Abstract
Background
Surgical strategy regarding nerve identification and resection in relation to chronic postoperative pain remains controversial. A central question is whether nerves in the operation field, when identified, should be preserved or resected. In the present study, the hypotheses that the identification and consequent resection of nerves ‘at risk’ have no influence on postoperative pain has been tested.
Methods
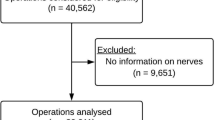
A single-centre study was conducted in 525 patients undergoing Lichtenstein hernioplasty. One surgeon (364 operations, Group A) consequently resected nerves ‘at risk’ for being injured and nine surgeons (161 operations, Group B) adhered to the general routine of nerve preservation. All cases were ambulatory surgery on anaesthetised patients and the groups were similar with regard to age, body mass index (BMI) and preoperative pain. Self-reported pain at 3 months was recorded on a 10-box visual analogue scale (VAS). The identification and resection of nerves were continuously registered. Statistical calculations were performed with Fisher’s exact test and ordinal logistic regression.
Results
There was no significant difference in the number of identified nerves in the two groups of patients (iliohypogastricus, P = 0.555; ilioinguinalis, P = 0.831; genital branch, P = 0.214). However, the number of resected nerves was significantly higher in Group A for the iliohypogastric nerve, P < 0.001, but not for ilioinguinalis, P = 0.064, and genital branch, P = 0.362. Non-identification of the ilioinguinal nerve correlated to the highest level of self-reported postoperative pain at 3 months. Patients in Group A, who had nerves ‘at risk’ resected from the operation field, reported significantly less postoperative pain at 3 months, P = 0.007.
Conclusion
This register study confirms the importance of nerve identification. Nerve resection strategy with the consequent removal of nerves ‘at risk’ gives a significantly better outcome in Lichtenstein hernioplasty.
Similar content being viewed by others
Notes
The Sergel Clinic has changed name to Medicinskt Centrum from January 1st, 2009.
References
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1988) Cause and prevention of postherniorrhaphy neuralgia: a proposed protocol for treatment. Am J Surg 155:786–790
Ravichandran D, Kalambe BG, Pain JA (2000) Pilot randomized controlled study of preservation or division of ilioinguinal nerve in open mesh repair of inguinal hernia. Br J Surg 87:1166–1167
Pappalardo G, Frattaroli FM, Mongardini M, Salvi PF, Lombardi A, Conte AM, Arezzo MF (2007) Neurectomy to prevent persistent pain after inguinal herniorraphy: a prospective study using objective criteria to assess pain. World J Surg 31:1081–1086
Rab M, Ebmer And J, Dellon AL (2001) Anatomic variability of the ilioinguinal and genitofemoral nerve: implications for the treatment of groin pain. Plast Reconstr Surg 108:1618–1623
Picchio M, Palimento D, Attanasio U, Matarazzo PF, Bambini C, Caliendo A (2004) Randomized controlled trial of preservation or elective division of ilioinguinal nerve on open inguinal hernia repair with polypropylene mesh. Arch Surg 139:755–758
Wijsmuller AR, van Veen RN, Bosch JL, Lange JFM, Kleinrensink GJ, Jeekel J, Lange JF (2007) Nerve management during open hernia repair. Br J Surg 94:17–22
Bartlett DC, Porter C, Kingsnorth AN (2007) A pragmatic approach to cutaneous nerve division during open inguinal hernia repair. Hernia 11:243–246
Kalliomäki ML, Meyerson J, Gunnarsson U, Gordh T, Sandblom G (2008) Long-term pain after inguinal hernia repair in a population-based cohort; risk factors and interference with daily activities. Eur J Pain 12:214–225
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Ravindran R, Bruce J, Debnath D, Poobalan A, King PM (2006) A United Kingdom survey of surgical technique and handling practice of inguinal canal structures during hernia surgery. Surgery 139:523–526
Dittrick GW, Ridl K, Kuhn JA, McCarty TM (2004) Routine ilioinguinal nerve excision in inguinal hernia repairs. Am J Surg 188:736–740
Mui WL, Ng CS, Fung TM, Cheung FK, Wong CM, Ma TH, Bn MY, Ng EK (2006) Prophylactic ilioinguinal neurectomy in open inguinal hernia repair: a double-blind randomized controlled trial. Ann Surg 244:27–33
Alfieri S, Rotondi F, Di Giorgio A, Fumagalli U, Salzano A, Di Miceli D, Ridolfini MP, Sgagari A, Doglietto G; Groin Pain Trial Group (2006) Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg 243:553–558
Lange JF, Wijsmuller AR, van Geldere D, Simons MP, Swart R, Oomen J, Kleinrensink GJ, Jeekel J, Lange JF (2009) Feasibility study of three-nerve-recognizing Lichtenstein procedure for inguinal hernia. Br J Surg 96(10):1201–1204
Wijsmuller AR, Lange JFM, Kleinrensink GJ, van Geldere D, Simons MP, Huygen FJPM, Jeekel J, Lange JF (2007) Nerve-identifying inguinal hernia repair: a surgical anatomical study. World J Surg 31:414–420
Wantz GE (1993) Testicular atrophy and chronic residual neuralgia as risks of inguinal hernioplasty. Surg Clin North Am 73:571–581
Cunningham J, Temple WJ, Mitchell P, Nixon JA, Preshaw RM, Hagen NA (1996) Cooperative hernia study. Pain in the postrepair patient. Ann Surg 224:598–602
Amid PK, Hiatt JR (2007) New understanding of the causes and surgical treatment of postherniorrhaphy inguinodynia and orchalgia. J Am Coll Surg 205(2):381–385
Malekpour F, Mirhashemi SH, Hajinasrolah E, Salehi N, Khoshkar A, Kolahi AA (2008) Ilioinguinal nerve excision in open mesh repair of inguinal hernia—results of a randomized clinical trial: simple solution for a difficult problem? Am J Surg 195:735–740
Zieren J, Rosenberg T, Menenakos Ch (2008) Impact of ilio-inguinal nerve excision on sexual function in open inguinal hernia mesh repair: a prospective follow-up study. Acta Chir Belg 108(4):409–413
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smeds, S., Löfström, L. & Eriksson, O. Influence of nerve identification and the resection of nerves ‘at risk’ on postoperative pain in open inguinal hernia repair. Hernia 14, 265–270 (2010). https://doi.org/10.1007/s10029-010-0632-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0632-9