Abstract
For Japanese patients with non-valvular atrial fibrillation (NVAF), the risk of stroke and major bleeding events was assessed by using the CHADS2, CHA2DS2-VASc, and HAS-BLED scores. The risk factors for embolism and major bleeding under DOAC may be different from current reports. We analyzed the data set of the EXPAND Study to determine the risk factors for events among Japanese NVAF patients in the era of direct oral anticoagulant. Using the data of EXPAND Study, the validity for predictability of the CHADS2, CHA2DS2-VASc, and HAS-BLED scores was identified using the receiver operating characteristic curve analysis. Multivariate analysis was performed with the Cox proportional hazard model to determine the independent risk factors for stroke/systemic embolism and major bleeding among NVAF patients receiving rivaroxaban. Explanatory variables were selected based on the univariate analysis. A total of 7141 patients (mean age 71.6 ± 9.4 years, women 32.3%, and rivaroxaban 15 mg per day 56.5%) were included. Incidence rates of stroke/systemic embolism and major bleeding were 1.0%/year and 1.2%/year, respectively. The multivariate analysis revealed that only history of stroke was associated with stroke/systemic embolism (hazard ratio 3.4, 95% confidence interval 2.5-4.7, p < 0.0001). By contrast, age (1.7, 1.1–2.6, p = 0.0263), creatinine clearance (CrCl) 30–49 mL/min (1.6, 1.2-2.2, p = 0.0011), liver dysfunction (1.7, 1.1–2.8, p = 0.0320), history/disposition of bleeding (1.8, 1.0–3.0, p = 0.0348), and concomitant use of antiplatelet agents (1.6, 1.2–2.3, p = 0.0030) were associated with major bleeding. This sub-analysis showed that some components of the HAS-BLED score were independently associated with major bleeding in Japanese NVAF patients receiving anticoagulation therapy by rivaroxaban. Additionally, CrCl value of 30–49 mL/min was an independent predictor of major bleeding in patients receiving rivaroxaban.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-valvular atrial fibrillation (NVAF) is a common disease in the cardiovascular field, but is also a type of arrhythmia often observed in other medical fields. It can occur without any clear underlying diseases, with the prevalence increasing with aging. The overall prevalence of NVAF in Japan is 0.56%, estimated using the data from periodical medical checkups of patients aged ≥ 40 years [1, 2]. Of the patients, 85% were older than 60 years and 25% were older than ≥ 80 years, leading to an overall estimated prevalence of 1.09% in 2050 [1, 2].
For evaluation of thromboembolic risks in patients with NVAF, CHADS2 (congestive heart failure [CHF], hypertension [HT], age ≥ 75 years, diabetes mellitus [DM], previous stroke/transient ischemic attack [TIA]) score has been used and validated as optimal in Japanese patients [3,4,5]. Among Japanese NVAF patients without anticoagulation, the incidence rate of ischemic stroke has been reported to be 13.3 per 1000 person-years by the pooled analysis of data from J-RHYTHM Registry, Fushimi AF Registry, and Shinken Database [4]. CHA2DS2-VASc (CHF, HT, age ≥ 75 years, DM, previous stroke/TIA, vascular disease, age 65–74 years, female; age ≥ 75 years and previous stroke carry doubled risk weight) score was introduced in Europe to extract truly low-risk patients from patients with CHADS2 score of 0 and 1 [6, 7]. In the above-mentioned pooled analysis in Japanese patients without anticoagulants, an increase in incidence of ischemic stroke was observed in Japanese patients with CHA2DS2-VASc scores ≥ 2 [4]. Furthermore, although other Japanese data validated the usefulness of CHA2DS2-VASc score, its full applicability remains uncertain in the era of direct oral anticoagulants (DOACs) [8,9,10,11]. Risk stratification schemes used to predict bleeding events during treatment with anticoagulants include HAS-BLED, ORBIT, and ATRIA; however, HAS-BLED score has been used together with CHA2DS2-VASc score in the guidelines of the European Society of Cardiology [7, 12, 13]. The usefulness of HAS-BLED score was also validated in Japanese patients [10, 14].
The EXPAND Study is a prospective observational cohort study in patients with NVAF who were treated with Japan-specific dosages of rivaroxaban to determine the efficacy and safety in the real-world clinical setting [15, 16]. The risk factors for embolism and major bleeding under DOAC may be different from current reports. In this sub-analysis, we determined the relationship of each component of CHADS2, CHA2DS2-VASc, and HAS-BLED scores with thromboembolic and bleeding events among Japanese NVAF patients receiving Japan-specific dosage of rivaroxaban, and validated the predictability of those scores.
Methods
Study design and outcome
The EXPAND Study (Evaluation of the effectiveness and safety of Xa inhibitor for the Prevention of stroke And systemic embolism [SE] in a Nationwide cohort of Japanese patients Diagnosed as NVAF) is an investigator-initiated multicenter registry conducted from November 2012 to March 2016 to evaluate the efficacy and safety of rivaroxaban for prevention of stroke/SE in Japanese NVAF patients in the real-world clinical practice as reported elsewhere [15, 16]. Briefly, 7141 patients with NVAF aged ≥ 20 years were included from 684 medical institutes (mean age 71.6 ± 9.4 years, women 32.3%). They were followed for a mean duration of 2.5 years. The endpoints were stroke/SE and major bleeding events (defined as International Society on Thrombosis and Haemostasis [ISTH] major bleeding criteria) [15, 16]. The incidence rates for stroke/SE and ISTH major bleeding were 1.0%/year (176 events) and 1.2%/year (215 events), respectively [16].
The present study was conducted in accordance with the Declaration of Helsinki; the Ethical Guidelines for Clinical Studies by the Japanese Ministry of Health, Labour and Welfare; and all applicable laws and regulations in Japan. The protocol was reviewed and approved by the institutional review boards and/or ethics committees in all the participating institutes. All patients provided written informed consent before enrollment in this study. This study is registered with ClinicalTrials.gov (NCT02147444) and the University Hospital Medical Information Network clinical trials registry (UMIN000009376).
Statistical analysis
The incidence rates of outcome events (%/year) from time of starting rivaroxaban to the initial onset of events were compared according to patient characteristics and medical history. The validity for prediction ability of the CHADS2, CHA2DS2-VASc and HAS-BLED scores was identified using the receiver operating characteristic (ROC) curve analysis. Hazard ratio (HR), 95% confidence interval (CI), and p value for thromboembolic and bleeding events were estimated using Cox proportional hazards model. Multivariate analysis was conducted below model. Components of CHADS2 and CHA2DS2-VASc scores were selected for thromboembolic events, whereas components of HAS-BLED score were selected for major bleeding. Labile prothrombin time international normalized ratio was handled as “data not available” for HAS-BLED score. The factors selected showing a significant difference (p < 0.05) in the univariate analysis. P values of < 0.05 were considered to be statistically significant. All statistical analyses were conducted using the SAS software (SAS for Windows Release ver. 9.2 or later, SAS Institute Inc.).
Results
Patient characteristics
Baseline characteristics of the patients are listed in Table 1. Among 7141 patients enrolled, approximately 80% aged ≥ 65 years, 40% aged ≥ 75 years, and 70% had HT. Twenty percent of patients had prior history of ischemic stroke. A total of 972 patients (13.6%) were at lower risk for thromboembolism, with CHA2DS2-VASc scores of 0 and 1. Among patients complicated with HT and DM, 4675 patients (94.5%) and 1118 patients (91.3%) received antihypertensive and antidiabetic medications at baseline of this study, respectively.
Outcome of sub-group analysis
The results of validity for predictability of the scores are shown in Fig. 1. The area under the ROC curve and score of cut-off in CHADS2, CHA2DS2-VASc, and HAS-BLED were 0.6553 (95% CI 0.6161–0.6945) and 3, 0.6470 (95% CI 0.6075–0.6865) and 4, and 0.5925 (95% CI 0.5566–0.6283) and 2, respectively (Fig. 1). In any scores, the area under the ROC curve analysis showed low accuracy of predictability for risk of thromboembolic and bleeding events.
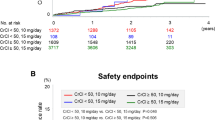
The results of the incidence rates and univariate analysis using Cox proportional hazards model are shown in Tables 2 and 3. The results of the multivariate analysis using the Cox proportional hazards model are summarized in Fig. 2. The CHADS2, CHA2DS2-VASc and HAS-BLED scores showed a significant difference in univariate analysis, although those factors were not included for multivariate analysis due to a high correlation coefficient. Only prior history of stroke (ischemic/hemorrhagic) was associated with stroke/SE (HR 3.2, 95% CI 2.3–4.4, p < 0.0001), but other components of CHA2DS2-VASc score were not (Fig. 2a). By contrast, several components of HAS-BLED score were associated with major bleeding (Fig. 2b). Among them were age ≥ 65 years, liver dysfunction, history/disposition of bleeding, and concomitant use of antiplatelet drugs. Additionally, CrCl of 30–49 mL/min and < 30 mL/min was independently associated with major bleeding. Renal dysfunction was not included in both univariate and multivariate analysis due to the small number of patients (7 patients) with this diagnosis and events (stroke/SE; 0 event, major bleeding; 3 events) (Table 1).
Discussion
The major findings of the present sub-analysis of EXPAND Study are as follows. First, the CHADS2, CHA2DS2-VASc, and HAS-BLED scores were of low accuracy for assessment of thromboembolic and bleeding events verifying by ROC curve analysis. However, the incidence rate in patients with high score was significantly increased compared with those with low score. Second, among Japanese NVAF patients receiving Japan-specific dosages of rivaroxaban, some components of HAS-BLED score were independently associated with major bleeding. Among them were age, liver dysfunction, history/disposition of bleeding, age ≥ 65 years, and concomitant use of antiplatelet agents. Additionally, lower values of creatinine clearance (CrCl) were associated with major bleeding. Third, only prior history of stroke emerged as an independent predictor of stroke/SE, but other components of CHA2DS2-VASc score did not so.
Predictors of major bleeding
Several components of HAS-BLED score were associated with major bleeding as expected. In the present sub-analysis, number of patients clinically having renal dysfunction was small; therefore, we included CrCl values as a possible explanatory variable for multivariate analysis instead of renal dysfunction. Lower CrCl values were associated with major bleeding as expected from the ABC-Bleeding score [17], although HAS-BLED score was superior in evaluating the risk of developing a serious bleeding event for a long time period [18]. In J-RHYTHM Registry, CrCl values < 50 mL/min were associated with major bleeding in univariate analysis; however, they were not so in multivariate analysis [19].
Since a substantial portion of DOAC is excreted through the kidney, CrCl values could be closely associated with bleeding events. However, the relation between CrCl values and rivaroxaban dosage was not determined thoroughly in this sub-analysis, and further investigation should be conducted. The present study showed that patient with off-label dosage of rivaroxaban has approximately 24% and 2% in under-dosage and over-dosage, respectively. We plan to clarify the relationship between renal function and dosage of rivaroxaban in the ongoing exploratory analyses of our study.
Predictors of thromboembolic events
Multivariate analysis revealed that the history of stroke alone was associated with stroke/SE. In the pooled analysis of data from J-RHYTHM Registry, Fushimi AF Registry, and Shinken Database [4], age ≥ 75 years, HT and history of stroke/TIA emerged as independent predictor of ischemic stroke for Japanese patients with NVAF not using anticoagulants. Furthermore, the Fushimi AF Registry reported that not only age and history of stroke, but also unstable heart failure (HF) (within 30 days after hospitalization due to HF), type B natriuretic peptide (BNP) level, or N-terminal fragment of the prohormone B natriuretic peptide (NT-pro BNP) level were independent risk factors [20].
In the main analysis of EXPAND Study [16], the incidence rate of stroke/SE increased along with an increase in CHA2DS2-VASc score. However, the incidence rate of stroke/SE was too low to determine impact of each component on incident stroke/SE in patients receiving rivaroxaban. The incidence of stroke in Japanese patients has been decreasing because of appropriate management of salt intake and blood pressure (BP), as well as decreased smoking rate [21]. In the present study, the proportion of patients complicated with HT using antihypertensive medications was 94.5%, which is higher than that of general Japanese patients with HT aged 60–69 years (65.6%) and aged 70–79 years (80.8%) in 2010 [22]. The patients complicated with HT may be the not-at-risk population for stroke if they undergo optimal antihypertensive treatment [22]. A sub-analysis of the J-RHYTHM Registry [23] clearly indicated BP control was closely associated with thromboembolic events as well as bleeding events. Although the proportion of patients with baseline systolic BP of ≥ 160 mmHg was quite low, i.e., 4.6%, information for BP control was not collected during the follow-up period in the present study. The patients of this study were treated with rivaroxaban, mostly treated by a cardiologist or a physician who was interested in anticoagulation. Therefore, it is possible that the patient’s condition was being well and the incidence rate of thromboembolic events were lower than patients who were not so.
Predictability of thromboembolic and bleeding events
The present sub-analysis showed that CHADS2, CHA2DS2-VASc, and HAS-BLED scores had low accuracy of predictability for thromboembolic and bleeding events in patients treated with rivaroxaban under daily clinical practice verifying by ROC curve analysis. However, the other analyses of this study showed that the incidence rates increased with the higher score [16], and the rate was higher in the patients with high score than in those with low score (Tables 2 and 3). Although the ROC curve analysis did not show predictability for thromboembolism and bleeding events, the scores have enough predictability for those in NVAF patients treated with rivaroxaban. Additional clinical trials may be needed to develop highly predictive tool for thromboembolic and bleeding events in NVAF patients treated with DOACs.
Study limitations
The present study had several limitations [15, 16]. First, several biases may have affected the present results. For instance, rivaroxaban-naïve as well as rivaroxaban-experienced patients were included. Second, patients who were switched to other oral anticoagulants from rivaroxaban and did not continue anticoagulation were included. Third, only clinical risk factors were selected for multivariate analysis, and laboratory data except for CrCl such as NT-pro BNP, growth differentiation factor-15, high-sensitivity cardiac troponin T, prothrombin time and hemoglobin [7, 24, 25] were not included. Finally, detailed information for management of comorbidities such as HF, HT, and DM during the follow-up period was not collected. In addition, incident comorbidities during the follow-up period could have affected event rates [26]; however, only the baseline clinical characteristics were used for the analysis in the present study.
Conclusions
This sub-analysis showed that some components of the HAS-BLED score were independently associated with major bleeding in Japanese NVAF patients receiving anticoagulation therapy by rivaroxaban. Although the ROC curve analysis did not show accurate predictability for thromboembolic and bleeding events, the scores are effective for evaluating risk of thromboembolism and bleeding in NVAF patients treated with rivaroxaban. Additionally, CrCl value of 30–49 mL/min was an independent predictor of major bleeding in patients receiving rivaroxaban. Only prior history of stroke emerged as an independent predictor of stroke/SE, but other components of CHA2DS2-VASc score did not so.
Change history
02 August 2019
In the original publication of the article, the Figure 2b and the Tables 2 and 3 were published incorrectly. The corrected figure and tables are provided below.
Abbreviations
- AF:
-
Atrial fibrillation
- BP:
-
Blood pressure
- BNP:
-
Brain-type natriuretic peptide
- CI:
-
Confidence interval
- CrCl:
-
Creatinine clearance
- DM:
-
Diabetes mellitus
- DOAC:
-
Direct oral anticoagulants
- DVT:
-
Deep vein thromboembolism
- CHF:
-
Congestive heart failure
- HR:
-
Hazard ratio
- HF:
-
Heart failure
- HT:
-
Hypertension
- ROC:
-
Receiver operating characteristic
- ISTH:
-
International Society on Thrombosis and Haemostasis
- MI:
-
Myocardial infarction
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- NVAF:
-
Non-valvular atrial fibrillation
- NT-pro BNP:
-
N-terminal fragment of the prohormone brain-type natriuretic peptide
- PAD:
-
Peripheral arterial disease
- PAF:
-
Paroxysmal atrial fibrillation
- PE:
-
Pulmonary embolism
- SD:
-
Standard deviation
- SE:
-
Systemic embolism
- TIA:
-
Transient ischemic attack
References
Inoue H, Fujiki A, Origasa H, Ogawa S, Okumura K, Kubota I, Aizawa Y, Yamashita T, Atarashi H, Horie M, Ohe T, Doi Y, Shimizu A, Chishaki A, Saikawa T, Yano K, Kitabatake A, Mitamura H, Kodama I, Kamakura S (2009) Prevalence of atrial fibrillation in the general population of Japan: an analysis based on periodic health examination. Int J Cardiol 137:102–107
Sakamoto T, Inoue H (2013) Epidemiology and prognosis of atrial fibrillation in Japanese population. Nihon Rinsho 71:15–20 (in Japanese)
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285:2864–2870
Suzuki S, Yamashita T, Okumura K, Atarashi H, Akao M, Ogawa H, Inoue H (2015) Incidence of ischemic stroke in Japanese patients with atrial fibrillation not receiving anticoagulation therapy–pooled analysis of the Shinken Database, J-RHYTHM Registry, and Fushimi AF Registry. Circ J 79:432–438
Inoue H, Nozawa T, Hirai T, Iwasa A, Okumura K, Lee JD, Shimizu A, Hayano M, Yano K (2006) Accumulation of risk factors increases risk of thromboembolic events in patients with nonvalvular atrial fibrillation. Circ J 70:651–656
European Heart Rhythm Association, European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De Caterina R, De Sutter J, Goette A, Gorenek B, Heldal M, Hohloser SH, Kolh P, Le Heuzey JY, Ponikowski P, Rutten FH (2010) Guidelines for the management of atrial fibrillation: the Task Force for the management of atrial fibrillation of the European society of cardiology (ESC). Eur Heart J 31:2369–2429
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, ESC Scientific Document Group (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37:2893–2962
Yoshizawa R, Komatsu T, Kunugita F, Ozawa M, Ohwada S, Satoh Y, Morino Y, Nakamura M (2017) Comparison of the CHADS2, CHA2DS2-VASc and R2CHADS2 scores in Japanese patients with non-valvular paroxysmal atrial fibrillation not receiving anticoagulation therapy. Intern Med 56:2827–2836
Tomita H, Okumura K, Inoue H, Atarashi H, Yamashita T, Origasa H, Tsushima E, Registry Investigators J-RHYTHM (2015) Validation of risk scoring system excluding female sex from CHA2DS2-VASc in Japanese patients with nonvalvular atrial fibrillation—subanalysis of the J-RHYTHM Registry. Circ J 79:1719–1726
Okumura K, Inoue H, Atarashi H, Yamashita T, Tomita H, Origasa H, Registry Investigators J-RHYTHM (2014) Validation of CHA2DS2-VASc and HAS-BLED scores in Japanese patients with nonvalvular atrial fibrillation: an analysis of the J-RHYTHM Registry. Circ J 78:1593–1599
Senoo K, Lane DA, Lip GY (2015) Stroke risk reduction with oral anticoagulation using CHA2DS2-VASc in a Japanese AF population: a modeling analysis. Int J Cardiol 181:247–254
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138:1093–1100
Lip GYH, Skjøth F, Nielsen PB, Jældgaard JN, Larsen TB (2018) The HAS-BLED, ATRIA, and ORBIT bleeding scores in atrial fibrillation patients using non-vitamin K antagonist oral anticoagulants. Am J Med 131:574.e13–574.e27
JCS Joint working group (2014) Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J 78:1997–2021
Ikeda T, Atarashi H, Inoue H, Uchiyama S, Kitazono T, Yamashita T, Shimizu W, Kamouchi M, Kaikita K, Fukuda K, Origasa H, Sakuma I, Saku K, Okumura Y, Nakamura Y, Morimoto H, Matsumoto N, Tsuchida A, Ako J, Sugishita N, Shimizu S, Shimokawa H (2016) Study design and baseline characteristics of the EXPAND Study: evaluation of effectiveness and safety of Xa inhibitor, rivaroxaban for the prevention of stroke and systemic embolism in a nationwide cohort of Japanese patients diagnosed as non-valvular atrial fibrillation. Tohoku J Exp Med 240:259–268
Shimokawa H, Yamashita T, Uchiyama S, Kitazono T, Shimizu W, Ikeda T, Kamouchi M, Kaikita K, Fukuda K, Origasa H, Sakuma I, Saku K, Okumura Y, Nakamura Y, Morimoto H, Matsumoto N, Tsuchida A, Ako J, Sugishita N, Shimizu S, Atarashi H, Inoue H (2018) The EXPAND study: efficacy and safety of rivaroxaban in Japanese patients with non-valvular atrial fibrillation. Int J Cardiol 258:126–132
Hijazi Z, Oldgren J, Lindbäck J, Alexander JH, Connolly SJ, Eikelboom JW, Ezekowitz MD, Held C, Hylek EM, Lopes RD, Siegbahn A, Yusuf S, Granger CB, Wallentin L, ARISTOTLE and RE-LY Investigators (2016) The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet 387:2302–2311
Esteve-Pastor MA, Rivera-Caravaca JM, Roldan V, Vicente V, Valdés M, Marín F, Lip GYH (2017) Long-term bleeding risk prediction in ‘real world’ patients with atrial fibrillation: comparison of the HAS-BLED and ABC-bleeding risk scores. the Murcia Atrial Fibrillation Project. Thromb Haemost 117:1848–1858
Kodani E, Atarashi H, Inoue H, Okumura K, Yamashita T, Origasa H, Registry Investigators J-RHYTHM (2018) Impact of creatinine clearance on outcomes in patients with non-valvular atrial fibrillation: a subanalysis of the J-RHYTHM Registry. Eur Heart J Qual Care Clin Outcomes 4:59–68
Iguchi M, Tezuka Y, Ogawa H, Hamatani Y, Takagi D, An Y, Unoki T, Ishii M, Masunaga N, Esato M, Tsuji H, Wada H, Hasegawa K, Abe M, Lip GYH, Akao M (2018) Incidence and risk factors of stroke or systemic embolism in patients with atrial fibrillation and heart failure—the Fushimi AF Registry. Circ J 82:1327–1335
Kokubo Y (2017) Trends in stroke in Japan and abroad. Jpn J Cardiovasc Dis Prev 52:223–232 (in Japanese)
Miura K, Nagai M, Ohkubo T (2013) Epidemiology of hypertension in Japan: where are we now? Circ J 77:2226–2231
Kodani E, Atarashi H, Inoue H, Okumura K, Yamashita T, Otsuka T, Tomita H, Origasa H, Registry Investigators J-RHYTHM (2016) Impact of blood pressure control on thromboembolism and major hemorrhage in patients with nonvalvular atrial fibrillation: a subanalysis of the J-RHYTHM Registry. J Am Heart Assoc 5(9):e004075
Hijazi Z, Oldgren J, Andersson U, Connolly SJ, Ezekowitz MD, Hohnloser SH, Reilly PA, Vinereanu D, Siegbahn A, Yusuf S, Wallentin L (2012) Cardiac biomarkers are associated with an increased risk of stroke and death in patients with atrial fibrillation: a randomized evaluation of long-term anticoagulation therapy (RE-LY) substudy. Circulation 125:1605–1616
Hijazi Z, Lindbäck J, Alexander JH, Hanna M, Held C, Hylek EM, Lopes RD, Oldgren J, Siegbahn A, Stewart RA, White HD, Granger CB, Wallentin L, ARISTOTLE and STABILITY Investigators (2016) The ABC (age, biomarkers, clinical history) stroke risk score: a biomarker-based risk score for predicting stroke in atrial fibrillation. Eur Heart J 37:1582–1590
Chao TF, Lip GYH, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Chen SA (2018) Relationship of aging and incident comorbidities to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol 71:122–132
Funding
The EXPAND Study is an investigator-initiated clinical study based on a collaborative contract with, Tohoku University Hospital and Bayer Yakuhin Ltd. The company had no role in the study design, study conduct, data collection, data analysis, or manuscript preparation or submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
IS has received personal fees from Bayer and Takeda, outside the submitted work. AT and KK have nothing to disclose. HI has received personal fees from Bayer Healthcare, Boehringer Ingelheim, Daiichi-Sankyo, and Bristol-Myers Squibb, outside the submitted work. SU has received personal fees from Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo, Sanofi, Dainippon Sumitomo, Otsuka, Takeda, Astellas, AstraZeneca, Sanwa Kagaku, Shionogi, Mitsubishi Tanabe, and Pfizer, outside the submitted work. TK has received grants and personal fees from Daiichi Sankyo, Bayer Yakuhin, Pfizer, Chugai, Boehringer Ingelheim, Mitsubishi Tanabe, Shionogi, Astellas, and MSD; personal fees from Bristol-Myers Squibb, Sanofi, and AstraZeneca; and grants from Takeda, Kissei, Kyowa Hakko Kirin, EA Pharma, Asahi Kasei Medical, Otsuka, Torii, Eisai, Ono, Zeria, and Dainippon Sumitomo, outside the submitted work. TY has received grants and personal fees from Bayer, Daiichi Sankyo, Bristol-Myers Squibb, and Mitsubishi Tanabe; and personal fees from Pfizer, Eisai, Ono Pharmaceutical, Toa Eiyo, and Nippon Boehringer, outside the submitted work. WS has received grants and personal fees from Bayer, Daiichi Sankyo, Nippon Boehringer, Bristol-Myers Squibb, Pfizer, Eisai, Ono Pharmaceutical, and Mitsubishi Tanabe, outside the submitted work. TI reports grants and personal fees from Daiichi-Sankyo, personal fees from Bayer, grants and personal fees from Bristol-Myers Squibb, personal fees from Pfizer, grants from Boehringer Ingelheim, outside the submitted work. MK has received personal fees from Tohoku University, during the conduct of the study; and personal fees from Bayer, outside the submitted work. KF has received personal fees from Bayer, outside the submitted work. HO has received personal fees from Daiichi-Sankyo and Bayer, outside the submitted work. HS has received personal fees from Bayer, and Daiichi Sankyo, outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sakuma, I., Uchiyama, S., Atarashi, H. et al. Clinical risk factors of stroke and major bleeding in patients with non-valvular atrial fibrillation under rivaroxaban: the EXPAND Study sub-analysis. Heart Vessels 34, 1839–1851 (2019). https://doi.org/10.1007/s00380-019-01425-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01425-x