Abstract
Objectives
To recognize the national trends in management of pediatric craniopharyngioma and to address the significant predictors of discharge disposition.
Methods
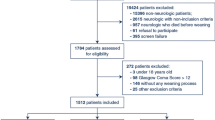
We utilized the Kids’ Inpatient Database (KID), a pediatric inpatient sample generated by the Healthcare Cost and Utilization Project (HCUP) triennially from 1997 to 2016.
Results
KID contains 2141 pediatric craniopharyngioma admissions. Patient demographics had no effect on discharge disposition. Based on the multivariable logistic regression analysis, we confirmed a significantly higher non-routine discharge rate among patients with hydrocephalus (P = 0.01). Patients who developed diabetes insipidus were at higher risk for non-routine discharge (P = 0.02). Admission of patients to a freestanding children’s hospital increased the likelihood of routine discharge (P = 0.001).
Conclusion
Hydrocephalus, diabetes insipidus, and admission to a freestanding children’s hospital are significant independent predictors of discharge disposition.


Similar content being viewed by others
References
Ali ZS, Lang SS, Kamat AR, Adappa ND, Palmer JN, Storm PB, Lee JY (2013) Suprasellar pediatric craniopharyngioma resection via endonasal endoscopic approach. Child’s Nerv Syst 29:2065–2070. https://doi.org/10.1007/s00381-013-2153-1
Bakhsheshian J, Jin DL, Chang KE, Strickland BA, Donoho DA, Cen S, Mack WJ, Attenello F, Christian EA, Zada G (2016) Risk factors associated with the surgical management of craniopharyngiomas in pediatric patients: analysis of 1961 patients from a national registry database. Neurosurg Focus 41:E8. https://doi.org/10.3171/2016.8.Focus16268
Barreca T, Perria C, Francaviglia N, Rolandi E (1984) Evaluation of anterior pituitary function in adult patients with craniopharyngiomas. Acta Neurochir 71:263–272
Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM (1998) The descriptive epidemiology of craniopharyngioma. J Neurosurg 89:547–551. https://doi.org/10.3171/jns.1998.89.4.0547
Burns EM, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, Faiz OD (2012) Systematic review of discharge coding accuracy. Journal of public health (Oxford, England) 34:138–148. https://doi.org/10.1093/pubmed/fdr054
Caldarelli M, Massimi L, Tamburrini G, Cappa M, Di Rocco C (2005) Long-term results of the surgical treatment of craniopharyngioma: the experience at the Policlinico Gemelli, Catholic University, Rome. Child’s Nerv Syst 21:747–757. https://doi.org/10.1007/s00381-005-1186-5
Clark AJ, Cage TA, Aranda D, Parsa AT, Sun PP, Auguste KI, Gupta N (2013) A systematic review of the results of surgery and radiotherapy on tumor control for pediatric craniopharyngioma. Child’s Nerv Syst 29:231–238. https://doi.org/10.1007/s00381-012-1926-2
Cohen M, Guger S, Hamilton J (2011) Long term sequelae of pediatric craniopharyngioma - literature review and 20 years of experience. Front Endocrinol 2:81. https://doi.org/10.3389/fendo.2011.00081
De Vile CJ, Grant DB, Kendall BE, Neville BG, Stanhope R, Watkins KE, Hayward RD (1996) Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? J Neurosurg 85:73–81. https://doi.org/10.3171/jns.1996.85.1.0073
Elliott RE, Hsieh K, Hochm T, Belitskaya-Levy I, Wisoff J, Wisoff JH (2010) Efficacy and safety of radical resection of primary and recurrent craniopharyngiomas in 86 children. J Neurosurg Pediatr 5:30–48. https://doi.org/10.3171/2009.7.Peds09215
Gonc EN, Yordam N, Ozon A, Alikasifoglu A, Kandemir N (2004) Endocrinological outcome of different treatment options in children with craniopharyngioma: a retrospective analysis of 66 cases. Pediatr Neurosurg 40:112–119. https://doi.org/10.1159/000079852
Harrell FE Jr (2015) Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer, Berlin
Hoffman HJ, De Silva M, Humphreys RP, Drake JM, Smith ML, Blaser SI (1992) Aggressive surgical management of craniopharyngiomas in children. J Neurosurg 76:47–52. https://doi.org/10.3171/jns.1992.76.1.0047
Jung TY, Jung S, Moon KS, Kim IY, Kang SS, Kim JH (2010) Endocrinological outcomes of pediatric craniopharyngiomas with anatomical pituitary stalk preservation: preliminary study. Pediatr Neurosurg 46:205–212. https://doi.org/10.1159/000318426
Karavitaki N, Brufani C, Warner JT, Adams CB, Richards P, Ansorge O, Shine B, Turner HE, Wass JA (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol 62:397–409. https://doi.org/10.1111/j.1365-2265.2005.02231.x
Lafferty AR, Chrousos GP (1999) Pituitary tumors in children and adolescents. J Clin Endocrinol Metab 84:4317–4323. https://doi.org/10.1210/jcem.84.12.6215
Merchant TE, Kiehna EN, Sanford RA, Mulhern RK, Thompson SJ, Wilson MW, Lustig RH, Kun LE (2002) Craniopharyngioma: the St. Jude Children’s Research Hospital experience 1984-2001. Int J Radiat Oncol Biol Phys 53:533–542
Muller HL (2010) Childhood craniopharyngioma--current concepts in diagnosis, therapy and follow-up. Nat Rev Endocrinol 6:609–618. https://doi.org/10.1038/nrendo.2010.168
Muller HL, Emser A, Faldum A, Bruhnken G, Etavard-Gorris N, Gebhardt U, Oeverink R, Kolb R, Sorensen N (2004) Longitudinal study on growth and body mass index before and after diagnosis of childhood craniopharyngioma. J Clin Endocrinol Metab 89:3298–3305. https://doi.org/10.1210/jc.2003-031751
Muller HL, Bruhnken G, Emser A, Faldum A, Etavard-Gorris N, Gebhardt U, Kolb R, Sorensen N (2005) Longitudinal study on quality of life in 102 survivors of childhood craniopharyngioma. Child’s Nerv Syst 21:975–980. https://doi.org/10.1007/s00381-004-1124-y
Paja M, Lucas T, Garcia-Uria J, Salame F, Barcelo B, Estrada J (1995) Hypothalamic-pituitary dysfunction in patients with craniopharyngioma. Clin Endocrinol 42:467–473
Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46:220–229
Prabhu VC, Brown HG (2005) The pathogenesis of craniopharyngiomas. Child’s Nerv Syst 21:622–627. https://doi.org/10.1007/s00381-005-1190-9
Steno J, Bizik I, Steno A, Matejcik V (2011) Craniopharyngiomas in children: how radical should the surgeon be? Child’s Nerv Syst 27:41–54. https://doi.org/10.1007/s00381-010-1330-8
Sughrue ME, Yang I, Kane AJ, Fang S, Clark AJ, Aranda D, Barani IJ, Parsa AT (2011) Endocrinologic, neurologic, and visual morbidity after treatment for craniopharyngioma. J Neuro-Oncol 101:463–476. https://doi.org/10.1007/s11060-010-0265-y
Titsworth WL, Scott RM, Smith ER (2016) National analysis of 2454 pediatric moyamoya admissions and the effect of hospital volume on outcomes. Stroke 47:1303–1311. https://doi.org/10.1161/strokeaha.115.012168
Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE (2011) Regression methods in biostatistics: linear, logistic, survival, and repeated measures models. Springer Science & Business Media,
Zada G, Laws ER (2010) Surgical management of craniopharyngiomas in the pediatric population. Hormone Res Paedia 74:62–66. https://doi.org/10.1159/000309349
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fouda, M.A., Riordan, C.P., Zurakowski, D. et al. Analysis of 2141 pediatric craniopharyngioma admissions in the USA utilizing the Kids’ Inpatient Database (KID): predictors of discharge disposition. Childs Nerv Syst 36, 3007–3012 (2020). https://doi.org/10.1007/s00381-020-04640-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04640-4