Abstract
Objective
To describe the first pediatric case in the literature of neuropathic inguinal pain secondary to iatrogenic nerve injury that occurred during a laparoscopic appendectomy, detailing clinical and morphological findings before and after surgery. The literature on adult patients is reviewed and pathophysiological, therapeutic, and prognostic factors are discussed.
Clinical presentation
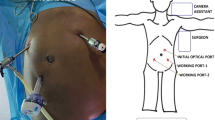
A 14-year-old female patient presented with a history of a laparoscopic appendectomy 3 years previously. Three months post-operatively, she developed progressively worsening neuropathic inguinal pain refractory to neuromodulators and several nerve blocks. Given her deterioration, poor response to conservative therapy, and clearly meeting the criteria for chronic post-operative inguinal pain (CPIP), surgical management was undertaken.
Results
Open surgery was performed through the previous incision, during which injury to a branch of the iliohypogastric nerve (IH) was confirmed. Neurolysis of the affected branch was performed, after which the patient experienced significant pain relief, resolution of allodynia, and reversal of skin hyperpigmentation. After discharge, analgesic therapy was gradually withdrawn and, ultimately, discontinued altogether.
Conclusions
Understanding the neuroanatomy of the inguinal region is an indispensable requirement for all surgeons operating in this region, to avoid complications including CPIP and optimize patient outcomes. Surgical management of CPIP can be effective for controlling severe pain in patients in whom conservative management has failed. Studies are needed in the pediatric population to identify specific characteristics of this entity in youth.






Similar content being viewed by others
References
Mackinnon SE (2015) The “border nerves”: iliohypogastric, ilioinguinal, and genitofemoral. In: Nerve Surgery, 1st edn. Thieme Publishers, New York, pp 345–354
Finkel DM (2000) Neuralgia residual cronica como complicacion postoperatoria de cirugia inguinal. Rev Arg Anest 58(1):35–41
Graham DS, MacQueen IT, Chen DC (2018) Inguinal neuroanatomy: implications for prevention of chronic postinguinal hernia pain. Int J Abdom Wall Hernia Surg 1:1–8
Konschake M, Zwierzina M, Moriggl B, Függer R, Mayer F, Brunner W, Schmid T, Chen DC, Fortelny R (2020) The inguinal region revisited: the surgical point of view: an anatomical-surgical mapping and sonographic approach regarding postoperative chronic groin pain following open hernia repair. Hernia 24(4):883–894. https://doi.org/10.1007/s10029-019-02070-z
Cirocchi R, Mercurio I, Nazzaro C, De Sol A, Boselli C, Rettagliata G, Vanacore N, Santoro A, Mascagni D, Renzi C, Lancia M, Suadoni F, Zanghì G, Palumbo P, Bruzzone P, Tellan G, Fedeli P, Marsilio F, D'Andrea V (2020) Dermatome mapping test in the analysis of anatomo-clinical correlations after inguinal hernia repair. BMC Surg 20(1):319. https://doi.org/10.1186/s12893-020-00988-1
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia. 22(1):1–165
Jacobs CJ, Steyn WH, Boon JM (2004) Segmental nerve damage during a McBurney’s incision: a cadaveric study. Surg Radiol Anat 26(1):66–69. https://doi.org/10.1007/s00276-003-0189-8
Epstein NE (2019) Review of risks and complications of extreme lateral interbody fusion (XLIF). Surg Neurol Int 10:237. https://doi.org/10.25259/SNI_559_2019
Zhang Z, Wang Y, Liu R, Zhao L, Liu H, Zhang J, Li G (2015) Systematic review and meta-analysis of single-incision versus conventional laparoscopic appendectomy in children. J Pediatr Surg 50(9):1600–1609. https://doi.org/10.1016/j.jpedsurg.2015.05.018
Lange JF, Wijsmuller AR, van Geldere D, Simons MP, Swart R, Oomen J, Kleinrensink GJ, Jeekel J, Lange JF (2009) Feasibility study of three-nerve-recognizing Lichtenstein procedure for inguinal hernia. Br J Surg 96(10):1210–1214. https://doi.org/10.1002/bjs.6698
Wijsmuller AR, Lange JF, Kleinrensink GJ, van Geldere D, Simons MP, Huygen FJ, Jeekel J, Lange JF (2007) Nerve- identifying inguinal hernia repair: a surgical anatomical study. World J Surg 31(2):414–420. https://doi.org/10.1007/s00268-006-0376-y
O’Dwyer PJ, Alani A, McConnachie A (2005) Groin hernia repair: postherniorrhaphy pain. World J Surg 29(8):1062–1065. https://doi.org/10.1007/s00268-005-7903-0
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367(9522):1618–1625. https://doi.org/10.1016/S0140-6736(06)68700-X
Reinpold W (2017) Risk factors of chronic pain after inguinal hernia repair: a systematic review. Innov Surg Sci 2(2):61–68. https://doi.org/10.1515/iss-2017-0017
Smeds S, Lofstrom L, Eriksson O (2010) Influence of nerve identification and the resection of nerves ’at risk’ on postoperative pain in open inguinal hernia repair. Hernia 14(3):265–270. https://doi.org/10.1007/s10029-010-0632-9
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, di Miceli D, Doglietto GB (2011) International guidelines for prevention and management of postoperative chronic pain following inguinal hernia surgery. Hernia. 15:239–249
Werner MU (2014) Management of persistent postsurgical inguinal pain. Langenbeck's Arch Surg 399(5):559–569. https://doi.org/10.1007/s00423-014-1211-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Quevedo Orrego, E., Robla Costales, J., Rodríguez Aceves, C. et al. Neuropathic inguinal pain due to nerve injury after a laparoscopic appendectomy: first pediatric case described in the literature. Childs Nerv Syst 37, 1825–1830 (2021). https://doi.org/10.1007/s00381-021-05177-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05177-w