of forceps were employed for decompression, and then the traversing nerve root was visualized (Fig. 2h). The shoulder and axillary sides of the nerve roots were explored, prior to the removal of the working channel and endoscope. The patient’s straight-leg-raise test value increased from 50 to 90° after PEID. Although asymptomatic residual disc tissue was noted on magnetic resonance imaging (MRI) at the 3-month follow-up post operation (Fig. 3), the patient was able to return to his original high level of activity, without any residual lower back pain at the 6-month follow-up post operation. No complications were observed during the follow-ups.
Discussion and conclusions
PRAF is a rare etiology of back pain in adolescents and young adults, and it is, unfortunately, ignored by many surgeons [1, 3]. Trauma is considered a significant causative factor in about 50% of children and adolescents [1, 5]. The main pathogenesis of the presented case included ring apophysis, and incompletely fused vertebral endplate following high-intensity dive training. PRAF mainly occurs at the L4-5 and L5-S1 disc levels [1, 3, 5]. PRAF diagnosis primarily depends on computed tomography (CT), and it can be classified into four sub-groups [3, 6]. Early surgical intervention is advocated for patients with persistent symptoms. Laminectomy or semi-laminotomy, along with discectomy via the posterior approach, is a strongly recommended surgical procedure [3]. Different approaches are chosen to reach this principle, such as classical microdiscectoms [3], tubular microdiscectomy (TMD) [7], and percutaneous endoscopic discectomy (PED) [6]. The surgical trauma and dual scars caused by classical microdiscectomy are the greatest challenges for patients at the present time [6]. TMD can achieve more extensive bone resection, which is especially applicable to the central fragment fractures (i.e., types I, II, and IV), which can eventually lead to either spinal canal or intervertebral foramen stenosis [3, 6]. Our patient presented with a unilateral lesion and was classified as a type III. Hence, a unilateral semi-laminotomy or laminectomy could have achieved satisfactory results [6]. PEID was previously reported as a treatment option for type III PRAF in young adults, and it possesses the characteristics of markedly reduced epidural scar, iatrogenic injury, and surgical trauma [6]. Therefore, PEID offers more advantages in treating type III PRAF than TMD. It is not mandatory to remove the separated fragments because there is no difference in clinical results [8]. Most authors recommended that herniated discs must be removed [9, 10]. However, few authors suggested that discectomy must not be performed in pediatric patients, particularly, if they do not display degenerative disc disease [3]. Our recommendation was that discectomy must be considered, based on age and MRI findings. Therefore, limited nucleus pulposus removal was performed in our patient. Zheng et al. reported that over 90% of PRAF patients achieve good or excellent results at the 2-year follow-up after PEID [6]. However, few scholars are attentive to the surgical effect of PRAF, accompanied with LDH, relative to LDH alone. Following a comprehensive review of available literature, we discovered that patients with PRAF, accompanied with LDH, exhibit equal long-term clinical prognoses and postoperative complications, compared to LDH patients alone [8, 11].
In summary, PEID is an optimal approach for treatment of PRAF with LDH (type III) in a pediatric diver.
Availability of data and materials
The original contributions generated for the study are included in the article/Supplementary Material, and further inquiries can be directed to the corresponding author.
Abbreviations
- PRAF:
-
Posterior ring apophysis fracture
- LDH:
-
Lumbar disc herniation
- PEID:
-
Percutaneous endoscopic interlaminar discectomy
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- TMD:
-
Tubular microdiscectomy
- PED:
-
Percutaneous endoscopic discectomy
References
Kadam G, Narsinghpura K, Deshmukh S et al (2017) Traumatic lumbar vertebral ring apophysis fracture with disk herniation in an adolescent[J]. Radiol Case Rep 427–430. https://doi.org/10.1016/j.radcr.2016.11.026
Lei D, Liu Z (2010) A review of current treatment for lumbar disc herniation in children and adolescents[J]. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 19(2):205. https://doi.org/10.1007/s00586-009-1202-7
Wu X, Ma W, Du H et al (2013) A review of current treatment of lumbar posterior ring apophysis fracture with lumbar disc herniation[J]. Eur Spine J 22(3):475–488. https://doi.org/10.1007/s00586-012-2580-9
Albeck MJ, Madsen FF, Wagner A et al (1991) Fracture of the lumbar vertebral ring apophysis imitating disc herniation[J]. Acta Neurochir 113(1–2):52–56. https://doi.org/10.1007/BF01402115
Zamani MH, Macewen GD (1982) Herniation of the lumbar disc in children and adolescents.[J]. J Pediatr Orthop 2(5):528–33. https://doi.org/10.1097/01241398-198212000-00012
Zheng ZZ, Tu Z, Li Y et al (2018) Full-endoscopic lumbar discectomy for lumbar disc herniation with posterior ring apophysis fracture: a retrospective study[J]. World Neurosurgery. https://doi.org/10.1016/j.wneu.2018.12.054
Montejo JD et al (2018) Tubular approach to minimally invasive microdiscectomy for pediatric lumbar disc herniation[J]. Journal of neurosurgery. Pediatrics. https://doi.org/10.3171/2017.11.PEDS17293
Shirado O, Yamazaki Y, Takeda N et al (2005) Lumbar disc herniation associated with separation of the ring apophysis: is removal of the detached apophyses mandatory to achieve satisfactory results?[J]. Clin Orthop Relat Res 431(431):120–128. https://doi.org/10.1111/j.1472-765X.2005.01712.x
Epstein NE (1992) Lumbar surgery for 56 limbus fractures emphasizing noncalcified type III lesions.[J]. Spine 17(12):1489–96. https://doi.org/10.1097/00007632-199212000-00008
Chang CH, Lee ZL, Chen WJ et al (2008) Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation.[J]. Spine 33(16):1750. https://doi.org/10.1097/BRS.0b013e31817d1d12
Adebayo A, Balogun T, Yakubu O (2007) Microendoscopic discectomy for lumbar disc herniation with bony fragment due to apophyseal separation[J]. Minim Invasive Neurosurg 50(06):335–339. https://doi.org/10.1055/s-2007-993202
Acknowledgements
We express our sincere gratitude to the patient and his parents for their support.
Author information
Authors and Affiliations
Contributions
Hui Wu performed the literature search and collection and drafted the manuscript. Sikuan Zheng supervised and participated in the literature review. Dingwen He and Xigao Cheng completed all examinations and confirmed the final diagnosis. All authors read, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures performed in this case report were in accordance with the ethical standards of the institution and the 1964 Helsinki Declaration. Informed consent for participation was obtained from the patient and his parents.
Consent for publication
Written informed consent was obtained from the patient and his parents for publication of this case report and accompanying images and pictures.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, H., Zheng, S., He, D. et al. Percutaneous endoscopic interlaminar discectomy for posterior ring apophyseal fracture accompanied with lumbar disc herniation in a 12-year pediatric diver: a case report. Childs Nerv Syst 39, 275–278 (2023). https://doi.org/10.1007/s00381-022-05605-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05605-5