Abstract
Acute kidney injury (AKI) is a common complication after Percutaneous Coronary Intervention (PCI) for ST segment elevation myocardial infarction (STEMI) and is associated with poor outcomes. AKI is diagnosed by the dynamic change of serum Cr, but it could not predict AKI. This study aimed to evaluate a biomarker array that may fulfill this shortage. Setting: Cardiology Department, Tanta University Hospital. Design: Prospective interventional study included 280 acute STEMI patients who underwent emergency PCI. Serial samples of blood and urine were obtained at the time of admission to the hospital (T0) and PCI unit (T1) and at 12 h and 72 h (T12 and T72) after coronary revascularization to estimate levels of serum Cr, creatine phosphokinase, and heart-type fatty acid-binding protein (H-FABP) and calculation of neutrophil/lymphocyte ratio (NLR) and urinary liver-type FABP (L-FABP). AKI was diagnosed according to the recommendations of the European Renal Best Practice as the times of increased serum Cr concerning baseline level. 85 patients developed AKI. Regression analyses defined a high NLR ratio in the T0 sample as the most significant predictor for early AKI diagnosed at T1 time, while high NLR and serum H-FABP levels in T1 samples as the significant predictors for AKI defined at T12 time. However, high urinary L-FABP levels in T12 samples and high NLR are significant predictors for AKI at T72 time. Combined estimations of serum H-FABP and urinary L-FABP with the calculation of NLR could predict the oncoming AKI and discriminate its pathogenesis. The study protocol was approved by the Local Ethical Committee at Tanta Faculty of Medicine by approval number: 35327/3/22. For blindness purposes, the authors will be blinded about the laboratory results till the end of 72 h after revascularization and the clinical pathologist will be blinded about the indication for the requested investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is marked by deterioration of renal function within hours or days and is manifested by minor rises in serum creatinine (Cr) up to anuric renal failure needing renal replacement therapy (RRT) [1].
There are multiple risk factors for AKI development in patients who had acute coronary syndrome (ACS) especially the presence of chronic kidney disease, diabetes mellitus, old age, anemia, and dehydration [2]. Moreover, systemic hypoperfusion in patients with acute myocardial infarction (AMI) causes renal ischemia secondary to the acute left ventricular systolic failure leading to the development of AKI [3].
Contrast-induced AKI (CI-AKI) was defined as an increased serum Cr level by ≥ 0.5 mg/dl, or ≥ 25%, over the baseline level within 72 h after a contrast material (CM) administration [4]. CI-AKI is mostly the third most common cause of hospital-acquired AKI [5] and ACS patients have a threefold higher risk of developing CI-AKI [6]. Unfortunately, CI-AKI is associated with poor outcomes with prolonged hospitalization and increased morbidity and mortality rates [7].
Heart-type fatty acid-binding protein (H-FABP) is a low molecular weight cytosolic protein, which is primarily expressed in myocardial tissue and functions as the principal transporter of long-chain fatty acids in the cardiomyocyte [8]. Under normal conditions, H-FABP is not present in plasma or interstitial fluid, but is released into the blood upon cardiac cellular injury within 2 h, peaks at about 4–6 h, and returns to its baseline level in 20 h [9], so could be used as an early marker of AMI due to its high sensitivity, specificity and prognostic value [10]. Liver-type fatty acid-binding protein (L-FABP) is a 14kDa protein, which is expressed in the proximal tubular epithelial cells as a carrier of short-chain fatty acid to be transported to and β-oxidized at the mitochondria or peroxisomes [11]. L-FABP is more closely associated with tubular than glomerular dysfunction and is detected in urine only during tubular injury [12].
Objective
The ability of estimated biomarkers' levels during 72 h after admission of AMI patients to the Emergency Department to predict AKI development and to discriminate its underlying etiology was investigated.
Setting
Cardiology Department, Faculty of Medicine, Tanta University.
Design
Prospective comparative interventional study.
Patients
All patients who arrived at the emergency department from March 2021 till January 2022 with manifestations suggestive of AMI were clinically evaluated for demographic data, smoking, history of previous attacks, maintenance on fibrinolytic drugs, and associated medical conditions, or cardiovascular surgeries. Then, patients underwent complete cardiac examination including ECG to evaluate presence or absence of ST segment elevation and echocardiography to evaluate the ventricular functions.
Diagnostic definitions
-
1.
STEMI was diagnosed according to the 2017 ESC Guidelines for the management of AMI in patients presenting with typical angina pectoris-like manifestation with elevated serum creatine kinase and cardiac Troponin I. ST segment elevation was defined as at least 0.2 mV elevations in ≥ 2 contiguous precordial leads or at least 0.1 mV elevations in the limbs lead [13].
-
2.
CKD was defined according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) serum Cr-based equation for estimating glomerular filtration rate (GFR) as at-admission eGFR of ≤ 60 ml/min/1.73 m2 [14].
-
3.
AKI was diagnosed according to the recommendations of the European Renal Best Practice [15] for diagnosis and severity staging of AKI as Stage I if there was an increased serum Cr level by 1.5–1.9 times the baseline level or if it was increased by > 0.3 mg/dl or if urine output (UOP) was < 0.5 ml/kg/h for a 6-h block; Stage II if serum Cr level was increased by 2–2.9 times the baseline level or if UOP was < 0.5 ml/kg/h for two successive 6-h blocks; and Stage III if there was increased serum Cr level by > 3 times the baseline level or if UOP was < 0.3 ml/kg/h during > 24 h, anuria for > 12 h or if RRT was initiated.
-
4.
The probable patients' prognosis was predicted according to Killip's classification with no clinical signs of heart failure indicating class I, presence of rales or cracks in lung and S3 gallop, and elevated jugular venous pressure defining class II patients, presence of manifestation of acute pulmonary edema indicates class III, while manifestations of cardiogenic shock with blood pressure < 90mmHg and evidence of low cardiac output indicates class IV [16].
Exclusion criteria
The exclusion criteria included medical reperfusion using fibrinolytic drugs, provisional diagnosis of non-ST segment elevation myocardial infarction (NSTEMI), diabetic nephropathy, or maintenance on RRT. Patients who also had history of receiving nephrotoxic, immunosuppressing, and chemotherapeutic drugs were also excluded. Patients of Killip's classes II–IV who had circulatory impairment were considered as high-risk patients, and patients who refused to undergo percutaneous coronary intervention (PCI) were excluded and transferred to department for receiving the appropriate treatment. During the procedure, patients who developed cardiogenic shock or required mechanical ventilation were also excluded from statistical analyses.
Inclusion criteria
Patients with a provisional diagnosis of ST segment elevation myocardial infarction (STEMI) who did not receive medical fibrinolysis, accepted to undergo emergency PCI, and free from exclusion criteria were enrolled in the study.
Laboratory workup
Sample collection and processing
At the time of admission to ED, urine and blood samples were obtained and prepared to undertake the assigned investigations:
-
1.
Urine samples: Random midstream urine sample was collected in a sterile tube and immediately centrifuged at 3000 rpm for 20 min. The supernatants were carefully separated into two parts:
-
(a)
The first part: 1 ml of supernatant was collected in 1.5 ml sterile dry tubes and preserved at − 20 °C till be ELISA assayed for urinary L-FABP levels.
-
(b)
The second part: 3 ml of supernatant was collected in a clean dry tube for measurement of urinary Cr.
-
(a)
-
2.
Blood samples (5 ml) were obtained under complete aseptic conditions from the antecubital vein; two blood samples were obtained:
-
The 1st blood sample was divided into two parts, one was collected in a sodium fluoride (2 mg sodium fluoride/ml blood) containing tube to prevent glycolysis for estimation of blood glucose levels and the other part was collected in tri-potassium ethylenediaminetetraacetate (K3-EDTA) containing tube for complete blood count including a differential leukocytic count for calculation of neutrophil/lymphocyte ratio (NLR).
-
The 2nd blood sample was collected in a plain tube and blood was allowed to clot in a warm water bath at a temp of 37 °C for 5 min and then centrifuged at 5000 rpm for 2 min to separate serum. The resultant serum sample was divided into two parts: one was used for estimation of serum Cr and creatine phosphokinase (CPK) and the 2nd part was collected in a clean Eppendorf tube and stored at − 20 °C for ELISA estimation of human H-FABP
-
Investigation
-
1.
Blood glucose level using glucose oxidase method [17].
-
2.
Serum creatine phosphokinase uses a method, which is based on the reaction of creatine, formed enzymatically from creatine phosphate and ADP, with p-nitrophenylglyoxal under alkaline conditions to produce a colored product that absorbs maximally at 480 nm [18].
-
3.
Serum creatinine using the Jaffe-based creatinine–picrate formation in an alkaline medium. [19, 20]
-
4.
Serum human H-FABP was measured with the enzyme-linked immunoassay (ELISA) kit (catalog no. ab243682 Abcam Inc., San Francisco, USA) by quantitative sandwich enzyme immunoassay technique [21].
-
5.
Urinary creatinine (uCr) was measured with a creatinine (urinary) colorimetric assay kit (catalog no. 500701, Cayman Chemical, Ann Arbar, MI, USA) by Jaffe’s reaction method [22].
-
6.
Urinary L-FABP was measured with the enzyme-linked immunoassay (ELISA) kit (catalog no. ab2218261 Abcam Inc., San Francisco, USA) by quantitative sandwich enzyme immunoassay technique. The total urinary L-FABP levels were normalized to the estimated Cr concentration to determine urinary L-FABP/Cr (µg/gCr) ratios [11].
Management protocol
-
According to the 2017 ESC Guidelines for the management of AMI in patients presenting with ST segment elevation, the time of diagnosis of STEMI during ECG examination was considered as the zero time if the patient had arrived directly to the PCI unit within < 10 min after pain sensation and PCI was undertaken after diagnosis. The maximum allowable time for primary PCI intervention is ≤ 120 min.
-
Serial estimation of serum Cr levels for diagnosis of AKI according to the ERBP recommendations [15], with an estimation of serum CPK and calculation of N/L ratio. Multiple blood samples were obtained at the time of admission to the emergency department to obtain baseline data (T0 sample), at the time of admission to the PCI unit, and before CM injection for evaluation of the effect of ischemia secondary to AMI on kidney functions (T1 sample), at 12 h after revascularization (T12 sample) for evaluation of the effects of revascularization and immediate effects of CM on kidney functions and 72 h (T72 sample) after CM injection for diagnosis of CI-AKI.
Study outcomes
-
1.
The primary outcome is the ability of estimated serum and urinary biomarkers levels and NLR to discriminate STEMI patients liable to develop AKI.
-
2.
The secondary outcomes include:
-
•
The ability of the estimated biomarkers' levels to differentiate between patients who developed STEMI-induced AKI and those who developed CI-AKI.
-
•
The determination of the predictability of using more than one marker to achieve outcomes.
Sample size
The sample size was calculated by the G*Power (Version 3.1.9.2) [23]. A previous study of the relation between the L-FABP level and the development of AKI during AMI attack reported that the median level of L-FABP in No-AKI patients was 1 (range 0.5–2.8 ng/ml), while in AKI patients, the median value was 2.1; range 0.67–6.3 ng/mL [24]. Considering the null hypothesis was the absence of difference in the L-FABP level between AKI and No-AKI groups and considering the previously documented AKI incidence rate during interventional cardiology which was 29.5% [24] and 36% [25], so to achieve a similar incidence of AKI, using α error 5% and a power of 80%, and considering the required sample size for AKI group must be 85 patients, the total patients' number must be 250 to get an AKI incidence of 34%.
Results
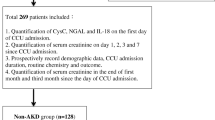
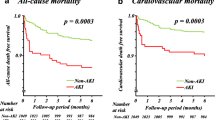
During the study duration, 359 patients were eligible for evaluation, 79 patients were excluded for not fulfilling the inclusion criteria, and 280 patients were enrolled in the study. Serum Cr levels estimated at the time of hospital admission (T0 Sample) showed non-significant differences between patients. However, serum Cr levels were significantly higher in T1, T12, and T72 samples compared to levels estimated in T0 samples. Estimated serum Cr levels in samples obtained at T1, T12, and T72 times were increased in samples of 13, 35, and 37 patients, respectively, up to the AKI diagnostic levels, and these 85 patients were grouped as AKI group. In the same samples of the remaining 195 patients, the times of increase in serum Cr were not diagnostic for AKI (No-AKI group) and significantly lower in comparison to that of AKI patients (Table 1, Fig. 1). According to times of increase in serum Cr levels concerning T0 levels, there were 40 patients of AKI grade I, 41 patients of AKI grade II, and 4 patients of AKI grade III (Table 1). Revision of enrollment data of studied patients after grouping showed non-significant differences between T0 data of patients of both groups as shown in Table 2.
Serum CPK levels were increased in T1 samples significantly more than in T0 samples but decreased in T12 samples significantly compared to levels estimated in T0 and T1 samples. Serum levels of CPK were non-significantly higher in T0 and T12 samples but significantly higher in T1 samples of AKI than in No-AKI patients.
Serum levels of H-FABP showed a progressive increase in T1 and T12 samples with a significant difference between levels estimated in T0 samples and between levels estimated in T1 and T12 samples. However, the difference between AKI and No-AKI patients was non-significant in T0 samples but was significant in T1 and T12 samples.
The calculated NLR was significantly higher in patients of the AKI group compared to those of the No-AKI group in all samples and significantly higher in each sample in comparison to the preceding samples of AKI patients. On contrary, in samples of No-AKI patients, the ratio was significantly higher in T1 and T12 samples than in T0 and T72 samples with a non-significantly higher ratio in T1 than in T12 samples.
Estimated urinary levels of L-FABP in T1 samples showed a non-significant difference in comparison to levels estimated in T0 samples of patients in both groups. In T1 samples, urinary L-FABP levels were significantly higher in samples of AKI than in No-AKI patients. Urinary L-FABP levels estimated in T12 samples were significantly higher compared to levels estimated in the preceding samples with significantly higher levels in samples of AKI than in No-AKI patients. At 72 h after revascularization, urinary L-FABP levels were higher in samples of AKI patients but decreased in samples of No-AKI patients in comparison to levels estimated at T1 and T12 and with significantly higher levels in AKI than No-AKI samples (Table 3).
According to the results of linear univariate and multivariate regression analyses, a high NLR ratio in the T0 sample was defined as the most significant predictor for the times of increase in serum Cr in T1 samples and high NLR and serum H-FABP levels in T1 samples as the significant predictors for the times of increase in serum Cr levels in T12 samples. On the other hand, high L-FABP levels in T12 urinary samples and high NLR in blood samples are significant predictors for the times of increase in serum Cr in T72 samples (Table 4).
Discussion
Estimated serum Cr levels in T0 samples were within the normal range but were increased in all patients up to the diagnostic level for AKI in 13, 35, and 37 patients in T1, T12, and T72 samples. AKI cases that were detected at the time of admission to PCI (T1 time) could be attributed to the effect of ischemia secondary to the coronary obstruction that resulted in AMI. In line with this attribution, recent experimental studies detected reduced renal blood flow by about 40% with cardiac ischemia [27].
The development of AKI at 12 h after revascularization (T12 time) may be secondary to the effect of the washed inflammatory cytokines and free radicals in association with cardiac and renal ischemia–reperfusion injury as previously detected in animal models of ischemia–reperfusion AKI [28, 29] or may be due to early-onset contrast-induced AKI (CI-AKI) that was previously detected using an animal model of CI-AKI where microscopic examination assured that the strongest renal damage in CI-AKI existed between 12 and 24 h after CM injection [28]. On the contrary, AKI cases detected at 72 h after revascularization (T72 time) are considered CI-AKI as previously documented [4]. The reported AKI rate was in line with or lower than that reported by previous studies [30,31,32] evaluated similar condition and detected AKI incidence ranging between 29.6 and 46%.
Statistical analyses defined serum levels of H-FABP in T0 and T1 samples as a significant predictor, while serum levels of CPK despite being elevated in T0 and T1 samples were less significant predictors for increases in serum Cr at T1 and T12 respectively, and could predict increased serum Cr levels at T1 only. These data assured the relation between cardiac ischemia and development of AKI and supported the previous works that reported high sensitivity and specificity of high serum H-FABP to predict AKI [33] and worsening of renal function [34] in the setting of acute heart failure, especially in non-chronic kidney disease patients. A recent study documented that serum level of H-FABP was found to be changed significantly after PCI and can predict AKI with high sensitivity and negative predictive value [35].
The low levels of L-FABP in T0 and T1 urine samples manifest the low-grade early kidney affection as previously documented that kidneys try to preserve L-FABP, which is fatty acid transporter for renal mitochondria [11], but its progressive increase in the subsequent samples indicated renal tubular injury. The detected increase in urinary L-FABP in T1 than in T0 samples indicated the effect of prerenal ischemia secondary to AMI, which induces up-regulation of the expression levels of L-FABP to bind the ischemia-induced lipid peroxidation products and transferring them to urinary spaces [36] and this might explain the reported significant difference in urinary L-FABP levels in T1 samples of AKI and No-AKI patients.
Statistical analyses defined high urinary L-FABP in the T12 sample as a predictor and the T72 sample as a significant discriminator for AKI cases. The obtained data are in hand with the previously reported significant differences between levels of urinary L-FABP estimated at 24 and 48-h after dye injection before cardiac surgery [37] and with the conclusion that estimation of urinary L-FABP levels improves early prediction of AKI in patients hospitalized at medical cardiac intensive care units [38] and after coronary angiography/PCI [39]. Also, these results are in line with the survey study that found cardiologists who introduced pre- and peri-cardiac interventions estimation of L-FABP into patient care were 2.9 times more likely to correctly identify their patients' risk for AKI and were more than twice as likely to treat AKI [40].
The estimated high NLR in T0 and T1 samples indicated its relation with cardiac ischemia and supported the previous data that the NLR is an independent risk factor and a predictor of coronary artery disease (CAD) [41, 42]. Moreover, statistical analyses of NLR in T0 and T1 samples showed the significant predictability of high NLR in early samples for oncoming AKI. These findings assured the reported high predictability of a high systemic immune inflammation index, which equals the NLR multiplied by platelet count, to define patients liable to develop AKI after PCI [43, 44].
Further, high NLR in the T12 sample was defined as a significant predictor for the development of CI-AKI at 72 h after injection. These findings indicated two important points: first, early estimation of NLR could predict early AKI after dye injection and this suggestion went in hand with a previous study, which found high NLR was an independent predictor of CI-AKI in AMI patients and recommended its use to improve on current risk prediction models [4]. Second, the reported progressively increasing NLR up to 72 h after intervention pointed to the inflammatory origin of CI-AKI and assured the results obtained using AKI animal models that inhibition of NLRP3 inflammasome attenuated renal apoptosis and upregulated HIF1A and BNIP3-mediated mitophagy in CI-AKI [45] and the study which detected renal neutrophil and macrophage chemotaxis, accumulation of the lymphocyte antigen 6 complex with pyroptosis, mitophagy, and apoptosis in renal tissues of CI-AKI animal model [28].
Thus, elevated serum levels of H-FABP and high NLR before PCI could predict the development of AKI secondary to myocardial ischemia, while high NLR and urinary L-FABP 12 h after PCI could predict CI-AKI, and high urinary L-FABP levels and NLR 72 h after PCI could define AKI patients.
Conclusion
The obtained results spotlight the ability of the combined estimations of serum heart-type and urinary liver-type FABP with the calculation of NLR to predict the oncoming AKI and discriminate its underlying pathogenesis.
Recommendations
The same combination of the studied laboratory variables could be used to evaluate maneuvers to be used to minimize the deleterious effect of CM as pre-procedural hydration and metformin and for evaluating the effect of varied types of dyes.
Availability of data and materials
Available on request.
References
Kumar H, Jilanee D, Mehta SM, Gul A, Shah SMH, Saleem S, Sarfraz MB, Ashraf SU, Wali S (2022) Frequency and predictors of acute kidney injury in patients with acute coronary syndrome in a tertiary care hospital: a retrospective study. Cureus 14(2):e21869
Schmucker J, Fach A, Becker M, Seide S, Bünger S, Zabrocki R, Fiehn E, Würmann-Busch B, Pohlabeln H, Günther K, Ahrens W, Hambrecht R, Wienbergen H (2018) Predictors of acute kidney injury in patients admitted with ST-elevation myocardial infarction-results from the Bremen STEMI-Registry. Eur Heart J Acute Cardiovasc Care 7:710–722
Cosentino N, Resta M, Somaschini A, Campodonico J, Lucci C, Moltrasio M, Bonomi A, Cornara S, Camporotondo R, Demarchi A, De Ferrari G, Bartorelli A, Marenzi G (2021) Acute kidney injury and in-hospital mortality in patients with ST-elevation myocardial infarction of different age groups. Int J Cardiol 344:8–12
Butt K, D’Souza J, Yuan C, Jayakumaran J, Nguyen M, Butt H, Abusaada K (2020) Correlation of the neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) with contrast-induced nephropathy in patients with acute coronary syndrome undergoing percutaneous coronary interventions. Cureus 12(12):e11879
Abdalla M, Ahmed K, Yousef B (2022) Incidence and risk factors of contrast-induced acute kidney injury in sudanese patients undergoing coronary angiography: a descriptive prospective study. Cureus 14(2):e21876
Uzunhasan I, Yildiz A, Arslan S, Abaci O, Kocas C, Kocas B, Cetinkal G, Dalgic Y, Karaca O, Dogan S (2017) Contrast-induced acute kidney injury is associated with long-term adverse events in patients with acute coronary syndrome. Angiology 68(7):621–626
Natha J, Javaheri P, Kruger D, Benterud E, Pearson W, Tan Z, Ma B, Tyrrell B, Har B, Graham M, James M (2020) Patient experience after risk stratification and follow-up for acute kidney injury after cardiac catheterization: patient survey. CJC Open 3(3):337–344
Vera M, Koch C, Kavsak P, El-Khoury J (2021) Determination of 97.5th and 99th percentile upper reference limits for heart-type fatty acid-binding protein (H-FABP) in a US population. Clin Chim Acta 523:397–401
Al-Hadi H, William B, Fox K (2009) Serum level of heart-type fatty acid-binding protein in patients with chronic renal failure. Sultan Qaboos Univ Med J 9(3):311–314
Moon MG, Yoon CH, Lee K, Kang SH, Youn TJ, Chae IH (2021) Evaluation of heart-type fatty acid-binding protein in early diagnosis of acute myocardial infarction. J Korean Med Sci 36(8):e61
Kamijo-Ikemori A, Ichikawa D, Matsui K, Yokoyama T, Sugaya T, Kimura K (2013) Urinary L-type fatty acid-binding protein (L-FABP) as a new urinary biomarker promulgated by the Ministry of Health, Labour and Welfare in Japan. Rinsho Byori 61(7):635–640
Sunayama T, Yatsu S, Matsue Y, Dotare T, Maeda D, Ishiwata S, Nakamura Y, Suda S, Kato T, Hiki M, Kasai T, Minamino T (2022) Urinary liver-type fatty acid-binding protein as a prognostic marker in patients with acute heart failure. ESC Heart Fail 9(1):442–449
Ibanez B, James S, Agewall S, Antunes M, Bucciarelli-Ducci C, Bueno H, Caforio A, Crea F, Goudevenos J, Halvorsen S, Hindricks G, Kastrati A, Lenzen M, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P, ESC Scientific Document Group (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39(2):119–177
Levey A, Stevens L, Schmid C, Zhang Y, Castro A, Feldman H, Kusek J, Eggers P, Van Lente F, Greene T, Coresh J (2009) CKD-EPI (Chronic kidney disease epidemiology collaboration): a new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Ad-Hoc Working Group of ERBP, Fliser D, Laville M, Covic A, Fouque D, Vanholder R, Juillard L, Van Biesen W (2012) A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management, and contrast-induced nephropathy. Nephrol Dial Transplant 27(12):4263–4272
Khot U, Jia G, Moliterno D, Lincoff M, Khot M, Harrington R, Topol E (2003) Prognostic importance of physical examination for heart failure in non-ST-elevation acute coronary syndromes the enduring value of killip classification. JAMA 290(16):2174–2181
Tinder P (1969) Determination of blood glucose. Ann Clin Biochem 6:24
Aminlari M, Vaseghi T (1987) A new colorimetric method for determination of creatine phosphokinase. Anal Biochem 164(2):397–404
Jaffe M (1886) Ueber den Niederschlag, welchen Pikrinsäure in normalem Harn erzeugt und über eine neue Reaction des Kreatinins. ZPhysiolChem 10:391–400
Peake M, Whiting M (2006) Measurement of serum creatinine–current status and future goals. Clin Biochem Rev 27:173–184
Liu Y, Tian M, Jiang X, Luo J, Yi Z (2014) Evaluation of a heart-type fatty acid-binding protein detection kit for diagnosis of the acute coronary syndrome. Nan Fang Yi Ke Da Xue Xue Bao 34(6):901–903
Taussky HH (1961) Creatinine and creatine in urine and serum. In: Seligson D (ed) Standard methods of clinical chemistry, vol 3. Academic Press, New York, pp 99–113
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Prowle J, Calzavacca P, Licari E, Ligabo V, Echeverri J, Bagshaw S, Haase-Fielitz A, Haase M, Ostland V, Noiri E, Westerman M, Devarajan P, Bellomo R (2015) Combination of biomarkers for diagnosis of acute kidney injury after cardiopulmonary bypass. Ren Fail 37(3):408–416
Deftereos S, Giannopoulos G, Tzalamouras V, Raisakis K, Kossyvakis C, Kaoukis A, Panagopoulou V, Karageorgiou S, Avramides D, Toutouzas K, Hahalis G, Pyrgakis V, Manolis A, Alexopoulos D, Stefanadis C, Cleman M (2013) Renoprotective effect of remote ischemic post-conditioning by intermittent balloon inflations in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 61:1949–1955
Yamanaka T, Kawai Y, Miyoshi T, Mima T, Takagaki K, Tsukuda S, Kazatani Y, Nakamura K, Ito H (2015) Remote ischemic preconditioning reduces contrast-induced acute kidney injury in patients with ST elevation myocardial infarction: a randomized controlled trial. Int J Cardiol 178:136–141
Tai H, Jiang X, Lan Z, Li Y, Kong L, Yao S, Song N, Lv M, Wu J, Yang P, Xiao X, Yang G, Kuang J, Jia L (2021) Tanshinone IIA combined with CsA inhibit myocardial cell apoptosis induced by renal ischemia–reperfusion injury in obese rats. BMC Complement Med Ther 21:100
Li Y, Shi D, Zhang H, Yao X, Ren K (2022) Magnetic resonance imaging of contrast-induced acute renal injury and related pathological alterations in vivo. Anal Cell Pathol (Amst) 2022:6984200
Horikawa T, Maehata J, Hashimoto F, Ikuhara T, Araki H, Umeno H, Sano Y, Ishikawa C, Takagi H, Watanabe A, Koizumi T (2022) Constructing a continuous hemodiafiltration-type circulatory model of acute kidney injury in pigs. Ther Apher Dial 26:507–514
Shacham Y, Gal-Oz A, Flint N, Keren G, Arbel Y (2016) Serum uric acid levels and renal impairment among ST-segment elevation myocardial infarction patients undergoing primary percutaneous intervention. Cardiorenal Med 6:191–197
Taduru SS, Ramakrishnan M, Mustafa RA, Baweja PS (2017) Comparison of the frequency of acute kidney injury in patients with renal transplant who underwent percutaneous coronary intervention versus coronary artery bypass graft surgery. Am J Cardiol 120:1104–1109
Mezhonov EM, Vyalkina YA, Vakulchik KA, Halaev SVS (2018) Contrast-induced acute renal injury after percutaneous coronary interventioni in patients with ST-segment elevation myocardial infarction. Kardiologiia 8:5–11
Shirakabe A, Hata N, Kobayashi N, Okazaki H, Shinada T, Tomita K, Yamamoto M, Tsurumi M, Matsushita M, Yamamoto Y, Yokoyama S, Asai K, Shimizu W (2015) Serum heart-type fatty acid-binding protein level can be used to detect acute kidney injury on admission and predict an adverse outcome in patients with acute heart failure. Circ J 79:119–128
Shirakabe A, Hata N, Kobayashi N, Okazaki H, Matsushita M, Shibata Y, Uchiyama S, Sawatani T, Asai K, Shimizu W (2019) Worsening renal failure in patients with acute heart failure: the importance of cardiac biomarkers. ESC Heart Fail 6:416–427
Haybar H, Assareh A, Mohammadzadeh M, Hovyzian S (2020) Relationship between level of heart type fatty acid binding protein (before and after procedures) with acute renal failure after PCI in patients under PCI. Cardiovasc Hematol Disord Drug Targets 20:41–46
Yamamoto T, Noiri E, Ono Y, Doi K, Negishi K, Kamijo A, Kimura K, Fujita T, Kinukawa T, Taniguchi H, Nakamura K, Goto M, Shinozaki N, Ohshima S, Sugaya T (2007) Renal L-type fatty acid-binding protein in acute ischemic injury. J Am Soc Nephrol 18:2894–2902
Hwang Y, Hyun M, Choi B, Chun S, Cho M (2014) Acute kidney injury after using contrast during cardiac catheterization in children with heart disease. J Korean Med Sci 29:1102–1107
Naruse H, Ishii J, Takahashi H, Kitagawa F, Nishimura H, Kawai H, Muramatsu T, Harada M, Yamada A, Motoyama S, Matsui S, Hayashi M, Sarai M, Watanabe E, Izawa H, Ozaki Y (2018) Predicting acute kidney injury using urinary liver-type fatty-acid binding protein and serum N-terminal pro-B-type natriuretic peptide levels in patients treated at medical cardiac intensive care units. Crit Care 22:197
Yoshihara F, Hosoda H, Doi T, Yoshida M, Kitamura K, Yamamoto H, Asaumi Y, Ishibashi-Ueda H, Kishida M, Arisato T, Matsuo M, Miyazato M, Yasuda S (2021) Combined evaluation of plasma B-type natriuretic peptide and urinary liver-type fatty acid-binding protein/creatinine ratio is related to worsening renal function in patients undergoing elective percutaneous coronary intervention. Clin Exp Nephrol 25:1319–1328
Peabody J, Paculdo D, Valdenor C, McCullough P, Noiri E, Sugaya T, Dahlen J (2022) Clinical utility of a biomarker to detect contrast-induced acute kidney injury during percutaneous cardiovascular procedures. Cardiorenal Med 12:11–19
Pan Q, Zhang W, Li X, Chen Z, Yang Y, Wang G (2022) Sex difference in the association between neutrophil to lymphocyte ratio and severity of coronary artery disease. Angiology 73:470–477
Agarwal R, Aurora R, Siswanto B, Muliawan H (2022) The prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease. Coron Artery Dis 33:137–143
Yilmaz Y, Kelesoglu S, Kalay N (2022) A novel predictor of contrast-induced nephropathy in patients with carotid artery disease; the systemic immune inflammation index. Angiology 73:781–787
Öztürk R, İnan D, Güngör B (2022) Systemic immune-inflammation index is a predictor of contrast-induced nephropathy in patients with ST-segment elevation myocardial infarction. Angiology 73:125–131
Lin Q, Li S, Jiang N, Jin H, Shao X, Zhu X, Wu J, Zhang M, Zhang Z, Shen J, Zhou W, Gu L, Lu R, Ni Z (2021) Inhibiting NLRP3 inflammasome attenuates apoptosis in contrast-induced acute kidney injury through the upregulation of HIF1A and BNIP3-mediated mitophagy. Autophagy 17:2975–2990
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Local Ethical Committee at Tanta Faculty of Medicine by Approval No. 35327/3/22. For blindness purposes, the authors will be blinded about the laboratory results till the end of 72 h after revascularization and the clinical pathologist will be blinded about the indication for the requested investigations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alkassas, A., Elbarbary, Y., Sherif, M.H. et al. Biomarker array for prediction of acute kidney injury after percutaneous coronary intervention for patients who had acute ST segment elevation myocardial infarction. Heart Vessels 39, 206–215 (2024). https://doi.org/10.1007/s00380-023-02330-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-023-02330-0