Abstract
Glioblastoma (GBM) is an exceptionally aggressive brain tumor with a dismal prognosis, demanding fast and precise classification as a base for patient-specific treatment strategies. Here, we report on an adolescent patient with a histologically bona fide GBM that shows a molecular methylation profile suggesting a low-grade glioma-like subgroup. Despite an early relapse, intolerance of temozolomide, and change of treatment strategy to vinblastine and valproic acid (VPA), the patient is now in good clinical condition after more than 5 years since initial diagnosis. This case stresses the merit of methylation array data for clinical prognosis and treatment planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-grade glioma accounts for 10–15% of pediatric CNS tumors [1]. Gross surgical resection and radiotherapy are essential for survival. A rational base for chemotherapy treatment, however, is still missing [2]. The current German HIT HGG 2013 study investigates an additive effect of valproic acid (VPA) to temozolomide and radiotherapy [3]. But despite multimodal therapy approaches, the prognosis of pediatric glioblastoma patients with high-grade GBM is extremely poor. As prognosis varies significantly in dependence of clinical and biological features, identification of reliable prognostic parameters for treatment response and clinical outcome of individual patients is urgent [4].
DNA methylation profiling contributes to define molecular subgroups in pediatric GBM that are clinically and prognostically important [5, 6]. Two independent investigations in 2015 and 2017 describe that a subset of H3/IDH wild-type GBM showed methylation profiles resembling low-grade glioma (LGG-like) or pleomorphic xanthoastrocytoma (PXA-like). The LGG-like tumors occurred mainly in infants under the age of 1 year and showed a significantly better prognosis than other H3/IDH wild-type GBM [5, 6].
Case report
The 15-year-old female patient presented at the Department of Pediatric Hematology and Oncology, University Medical Center Hamburg-Eppendorf with several weeks of frontotemporal headache and was admitted to the hospital with transient weakness and paresthesia of the left extremities. The cranial MRI showed a right-frontal tumor with surrounding edema (Fig. 1a, f).
Cranial MRIs before and during treatment: T2 fluid-attenuated inversion recovery (FLAIR) a–e and contrast-enhanced T1 weighted f–j MRI sequences. Upon initial diagnosis a, f: heterogeneous mass on the right frontal lobe with perifocal edema a, ring enhancement f, a slight midline deviation and the presence of satellite lesions f. Post-operative imaging b, g: 2 days after tumor resection showing typical perifocal edema b and a focal nodular enhancement g at the anteromedial resection margin (broad arrow) suggesting possible residual tumor. Upon relapse 7 months after tumor resection c, h: frontal defect with discrete perifocal edema c and relapsing contrast-enhancing lesions (triangles) adjacent to the resection area h. Upon progression d, i: larger post-resection parenchyma defect on the right frontal lobe after repeated tumor resection and progressive hyperintense signal in the FLAIR d in the contralateral cingulate gyrus (arrow). Note the absence of enhancement (star) in the post-contrast images i. Seven months after progression, MRI images show stable disease e, j: stable non-enhancing (star) FLAIR hyperintensities (arrow) in the left cingulate gyrus e
After macroscopically complete tumor resection, a small residual tumor was suspected in the postoperative MRI (Fig. 1b, g). Histomorphologic assessment by local and reference pathologists confirmed the diagnosis of IDH-mutant GBM. The tumor region was irradiated with a target volume dose of 60 Gy following the HIT HGG-2007 protocol with concomitant daily temozolomide, followed by a temozolomide monotherapy in monthly cycles of 5 days (treatment overview in Fig. 2). Seven months after diagnosis, the tumor reoccurred (Fig. 1c, h). After the second surgical resection, a residual tumor at the dorsal resection border could not be excluded. We initiated adjuvant therapy with oral valproic acid (VPA) and due to slight progression of the residual mass, we added treatment with weekly vinblastine. At the time of 4.5 years after the first diagnosis, Vinblastine and VPA dosage remained unchanged but vinblastine applications were stretched to 3-week intervals in order to reduce adverse reactions.
Time line showing patient’s treatment. Chemotherapeutical treatment: oral temozolomide (green) was given concomitant to radiotherapy and then as a monotherapy first 150 mg/m2/day (5 days every 4 weeks), then 100 mg/m2/day and was terminated due to severe side effects. Valproic acid (blue) 300 mg/m2/day in 2 daily oral doses and vinblastine 3 mg/m2 treatment (red) was added first as weekly infusions and then in longer intervals of 2–3 weeks. Dosages remained unchanged for the entire treatment period
Five years after initial diagnosis and 6 months after decreasing the treatment intensity, MRI imaging showed a progressive hyperintense signal in the FLAIR sequence in the contralateral cingulate gyrus, indicating a new non-enhancing tumor lesion (Fig. 1d, i). The patient was clinically well and very hesitant towards intensified chemotherapy or surgery. Therefore, and with respect to the slow progression, we decided to continue the previous treatment schedule with VPA and vinblastine and to closely surveille the tumor by MRI imaging. The tumor showed no further progression on MRI for the following 7 months (Fig. 1 e, j).
Neuropathological and molecular workup
We investigated the biological characteristics of the tumors in more detail (Figs. 3 and 4). The initial histology showed a glial tumor with vascular proliferation, areas of necrosis, and increased proliferation. Tumor cells were positive for GFAP and MAP2c and negative for IDH-1 (R132H) and mutation-specific Histone H3. DNA sequencing ruled out mutations in codon 27 or 34 of the H3F3A gene.
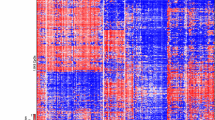
t-SNE analysis of the methylation profile suggested similarity to low-grade glioma: t-SNE plot including glioblastoma and low-grade glioma from the Heidelberg brain tumor classifier as published by Capper et al. [7]. Primary and relapse tumor of our patient depicted in red. Exemplary LGG-like glioblastoma from Mackay et al. depicted in orange [6]
We conducted Illumina Human Methylation 850 K Bead Chip array analysis of primary and relapse tumor tissue. Both tumors showed an unmethylated MGMT promoter. The tumor did not show a definite match with any of the reference brain tumor entities on the Heidelberg brain tumor classifier [7]. The initial tumor had a calibrated score of 0.4, and the relapse tumor did not score above 0.3. We then performed t-distributed stochastic neighbor embedding (t-SNE) analysis alongside 2,801 brain tumor cases as published [7]. Initial and relapse tumor clustered closely with low-grade glioma, comparable to published methylation data of LGG-like GBM by Mackay et al. [6] (Fig. 4).
Discussion
Despite an early relapse and a residual tumor, the adolescent patient remained with stable disease for over 5 years under treatment with vinblastine and VPA.
Weekly vinblastine has previously proven successful in treatment of recurrent LGG [8]. Vinca alkaloids showed activity in early chemotherapy studies [9, 10] and are a key element in previous and current treatment strategies [11].
VPA is a well-established anti-epileptic drug but was also found to induce an anti-tumor response in vitro and in GBM patients and has been proposed to have sensitizing effects during radiation therapy [12,13,14,15]. Due to promising preclinical and clinical reports, treatment with VPA is currently tested in the running German HIT-HGG 2013 trial [3].
Methylation analysis did not detect a clear match with any brain tumor methylation class, but t-SNE analysis of the methylation profile suggested similarity to low-grade glioma. The correct diagnosis of glioblastoma is strongly supported by the aggressive tumor biology and the clear histological features. However, the methylation profile in combination with the good response to VPA and Vinblastine treatment point towards this glioblastoma having some LGG-like features as described previously [5, 6].
Whether the good treatment response of our patient is due to an intrinsically less aggressive tumor biology, as suggested by the LGG-like methylation profile, or if the applied treatment strategy also contributed to the long-term survival remains unknown and will have to be put into context with detailed clinical data from comparable patients.
With respect to the devastating prognosis of GBM, we stress the importance of methylation profiling for risk stratification and treatment. Adolescent patients with GBM clustering in the LGG-like subgroup and an above-average prognosis might be more common than suggested by previous reports. Clustering of tumors in the LGG-like subgroup might even supply evidence for alternative treatment strategies including vinblastine and VPA.
References
Ostrom QT, Gittleman H, Liao P et al (2014) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol :16 Suppl 4:iv1–63
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Kramm C (2018) International cooperative Phase III trial of the HIT-HGG study group for the treatment of high grade glioma, diffuse intrinsic pontine glioma, and gliomatosis cerebri in children and adolescents < 18 years. ClinicalTrials.gov Identifier: NCT03243461; Start Date July 17, 2018
Pollack IF, Agnihotri S, Broniscer A (2019) Childhood brain tumors: current management, biological insights, and future directions. J Neurosurg Pediatr 23:261–273
Korshunov A, Ryzhova M, Hovestadt V et al (2015) Integrated analysis of pediatric glioblastoma reveals a subset of biologically favorable tumors with associated molecular prognostic markers. Acta Neuropathol 129:669–678
Mackay A, Burford A, Carvalho D et al (2017) Integrated molecular meta-analysis of 1,000 pediatric high-grade and diffuse intrinsic pontine glioma. Cancer Cell 32:520-537.e5
Capper D, Jones DTW, Sill M et al (2018) DNA methylation-based classification of central nervous system tumours. Nature 555:469–474
Bouffet E, Jakacki R, Goldman S et al (2012) Phase II study of weekly vinblastine in recurrent or refractory pediatric low-grade glioma. J Clin Oncol 30:1358–1363
Packer RJ, Ater J, Allen J et al (1997) Carboplatin and vincristine chemotherapy for children with newly diagnosed progressive low-grade gliomas. J Neurosurg 86:747–754
Rosenstock JG, Evans AE, Schut L (1976) Response to vincristine of recurrent brain tumors in children. J Neurosurg 45:135–140
Boesten T, Gerber NU, Kandels D et al (2017) Management of primary thalamic low-grade glioma in pediatric patients: results of the multicenter treatment studies HIT-LGG 1996 and SIOP-LGG 2004. Neurooncol Pract 4:29–39
Barker CA, Bishop AJ, Chang M, Beal K, Chan TA (2013) Valproic acid use during radiation therapy for glioblastoma associated with improved survival. Int J Radiat Oncol Biol Phys 86:504–509
Chen Y, Tsai Y-H, Tseng SH (2012) Valproic acid affected the survival and invasiveness of human glioma cells through diverse mechanisms. J Neurooncol 109:23–33
Masoudi A, Elopre M, Amini E et al (2008) Influence of valproic acid on outcome of high-grade gliomas in children. Anticancer Res 28:2437–2442
Wolff JEA, Kramm C, Kortmann RD et al (2008) Valproic acid was well tolerated in heavily pretreated pediatric patients with high-grade glioma. J Neurooncol 90:309–314
Funding
Open Access funding enabled and organized by Projekt DEAL. C.K. was sponsored by a fellowship of the University Cancer Center Hamburg (UCCH). Further funding from the Fördergemeinschaft Kinderkrebszentrum Hamburg is provided to U.S. The HIT-MED trial center in Hamburg and the reference center for Neuroradiology in Würzburg are supported by the Deutsche Kinderkrebsstiftung.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kresbach, C., Bronsema, A., Guerreiro, H. et al. Long-term survival of an adolescent glioblastoma patient under treatment with vinblastine and valproic acid illustrates importance of methylation profiling. Childs Nerv Syst 38, 479–483 (2022). https://doi.org/10.1007/s00381-021-05278-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05278-6