Abstract
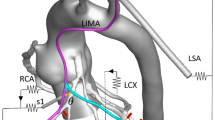
Distal anastomosis technique affects graft patency and long-term outcomes in coronary artery bypass grafting, however, there is no standard for the appropriate length of distal anastomosis. The purpose of this study is to evaluate whether longer distal anastomosis provides higher quality of distal anastomosis and better hemodynamic patterns. Off pump CABG training simulator, YOUCAN (EBM Corporation, Japan), was used for distal anastomosis model. Two lengths of distal anastomosis model (10 versus 4 mm) were prepared by end-to-side anastomosis technique. After CT scan constructed three-dimensional inner shape of distal anastomosis, computational flow dynamics (CFD) was used to analyze hemodynamic patterns. The working flow was defined as Newtonian fluid with density of 1050 kg/m3 and viscosity of 4 mPa s. The boundary condition was set to 100 mmHg at inlet, 50 ml/min at outlet, and 100 % stenosis of proximal coronary artery. Three-dimensional CT imaging showed quality of distal anastomosis in 10 mm model was more uniform without vessel wall inversion or kinking compared to 4 mm model. Anastomotic flow area was significantly larger in 10 mm model than that in 4 mm model (28.67 ± 4.91 versus 8.89 ± 3.18 mm2, p < 0.0001). Anastomotic angle was significantly smaller in 10 mm model compared to 4 mm model (10.2 ± 5.65° versus 20.6 ± 3.31°, p < 0.0001). CFD analysis demonstrated 10 mm model had streamlined flow with smooth graft curvature, whereas 4 mm model had abrupt blood flow direction changes with flow separation at the toe. 10 mm model had significantly lower energy loss than 4 mm model (34.78 ± 6.90 versus 77.10 ± 21.47 μW, p < 0.0001). Longer distal anastomosis provided higher quality of distal anastomosis, larger anastomotic flow area, smaller anastomotic angle, and smoother graft curvatures. These factors yielded lower energy loss at distal anastomosis.






Similar content being viewed by others
References
Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR Jr, Morel MA, Van Dyck N, Houle VM, Dawkins KD, Serruys PW (2013) Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 381:629–638
Bisleri G, Di Bacco L, Giroletti L, Muneretto C (2016) Total arterial grafting is associated with improved clinical outcomes compared to conventional myocardial revascularization at 10 years follow-up. Heart Vessels. doi:10.1007/s00380-016-0846-6
Gatti G, Dell’Angela L, Benussi B, Dreas L, Forti G, Gabrielli M, Rauber E, Luzzati R, Sinagra G, Pappalardo A (2016) Bilateral internal thoracic artery grafting in octogenarians: where are the benefits? Heart Vessels 31:702–712
Hayward PA, Buxton BF (2007) Contemporary coronary graft patency: 5-year observational data from a randomized trial of conduits. Ann Thorac Surg 84:795–799
Zhang L, Hagen PO, Kisslo J, Peppel K, Freedman NJ (2002) Neointimal hyperplasia rapidly reaches steady state in a novel murine vein graft model. J Vasc Surg 36:824–832
Kalan JM, Roberts WC (1990) Morphologic findings in saphenous veins used as coronary arterial bypass conduits for longer than 1 year: necropsy analysis of 53 patients, 123 saphenous veins, and 1865 five-millimeter segments of veins. Am Heart J 119:1164–1184
Clowes AW, Reidy MA, Clowes MM (1983) Kinetics of cellular proliferation after arterial injury. I. Smooth muscle growth in the absence of endothelium. Lab Invest 49:327–333
Liu MW, Roubin GS, King SB 3rd (1989) Restenosis after coronary angioplasty. Potential biologic determinants and role of intimal hyperplasia. Circulation 79:1374–1387
Keynton RS, Evancho MM, Sims RL, Rodway NV, Gobin A, Rittgers SE (2001) Intimal hyperplasia and wall shear in arterial bypass graft distal anastomoses: an in vivo model study. J Biomech Eng 123:464–473
Ballyk PD, Walsh C, Butany J, Ojha M (1998) Compliance mismatch may promote graft-artery intimal hyperplasia by altering suture-line stresses. J Biomech 31:229–237
Clowes AW, Kirkman TR, Clowes MM (1986) Mechanisms of arterial graft failure. II. Chronic endothelial and smooth muscle cell proliferation in healing polytetrafluoroethylene prostheses. J Vasc Surg 3:877–884
Bonert M, Myers JG, Fremes S, Williams J, Ethier CR (2002) A numerical study of blood flow in coronary artery bypass graft STS anastomoses. Ann Biomed Eng 30:599–611
Qiao A, Liu Y (2006) Influence of graft-host diameter ratio on the hemodynamics of CABG. Biomed Mater Eng 16:189–201
Brien TO, Walsh M, McGloughlin T (2005) On reducing abnormal hemodynamics in the femoral ETS anastomosis: the influence of mechanical factors. Ann Biomed Eng 33:310–322
Fei DY, Thomas JD, Rittgers SE (1994) The effect of angle and flow rate upon hemodynamics in distal vascular graft anastomoses: a numerical model study. J Biomech Eng 116:331–336
Hughes PE, How TV (1996) Effects of geometry and flow division on flow structures in models of the distal ETS anastomosis. J Biomech 29:855–872
Staalsen NH, Ulrich M, Winther J, Pedersen EM, How T, Nygaard H (1995) The anastomosis angle does change the flow fields at vascular ETS anastomoses in vivo. J Vasc Surg 21:460–471
Keynton RS, Rittgers SE, Shu MC (1991) The effect of angle and flow rate upon hemodynamics in distal vascular graft anastomoses: an in vitro model study. J Biomech Eng 113:458–463
Pietrabissa R, Inzoli F, Fumero R (1990) Simulation study of the fluid dynamics of aorto-coronary bypass. J Biomed Eng 12:419–424
Freshwater IJ, Morsi YS, Lai T (2006) The effect of angle on wall shear stresses in a LIMA to LAD anastomosis: numerical modeling of pulsatile flow. Proc Inst Mech Eng H 220:743–757
Smits AJ (1999) A physical introduction to fluid mechanics. Wiley, New York, pp 68–69
Taylor RS, Loh A, McFarland RJ, Cox M, Chester JF (1992) Improved technique for polytetrafluoroethylene bypass grafting: long-term results using anastomotic vein patches. Br J Surg 79:348–354
Lei M, Archie JP, Kleinstreuer C (1997) Computational design of a bypass graft that minimizes wall shear stress gradients in the region of the distal anastomosis. J Vasc Surg 25:637–646
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Tsukui, H., Shinke, M., Park, Y.K. et al. Longer coronary anastomosis provides lower energy loss in coronary artery bypass grafting. Heart Vessels 32, 83–89 (2017). https://doi.org/10.1007/s00380-016-0880-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0880-4