Abstract
Background
Discal cyst, a rare disease with unclear pathogenesis, exhibits symptoms similar to lumbar disk herniation. Currently, there is no consensus on the optimal treatment for this condition.
Case presentation
This report presents the clinical efficacy of the percutaneous endoscopic interlaminar approach surgery technique in patients diagnosed with lumbar 4–5 discal cyst. The patient exhibited sub-acute radiculopathy in the left leg accompanied by weakness of the extensor hallucis longus. Magnetic resonance imaging of the lumbar spine confirmed the presence of lumbar discal cysts, which exerted compression on the traversing nerve root. Surgical treatment involved performing percutaneous endoscopic interlaminar approach surgery without additional discectomy under general anesthesia. The symptoms were immediately alleviated following the removal of the discal cysts, and the weakness in the toe improved the day after the surgery. No recurrent symptoms or complications were observed during the 6-month follow-up period.
Conclusion
Based on our findings, we posit that percutaneous interlaminar endoscopic surgery represents a safe, minimally invasive, and appropriate approach for treating discal cysts.
Similar content being viewed by others
Introduction
Discal cysts are exceedingly uncommon intraspinal extradural cysts that establish communication with the intervertebral disc. These cysts pose a diagnostic challenge in distinguishing them from other sources of low back pain and radiculopathy [1]. Jung Won Park et al. [2] reported on 27 patients who have discal cysts, revealing a mean patient age of 32.5 ± 14.4 years, with a substantial majority of male patients (92.6%) female patient (7.4%), and the most prevalent location being L4-5 (55.6%).Nonetheless, due to the extreme rarity of discal cysts and the scarcity of literature references, comprehensive information regarding the natural progression of these lesions remains incomplete, leading to ongoing controversies in their management.
The full endoscopic surgery interlaminar approach is a minimally invasive surgical technique that preserves the integrity of the back muscles, facilitating rapid postoperative recovery for patients. Compared to conventional open surgery, full endoscopic surgery offers a swifter and more straightforward postoperative rehabilitation process. This report details the successful excision of a discal cyst utilizing the full endoscopic surgery interlaminar technique.
Medical report
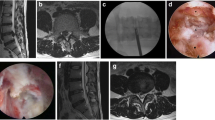
A male patient, aged 42, presented with a persistent and severe pain in the left lower buttock, radiating down to the left leg, which he has been experiencing for a duration of one month. The onset of the pain occurred after playing golf. The patient noted a significant decrease in the strength of his left leg and consequently decided to seek medical attention at the hospital. Upon physical examination, weakness was observed in the left extensor hallucis longus muscle, graded at 2/5, as well as in the left tibialis anterior muscle, graded at 4/5. Lumbar radiographs revealed no abnormalities in terms of spinal segmental stability or deformity. However, an oval-shaped cyst with a prominent high signal intensity was clearly visible behind the L5 vertebral body in the lower lumbar region on the MRI scan (see Fig. 1). The T1-weighted images showed low signal intensity, while the T2-weighted images exhibited high signal intensity, consistent with the characteristics of a cyst. Further examination through an axial cut of the MRI scan demonstrated a downwardly compressed cyst at the left L5 level, impinging on the traversing nerve (see Fig. 2). The diagnosis was confirmed as a lumbar discal cyst at the L4-5 level. Due to the rapidly progressing neurological deficits, a surgical intervention was recommended to the patient. We advised a full endoscopic interlaminar approach to minimize the risk of back muscle injury and maximize the visual perspective during cyst manipulation. Upon endoscopic examination, following the incision of the ligamentum flavum, a thin-walled cystic lesion containing gelatinous material was discovered (see Fig. 3). The cyst wall was firmly attached to the disc, which was completely excised by severing its connection with the annulus fibrosus (see Fig. 4). There is a low level of adherence observed in the cyst attached to the nerve root, and the level of vascularity in the cyst is also minimal. The duration of this surgical procedure is approximately two hours. The patient experienced immediate relief from the symptoms following surgery, and no complications were observed during the perioperative period. Consequently, the patient was discharged with complete resolution of his complaints. At the one-month follow-up, all motor functions had fully recovered to grade 5. Subsequently, at the 1-year follow-up, the patient remained asymptomatic without any recurrence of back pain.
Lumbar spinal sagittal cut MRI of the patient demonstrating the L4-L5 discal cyst, with prominent compression of the left L5 nerve root. a Sagittal T2-weighted image shows an ovoid lesion with a hyperintense center plus hypointense rim (red arrow). b Sagittal T1-weighted image shows an ovoid lesion with low signal intensity (red arrow)
Lumbar spinal axial cut MRI of the patient demonstrating the L4-L5 discal cyst, with prominent compression of the left L5 nerve root a axial MRI shows no compression of nerve at disk area. b Axial MRI at L5 vertebral body shows compression of L5 traversing nerve at vertebral body L5 level (red arrow)
Discussion
Discal cysts of the lumbar spine are exceedingly rare lesions, with only a limited number of articles in the literature addressing these lesions as individual case reports. The discal cyst establishes communication with the intervertebral disk [3]. Originally, Kono et al. provided the first description of intraspinal extradural cysts as well-defined homogeneous cysts situated in the ventrolateral extradural space, displacing the dural sac dorsomedially and communicating with the intervertebral disk [4]. The pathogenesis of discal cysts remains uncertain. Presently, two hypotheses have been proposed. Toyama et al. [3] and Chiba et al. [1] proposed that an epidural hematoma is initially formed by hemorrhage from the epidural venous plexus, resulting from disk injury. The discal cyst subsequently develops due to incomplete resorption of the hematoma. This theory is supported by reports indicating the presence of hemosiderin deposits in the majority of studied cysts. However, this hypothesis fails to explain the connecting stalk between the intervertebral disk and the cyst through an annular defect. Kono et al. [4] proposed a theory involving mechanical stress-induced focal degeneration of the posterior disk wall, followed by fluid accumulation, reactive pseudomembrane formation surrounding the fluid collection, and subsequent development of the discal cyst.
Chiba et al. [5] summarized the characteristics of discal cysts as follows: (1) clinical symptoms of a unilateral single nerve root lesion, (2) occurrence at a slightly younger age and at higher intervertebral levels compared to typical disk herniation, (3) minimal degeneration of the affected disk observed on imaging studies, (4) communication between the cyst and corresponding intervertebral discs detected on discograms, accompanied by severe radiating pain in the affected leg during injection, (5) a cyst containing bloody to clear serous fluid, and (6) absence of disk materials or a specific lining cell layer observed on histological examination. All these characteristics were observed in our patients. MRI is the preferred imaging modality for visualizing discal cysts. Lee et al. [6] described the MRI features of discal cysts as a ventrolateral extradural cystic mass attached to a lumbar intervertebral disc, exhibiting rim enhancement of its wall on contrast-enhanced MRI, with occasional spread of the mass into the lateral recess [7]. The symptoms of a discal cyst can vary [8]. Due to the cyst's ventromedial location in relation to the nerve root, causing compression on the root dorso-laterally, symptoms and signs are indistinguishable from those of a lumbar disk herniation, resulting in radiculopathy and nerve root tension.
Treatment options for disk cysts comprise conservative and surgical approaches. Conservative treatments encompass rest, pain management, physical therapy, selective nerve root block, among others [9]. Surgical treatments for discal cysts include CT-guided cyst aspiration, microscopic cystectomy, and endoscopic cystectomy [9,10,11,12]. Although percutaneous CT-guided puncture and steroid injection have been reported as potential treatments for discal cysts [13], the possibility of recurrence after CT-guided puncture and aspiration still exists. Therefore, we lean towards performing complete resection of discal cysts [5, 10]. Surgical techniques for treating discal cysts involve endoscopic and microscopic cyst resection. Recently, Matsumoto et al. [14] and Ha et al. [15] outlined the advantages of endoscopic techniques in cyst resection. The major benefit of full-endoscopic decompression is the complete removal of cysts while causing minimal disruption to ligamentous and bony structures. Additionally, this technique requires an incision of less than 1 cm, resulting in early ambulation and a shortened hospital stay [16]. Jin-Sung Kim [17] has presented a report on a minimally invasive surgical technique utilizing a side-firing Ho:YAG laser. This technique has demonstrated favorable postoperative results.
Upon removal of the discal cyst during the surgical intervention, it becomes essential to verify the connection between the disk and the capsule of the discal cyst. The critical step for achieving successful outcomes lies in excising both the capsule of the discal cyst and the disc's stalk [10, 17]. Some relevant studies have solely focused on removing the discal cyst without accompanying discectomy, resulting in favorable surgical outcomes and subsequent follow-ups revealing no instances of recurrence [15]. We believe that the decision to perform concurrent discectomy warrants careful consideration. Previous reports suggest that minimally invasive discectomy can potentially lead to spinal instability [16]. Therefore, we opted to solely eliminate the discal cyst without conducting discectomy. Subsequently, the patient experienced no recurrence of the cyst postoperatively. Based on our surgical experience and clinical results, we assert that cyst removal alone may represent an effective treatment method for lumbar discal cysts.
However, it should be noted that no previous studies have documented the utilization of an endoscopic interlaminar approach for discal cyst treatment. Given the similarity of symptoms and location between a discal cyst and lumbar disk herniation, we considered employing a minimally invasive percutaneous endoscopic interlaminar technique for treating the discal cyst. The procedure was successfully performed, resulting in immediate improvement of radiculopathy. One limitation of this study pertains to the absence of postoperative imaging, which can be attributed to the patients' refusal to undergo MRI scans as they do not exhibit any symptoms. Another limitation arises from the unavailability of histopathological analysis in this particular case, which is primarily due to financial constraints.
Conclusion
In the present report, we conducted a minimally invasive procedure employing the percutaneous endoscopic interlaminar approach to successfully address a discal cyst. A 6-month follow-up revealed no recurrences. Hence, we propose that properly selected cases of discal cysts can be effectively treated through the percutaneous endoscopic interlaminar approach, which offers numerous advantages. This approach may result in reduced postoperative spinal instability compared to conventional open surgery, along with minimal soft tissue trauma and bleeding, expedited rehabilitation, and shorter hospital stays. The authors hold the belief that this technique presents a viable and secure alternative when compared to both open surgery and microscope-assisted procedures.
Availability of data and materials
Not available.
Abbreviations
- CT:
-
Computer tomography
- L:
-
Lumbar
- MRI:
-
Magnetic resonance imaging
References
Chiba K, et al. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: discal cyst. Spine. 2001;26(19):2112–8.
Park JW, et al. Surgical treatment of lumbar spinal discal cyst: is it enough to remove the cyst only without following discectomy? Neurol Med Chir. 2019;59(6):204–12.
Toyama Y. Pathogenesis and diagnostic title of intraspinal cyst communicating with intervertebral disc in the lumbar spine. Rinsho Seikei Geka. 1997;32:393–400.
Kono K, et al. Intraspinal extradural cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. Am J Neuroradiol. 1999;20(7):1373–7.
Aydin S, et al. Discal cysts of the lumbar spine: report of five cases and review of the literature. Eur Spine J. 2010;19(10):1621–6.
Lee HK, et al. Discal cyst of the lumbar spine: MR imaging features. Clin Imaging. 2006;30(5):326–30.
Koga H, et al. Percutaneous CT-guided puncture and steroid injection for the treatment of lumbar discal cyst: a case report. Spine. 2003;28(11):E212–6.
Jeong GK, Bendo JA. Lumbar intervertebral disc cyst as a cause of radiculopathy. Spine J. 2003;3(3):242–6.
Arslan E, et al. Which treatment method should be preferred for lumbar discal cysts? A case report and a review of the literature. Neurol Neurochir Pol. 2014;48(1):71–5.
Jha, S.C., et al., Percutaneous endoscopic discectomy via transforaminal route for discal cyst. Case Rep Orthoped. 2015;2015.
Dasenbrock, H.H., et al., Successful treatment of a symptomatic L5/S1 discal cyst by percutaneous CT-guided aspiration. Surg Neurol Int. 2010;1.
Gadjradj PS, Harhangi BS. Percutaneous transforaminal endoscopic discectomy for lumbar disk herniation. Clin Spine Surg. 2016;29(9):368–71.
Haider SJ, et al. Symptomatic lumbar facet synovial cysts: clinical outcomes following percutaneous CT–guided cyst rupture with intra-articular steroid injection. J Vasc Interv Radiol. 2017;28(8):1083–9.
Matsumoto M, et al. Microendoscopic resection of lumbar discal cysts. Minim Invasive Neurosurg. 2010;53(02):69–73.
Ha SW, et al. Clinical outcomes of percutaneous endoscopic surgery for lumbar discal cyst. J Korean Neurosurg Soc. 2012;51(4):208–14.
Ishii K, et al. Endoscopic resection of cystic lesions in the lumbar spinal canal. A report of two cases. Minim Invasive Neurosurg. 2005;48(04):240–3.
Kim J-S, et al. Removal of a discal cyst using a percutaneous endoscopic interlaminar approach: a case report. Photomed Laser Surg. 2009;27(2):365–9.
Acknowledgements
To the spine department professors and colleges, for their assistance. To the patients and their relative for participating in the research.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors provided comments on the manuscript at various stages of development. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It was approved by the ethics committee of Bumrungrad clinical research center.
Consent for publication
Informed consent was obtained from the patient included in this study.
Competing interests
No competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kasempipatchai, P., Kesornsak, W. & Kuansongtham, V. Removal of discal cyst using percutaneous full endoscopic via interlaminar route: a case report. Egypt J Neurosurg 38, 48 (2023). https://doi.org/10.1186/s41984-023-00231-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00231-y