Abstract
The use of haptic simulation for emergency procedures in nursing training presents a viable, versatile and affordable alternative to traditional mannequin environments. In this paper, an evaluation is performed in a virtual environment with a head-mounted display and haptic devices, and also with a mannequin. We focus on a chest decompression, a life-saving invasive procedure used for trauma-associated cardiopulmonary resuscitation (and other causes) that every emergency physician and/or nurse needs to master. Participants’ heart rate and blood pressure were monitored to measure their stress level. In addition, the NASA Task Load Index questionnaire was used. The results show the approved usability of the VR environment and that it provides a higher level of immersion compared to the mannequin, with no statistically significant difference in terms of cognitive load, although the use of VR is perceived as a more difficult task. We can conclude that the use of haptic-enabled virtual reality simulators has the potential to provide an experience as stressful as the real one while training in a safe and controlled environment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Nursing schools face the challenge of training their students on a variety of skills that they must master by the end of their studies. In the case of rarely performed procedures, they will also have to continue practicing them even after they have completed their academic training because skills are refined through their repeated use, as well as for cases where new equipment is introduced. Simulation-based interventions often require the use of expensive resources, however, such as custom-made mannequins that are designed for a particular procedure. We have been investigating the feasibility of using more affordable resources based on Virtual Reality (VR) that can be deployed at nursing schools, providing them with a training opportunity that can be applied to a variety of procedures from the same general platform. This platform consists of a head-mounted display (HMD) and haptic devices as a means of interaction. VR allows a high level of immersion and more possibilities for scenario variations than using a mannequin. Our first prototype demonstrated the potential of this approach [22].
This paper describes an experiment that studies the same procedure carried out in two different simulation environments. The first one uses a mannequin and the second one uses our latest VR simulator scenario called ParaVR. What is innovative about this simulator is the combination of a 360\(^\circ \) immersive environment with the use of haptic devices for the interaction. Haptics pertains to the sense of touch and covers both tactile and force feedback. The use of haptics in a training simulator is not new [8] and there are many examples in the medical domain [7]. However, to the authors’ knowledge, there are no simulations of medical procedures that combine HMDs with the use of desktop force feedback devices that allow haptic interaction with the entire scene.
We focus on a chest decompression, a life-saving invasive procedure that every nurse needs to be able to carry out. It involves inserting a special type of needle into a predefined location on the chest. Haptic feedback is crucial when training this technique, as nurses are guided largely by their sense of touch while making the insertion. A grounded force feedback haptic device such as the 3D Systems Inc. (Rock Hill, South Carolina) Touch is the most suitable for this task—see Fig. 1. Through the manipulation of the end-effector stylus, the trainee can move the virtual tool used in the procedure (input) and feel the forces applied to the virtual tool as it is inserted into the chest (force output).
This study presents the improved version of ParaVR needle decompression simulator. The first goal is to validate its usability in order to be used as a training tool. The second goal is to measure the level of stress produced using the ParaVR compared to a classic mannequin. At this point, the simulated environment should be able to generate, at least, the same level of stress as the mannequin environment. Otherwise, it would mean that the simulation did not produce the desired immersion.
In the next section, we summarize related work and discuss the limitations of using a grounded force feedback device as the main interaction mechanism in immersive VR environments. Section 3 provides the detail of our new ParaVR implementation and how it has been adapted with a new approach for supporting haptic devices. Section 4 describes the validation study carried out with senior nursing students at the University of León (Spain). In Sect. 5, the results of the study are shown and the paper concludes with a discussion followed by conclusions and plans for future work.
2 Background
In the past 5 years, cost-effective HMDs for immersive VR have become readily available. They are typically used in combination with two hand controllers that can be tracked, or more recently by directly tracking the users hands. HMDs can be tetherless and contain an in-built computer for running the VR application. Those HMDs connected to a host computer (wired or wireless) can take advantage of the full computational power of the host PC’s graphics card and CPU. Surround sound support is also integrated into the headsets.
Providing force feedback within immersive VR is more of a challenge. The hand controllers contain lightweight vibrotactile actuators such as linear resonant actuators or eccentric revolution motors. These mostly provide just tactile feedback but have been used to simulate force feedback (e.g., [25]). The most common option currently available for force feedback is to use a grounded device such as the 3D Systems Touch (formerly called the SensAble Technologies PHANToM Omni). This device has been available in different forms for over twenty years [19] but has not been designed for immersive VR. It offers six degrees of freedom for input gestures, and three degrees of freedom for force output (up to 3.3 N). The work space of the Touch is constrained by the physical movement possible of the end-effector stylus, which is 16 cm\(\times \)12 cm\(\times \)7 cm (W\(\times \)H\(\times \)D). A third option is to use force feedback gloves such the NOVA from SenseGlove (Delft, The Netherlands). This glove uses four magnetic friction brakes on each finger to deliver up to 20N of force. Haptic gloves are still in development, however, and the fidelity of the force experienced is not always convincing. All three of these devices were available for the ParaVR project and a comparison is summarized in Table 1.
Based on the fidelity of the force feedback and cost, the Touch device was selected for this project. The challenge is then to integrate such a device seamlessly into a potentially much larger virtual work space. One approach is to change the Control-Display Gain (CDG) so that small movements of the haptics end effector are mapped onto much larger movements in the virtual space. Li et al. [17] have shown that this will reduce task completion time at the cost of task accuracy and could negatively influence user confidence in completing the task.
Another approach is called the “bubble" technique [10] and is used to relocate the device work space, which is displayed visually using a semi-transparent sphere (the bubble). When the end-effector is located inside the bubble, its motion is position controlled with direct mapping of the end-effector’s motion to the location of the bubble. When outside the bubble it is rate controlled and uses a faster coarser positioning of the bubble. Force feedback is applied when crossing the surface of the bubble. However, this feedback comes from the technique itself and does not feel realistic. It can alter the users’ perception, which is not desirable in medical simulation. Also, the bubble technique does not perform well when using it in immersive VR. The bubble, or the haptic work space, is never mapped to the user’s point of view or head orientation. This can cause situations in which from the point of view of the user, they push the haptic stylus forward but the bubble moves from left to right.
If eye tracking hardware is available, then gaze interaction can be used to relocate the device work space. Li et al.’s [16] gaze-switching workplace approach allows the user to gaze at a target in the VR scene for a predefined period of time, resulting in the device work space being relocated and locked onto this target. They obtained an improvement in interaction efficiency, kinaesthetic perception accuracy and overall user experience. However, it is noted that they used a CDG of 4 in this work and so the positional accuracy would have been reduced. Eye tracking hardware is starting to be integrated into high-end HMDs such as the HP Reverb G2 Omnicept Edition and HTC Vive Pro Eye, or can be purchased as an add on. This functionality is not yet available for the entry-level HMDs.
Regarding the use of VR in the training of medical procedures, its usefulness has been already proved in different studies. It has been used in teaching both theory and skills of RPC procedure [2, 6], highlighting its high effectiveness in teaching and practicing this procedure [1]. Virtual reality training has also been compared with classic training scenarios for other procedures [9], even in combination with basic haptic devices [27]. VR can improve nursing staff competencies [11] and can deliver as stressful environments as the reality [18], making it ideal for use in the training of the needle decompression procedure that usually has to be performed in this type of environments.
With a focus on needle decompression to release tension in pneumothoraces, we find in the literature that bespoke solutions have been used such as a wrist-worn haptic device, which is specially designed for the simulation of forces on the wrist of the hand holding a physical needle equipped with a magnetic tracker [24]. An approach to needle insertion training with haptic devices has also been applied to telementoring, as is shown in [23]. This work allows a mentor to feel the forces being applied by the trainee in real time. Although their application in online environments is very useful, the use of specific devices, such as the force sensing attachment required on the trainee’s needle or the prototype guidance feedback glove, offer a specific and non-generalist solution. Similarly, it does not address the problem of choosing the exact puncture point. In our study, we use a commercial off-the-shelf device to provide as general an environment as possible. Other techniques, such as augmented reality, have been shown to have a positive impact on assisting in the treatment of tension pneumothoraces. A study conducted in a military environment reports that the use of augmented reality goggles improves the performance of the procedure with a slight increase in time that did not reach statistical significance [26].
The current gold standard for training many medical procedures is to use conventional mannequins. However, doubts have been raised about the suitability of mannequins for this particular procedure. In [5], the result of a systematic literature review concludes that mannequin chests are not an accurate representation of the human chest when used for decompressing a tension pneumothorax and therefore may not provide a realistic experience. In particular, chest wall thickness in adults varies and this variation can easily be included in a VR environment, unlike physical models.
3 ParaVR simulator description
ParaVR [12, 22], a prototype developed for paramedics focused on training and skills retention, has been used as the basis for the development of this new version of the simulator.
3.1 Needle decompression
The needle decompression is a procedure performed by healthcare professionals as the treatment of tension pneumothorax, that is, when the air accumulates in the pleural cavity—between the lungs and the chest wall—due to a chest trauma.
The procedure involves inserting a needle and catheter into the patient’s chest to allow the air to escape and decrease pressure. The insertion should be made in the second intercostal space (between the second and the third ribs), slightly closer to the third rib than to the second, and at the mid-clavicular line. The needle should pass through the chest wall as perpendicular as possible and it must be inserted until the pleura is reached and the air can be heard coming out. At that point, the needle should be removed, leaving the catheter in place.
3.2 Scene development
ParaVR has been built by recreating the scene of a traffic accident in the Unity Engine (Unity Technologies, San Francisco, CA). It includes sound effects of passing traffic and general nature sounds to add an extra feeling of immersion. Third party models have been used for the scene—see Fig. 2. The patient model has been placed on a stretcher, at a suitable height to allow the use of the haptic device placed on a table in the real world to interact with it in a natural way.
As explained in the previous section, the 3D Systems Touch device has been selected as the haptic interaction device for ParaVR. It is an affordable force feedback device and the stylus arm has six degrees of freedom, which is essential for its use in positioning a medical instrument. In addition, the stylus can also be replaced with 3D printed models of the real tools used in the procedure as we have done in previous work [3]. To use this device within Unity, we imported the official 3D Systems Openhaptics Unity Plugin, which is freely available from the Unity Asset Store. The plugin manages the haptic rendering pipeline. However, a drawback of the Touch device is that the work space is limited to the physical movement of the stylus arm. Changing the CDG allows this limitation to be overcome but this necessitates a trade-off with the realism and accuracy of the interaction. This would be undesirable for ParaVR.
Our approach is to include in the scene a virtual work space matching the dimensions of the real-world Touch work space. This cube-shaped virtual work space is constantly visible to the trainee so that they are aware of the volume within which objects can be touched. In order to be able to haptically interact with any part of the scene, the virtual work space can be repositioned by a combination of pressing the buttons on the Touch and changing the trainee’s point of view by moving their head. The advantage is that in this way neither the level of haptic transparency nor the level of accuracy is affected.
4 Evaluation
To evaluate the applicability and usefulness of ParaVR as a training tool, it has been compared with the traditional approach of using a mannequin. The Laerdal SimMan ALS mannequin was used as it supports the training of needle decompression for tension pneumothorax.
4.1 Subjects
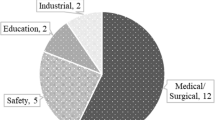
Participants for the experiment were recruited from the students of the School of Nursery from the University of León, Spain. A total of 21 women and 9 men aged between 19 and 34 years performed the evaluation. All of them had learnt and practiced the procedure of needle decompression using SimMan before the experiment. One of the participants was color-blind. Four of them had previous experience of using virtual reality, while none of them had previous experience using haptic devices. Eight of the participants reported that they had visual difficulties that could prevent them from correctly viewing the virtual scene when wearing the HMD.
4.2 Task
Participants had to carry out the needle decompression procedure in order to release the pneumothorax. This procedure is divided into three main subtasks: (1) palpation of the patient’s chest to identify and mark the insertion point, (2) insertion of the needle together with the catheter into the marked point until the correct depth is reached, and (3) separation of the catheter and the needle to remove only the needle, allowing the accumulated air to escape from the patient’s chest. Other subtasks such as cleaning the insertion area and application of local anesthesia may also be performed during the procedure, although they are not mandatory and are performed, or not, depending on the urgency of the decompression.
The procedure is deemed successful if the insertion is made according to the criteria listed in Sect. 3.1. Health care professionals know they have reached the pleural space when the resistance of the needle, as it is inserted into the patient’s chest, decreases dramatically and the air can be heard coming out of the patient’s chest through the catheter.
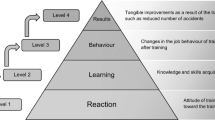
4.3 Assessment instrument
The week before the experiment, all the participants attended a familiarization session on VR and haptic technologies. They learned what these technologies were and how to use the haptic device correctly, including how to move the virtual workspace within the scene, mark the insertion point, change the tool, etc. The ParaVR simulator was presented to them and they had some minutes to freely test all of the functionality included. Some visual aids were added during this training phase. In particular, the ribs were visible, helping in this way to associate what they were touching and what they were seeing (see Fig. 3).
ParaVR was executed in a Windows 10 PC with 16GB of RAM and a NVIDIA GTX 1060 graphics card. The Oculust Quest 2 HMD was used and the haptic device was the 3D Systems Touch.
On the day of the experiment, participants used both the SimMan ALS (Laerdal Medical, Stavanger, Norway) mannequin (scenario 1) and ParaVR simulator (scenario 2) to perform the task. Half of the participants did the scenario 1 first followed by scenario 2, and the other half did scenario 2 first followed by scenario 1. Figure 4 shows one of the participants performing the evaluation on the mannequin and Fig. 5 shows another participant with ParaVR simulator.
All participants signed a consent form to participate in the evaluation. They then completed a questionnaire to collect their socio-demographic data and the questions to address the weighting phase of the NASA TLX, the multidimensional National Aeronautics and Space Administration Task Load Index (NASA-TLX) assessment instrument, a global workload score for a given task [14]. It contains six scales rating for mental, physical, and temporal demands, as well as for performance, effort, and frustration. They were then randomly assigned to either scenario 1 or scenario 2.
In order to examine the feasibility of the proposed VR simulator compared with the simulation with mannequins with regard to the changes in the psychophysiological response, participant’s vital signs—heart rate, systolic and diastolic blood pressure (Omron M6 Confort IT, Spain)—were monitored and recorded before and after performing the procedure. They should already know how the procedure is to be performed, so they were only assisted if they had difficulties operating the VR headset or the haptic device while performing scenario 2. Once the procedure was completed, and after their vital signs had been checked, they were redirected to the scenario that they had not yet performed.
The experiment ended with a questionnaire that included the questions from the NASA TLX scoring phase (both for the mannequin and ParaVR) and four open questions about the advantages and disadvantages of using the two training environments.
5 Results
This section presents the results of the statistical analysis carried out on the data collected during the experiment. All data collected and the results of the statistical analysis are accessible in [13].
Figure 6 shows the usability score that each participant gave to ParaVR. Five of the thirty participants rated the usability below average (i.e., below a score of 68).
The final TLX scores show that there is no statistically significant trend between the use of the mannequin (\(M = 42.6, SD = 17.628\)) and the use of ParaVR (\(M = 46.889, SD = 20.705\)) in terms of cognitive load, \(t(29) = -1.916, p = 0.065 > 0.05\). However, statistically significant trends were observed for the temporal dimension (\(t(29) = -2.536, p = 0.017 < 0.05\), higher in ParaVR), and frustration level dimension (\(t(29) = -2.546, p = 0.016 < 0.05\), higher in ParaVR).
Figure 7 shows a representation of the heart rate values collected during the evaluation. Regarding this vital sign, a statistically significant trend can be seen between the beginning and the end of the procedure in each scenario:
-
Mannequin: \(t(29) = 2.857, p = 0.008 < 0.05\), higher at the beginning
-
ParaVR: \(t(29) = -8.089, p <.001\), higher at the end
And also between the starting-points and the end-points of the two scenarios:
-
Beginning: (\(t(29) = 7.567, p <.001\), higher at the mannequin
-
End: \(t(29) = -2.962, p = 0.006 < 0.05\), higher at the ParaVR simulator
These differences remain among those who started the experiment in the ParaVR simulator, but not for those who started on the mannequin, where no significant differences can be seen between the beginning and the end of the procedure on the mannequin (\(t(14) = 1.665, p = 0.118 > 0.05\)), and between the end of the procedure in each scenario (\(t(14) = 1.461, p = 0.166 > 0.05\)).
In the comparison between the participants who started the evaluation in the mannequin and those who started the evaluation in the ParaVR simulator, a statistically significant trend can be seen in the values taken both at the beginning and at the end of the procedure in the ParaVR simulator:
-
Beginning: \(t(28) = -4.013, p <.001\)
-
End: \(t(28) = -2.344, p = 0.026 < 0.05\)
higher on those who started the evaluation in the ParaVR simulator in both.
Regarding systolic blood pressure, they showed a statistically significant trend between the values recorded at the beginning and between the values recorded at the end of the procedure:
-
Beginning: \(t(29) = -3.917, p <.001\)
-
End: \(t(29) = -4.246, p <.001\)
No differences were found in terms of diastolic blood pressure at the beginning of the procedure (\(t(29) = -1.689, p = 0.102 > 0.05\)). That is not the case for the measurements taken at the end of the procedure, showing a statistically significant trend in terms of diastolic blood pressure between the mannequin (\(t(29) = -2.775, p = 0.01 < 0.05\)).
Finally, Table 2 shows a summary of each participants’ answers to the open questions about the advantages and disadvantages of using the new virtual reality simulator with haptic feedback and the combination of this with classic mannequins. It has been analyzed following the methodology from [21] and guided by the questions raised.
6 Discussion
The results indicate that the use of haptic-enabled virtual reality simulators could replace and/or supplement the use of mannequins for medical procedures learning and training.
Similar scores for perceived cognitive load have been given to both training methods. These are high scores (42.6 for the mannequin and 46.8 for ParaVR), but are within the expected range for complex medical tasks such as the one performed in the evaluation. Differences between the two methods were found only in two of the cognitive load dimensions, temporal and frustration, with the mannequin providing a lower cognitive load score. Regarding these dimensions, the underlying reason may be the fact that by using the simulator, users have to spend an extra amount of time switching tools between hand and stylus, which in the real world does not involve any increase in time. This delay may be at the root of the increased level of frustration.
Regarding the usability, the average score (76.38) is above the threshold for considering it to have an acceptable degree of usability (68) but, as it can be seen in Fig. 6, five participants rated the usability of ParaVR below that threshold. In any case, this is a very good score for the simulator in terms of usability considering that none of the participants had previous experience in the use of haptic devices and only 4 of them had previous experience in the use of VR. The first goal has been achieved and the usability level of ParaVR simulator has been successfully validated. Furthermore, an increase in the level of usability of ParaVR has been observed since the evaluation of the previous version in [12]. It seems clear that the level of usability of ParaVR, and therefore the skill that professionals achieve in its use, increases the more time they spend practicing with it.
Primary findings revealed a statistically significant increase in heart rate regarding baseline levels in both scenarios, being higher in the ParaVR simulator. However, the heart rate did not increase performing the procedure in the mannequin for those participants who started the evaluation in that scenario, probably because they are used to practice with the mannequin and the level of immersion experienced is not as high as in the ParaVR simulator. This is also reinforced by the significant difference between the participants who started the evaluation with the mannequin and those who started with the ParaVR simulator, which shows that those who started on the simulator experienced a higher level of immersion from the very beginning. The cardiovascular response resulting from the overstimulation of the sympathetic nervous system was associated with the activation of the fight-or-flight response. The same physiological arousal has been previously reported in different simulation settings involving sports, military or clinical training. These studies suggested that the physiological stress provoked by simulation environments leads to a subjective response and a psychological effect on participant [15].
This pattern is consistent with the psychometric measures of cognitive load, indicating a more acute psychophysiological response due to the higher levels of immersion provided by the simulation, thus achieving the second goal of this study. [4, 18, 20].
In terms of the qualitative analysis of the data, Table 2 shows that participants believe that the combined use of VR haptic-enabled simulators and mannequins is the best option, with several advantages such as the variety models that can be used, realism, etc., and almost no disadvantages beyond the differences between the two training methods. Interestingly, several participants in the evaluation mentioned the cost of VR simulators with haptics as a disadvantage in their use, both on their own and in combination with the mannequins, when in fact the cost of the environment for the evaluation with the simulator is much cheaper than that of the mannequin.
Among the advantages that participants have seen in using a VR simulator are the fidelity, the variety of techniques that can be trained and the level of immersion that can be achieved. The main drawbacks are the complexity (related to lack of practice) and the lack of realism of the pen-shaped interface for some of the tasks (such as palpation). Overall, the participants have seen great potential in the use of ParaVR and would like to see it used in combination with the mannequin to achieve better training and thus improve their skills.
7 Conclusions and future work
A virtual reality haptic-enabled needle decompression simulator has been presented. It includes a special interaction technique that allows the use of workspace-limited haptic devices as the only input device, while maintaining high levels of accuracy. ParaVR reproduces the clinical situation in which a patient has a pneumothorax so that it can be used to train the chest decompression procedure in a realistic environment.
The evaluation experiment compared the use of ParaVR with the use of a mannequin, the classical method for training this type of procedure. Results have shown that the VR simulator has reached a good level of usability. Physiological values suggest the use of simulator as a more difficult tasks, but this is not reflected in the perceived cognitive load, which is similar between the use of the simulator and the mannequin.
Participants in the evaluation also expressed the perceived advantages of using this technology, such as the possibility to practice different procedures, the realism and fidelity of the scenes and the flexibility it offers.
All of the above leads to the conclusion that virtual reality simulators with force feedback capabilities as ParaVR could replace and/or complement the use of expensive mannequins for learning and training complex medical procedures because it has the potential to deliver a experience as stressful as reality while training in a safe and controlled environment.
Moreover, such simulators can be produced at affordable prices and distance learning applications can also benefit from their use.
Given the success of this evaluation, there are promising lines of research for the future, such as exploring the inclusion of a second haptic device to allow more realistic two-handed interaction. This could help resolve the main discrepancy between performing the procedure in reality and in ParaVR, which is that in reality both hands are used at the same time. Other pending work is to improve the haptic feedback by making the patient’s body model behave as one or more dynamic surfaces, which would increase the realism of what the professionals feel when touching the patient or inserting the needle. Finally, the time needed for trainee nurses (or other clinicians) to learn how to use the technology correctly needs to be minimized, so it is important to work on simplifying explanations and to have training scenarios to guide them in its use.
Data availability
Data collected during the evaluation is available in [13].
References
Artero, P.M.A., Rios, M.P., Greif, R., Cervantes, A.B.O., Gijón-Nogueron, G., Barcala-Furelos, R., Aranda-García, S., Petersen, L.R.: Efficiency of virtual reality for cardiopulmonary resuscitation training of adult laypersons: a systematic review. Medicine 102(4), e32736 (2023)
Barsom, E.Z., Duijm, R., Dusseljee-Peute, L., Landman-van der Boom, E., Van Lieshout, E., Jaspers, M., Schijven, M.P.: Cardiopulmonary resuscitation training for high school students using an immersive 360-degree virtual reality environment. Br. J. Educ. Technol. 51(6), 2050–2062 (2020)
Bello, F., Bulpitt, A., Gould, D.A., Holbrey, R., Hunt, C., How, T., John, N.W., Johnson, S., Phillips, R., Sinha, A., et al.: Imagine-s: imaging guided needle simulation. In: Eurographics 2009-Medical Prize, Eurographics Association, pp 5–8 (2009)
İşbilir, E., Çakır, M.P., Acartürk, C., Tekerek, A.Ş: Towards a multimodal model of cognitive workload through synchronous optical brain imaging and eye tracking measures. Front. Hum. Neurosci. 13, 375 (2019)
Boyle, M.J., Williams, B., Dousek, S.: Do mannequin chests provide an accurate representation of a human chest for simulated decompression of tension pneumothoraxes? World J. Emerg. Med. 3(4), 265 (2012)
Buttussi, F., Chittaro, L., Valent, F.: A virtual reality methodology for cardiopulmonary resuscitation training with and without a physical mannequin. J. Biomed. Inform. 111, 103590 (2020)
Coles, T.R., Meglan, D., John, N.W.: The role of haptics in medical training simulators: a survey of the state of the art. IEEE Trans. Haptics 4(1), 51–66 (2010)
Costales, G.E., Fernández, C., González, M.Á.C., Olivera, V.M.: Learning systems through haptic simulators: a domain expertise approach. Int. J. Eng. Educ. 31(3), 726–735 (2015)
Cowan, A., Chen, J., Mingo, S., Reddy, S.S., Ma, R., Marshall, S., Nguyen, J.H., Hung, A.J.: virtual reality vs dry laboratory models: comparing automated performance metrics and cognitive workload during robotic simulation training. J. Endourol. 35(10), 1571–1576 (2021)
Dominjon, L., Lécuyer, A., Burkhardt, J.M., Andrade-Barroso, G., Richir, S.: The" bubble" technique: interacting with large virtual environments using haptic devices with limited workspace. In: First Joint Eurohaptics Conference and Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems. World Haptics Conference, IEEE, pp 639–640 (2005)
Efendi, D., Apriliyasari, R.W., Prihartami Massie, J.G.E., Wong, C.L., Natalia, R., Utomo, B., Sunarya, C.E., Apriyanti, E., Chen, K.H.: The effect of virtual reality on cognitive, affective, and psychomotor outcomes in nursing staffs: systematic review and meta-analysis. BMC Nurs. 22(1), 1–15 (2023)
Gutiérrez-Fernández, A., Hogan, C., Rees, N., Fernández-Llamas, C., John, N.W.: An immersive haptic-enabled training simulation for paramedics. In: 2022 International Conference on Cyberworlds (CW), IEEE, pp 79–85 (2022)
Gutiérrez-Fernández, A., Fernández-Llamas, C., Vázquez-Casares, A.M., Mauriz-García, E., Riego-del Castillo, V., John, N.W.: Immersive haptic simulation for training nurses in emergency medical procedures - data collected (2023). https://doi.org/10.5281/zenodo.7540444
Hart, S.G., Staveland, L.E.: Development of nasa-tlx (task load index): results of empirical and theoretical research. Adv. Psychol. 52, 139–183 (1988)
Johannessen, E., Szulewski, A., Radulovic, N., White, M., Braund, H., Howes, D., Rodenburg, D., Davies, C.: Psychophysiologic measures of cognitive load in physician team leaders during trauma resuscitation. Comput. Hum. Behav. 111, 106393 (2020)
Li, Z., Akkil, D., Raisamo, R.: Gaze-based kinaesthetic interaction for virtual reality. Interact. Comput. 32(1), 17–32 (2020)
Li, Z., Akkil, D., Raisamo, R.: The impact of control-display gain in kinesthetic search. In: International Conference on Human Haptic Sensing and Touch Enabled Computer Applications, Springer, pp 158–166 (2020b)
Martens, M.A., Antley, A., Freeman, D., Slater, M., Harrison, P.J., Tunbridge, E.M.: It feels real: physiological responses to a stressful virtual reality environment and its impact on working memory. J. Psychopharmacol. 33(10), 1264–1273 (2019)
Massie, T.H., Salisbury, J.K., et al.: The phantom haptic interface: a device for probing virtual objects. In: Proceedings of the ASME winter annual meeting, symposium on haptic interfaces for virtual environment and teleoperator systems, Chicago, IL 55, 295–300 (1994)
Mauriz, E., Caloca-Amber, S., Córdoba-Murga, L., Vázquez-Casares, A.M.: Effect of psychophysiological stress and socio-emotional competencies on the clinical performance of nursing students during a simulation practice. Int. J. Environ. Res. Public Health 18(10), 5448 (2021)
Miles, M.B., Huberman, A.M.: Qualitative Data Analysis: An Expanded Sourcebook. Sage, London (1994)
Rees, N., Vaughan, N., Day, T.W., Dorrington, K., Rees, L., John, N.W.: Paravr: a virtual reality training simulator for paramedic skills maintenance. J. Paramed. Pract. 12(12), 478–486 (2020)
Reyes, L.R., Gavino, P., Zheng, Y., Boehm, J., Yeatman, M., Hegde, S., Park, C., Battaglia, E., Fey, A.M.: Towards telementoring for needle insertion: Effects of haptic and visual feedback on mentor perception of trainee forces. In: 2022 IEEE Haptics Symposium (HAPTICS), pp 1–7 (2022). https://doi.org/10.1109/HAPTICS52432.2022.9765597
Sarac, M., Hallett, K., Saunders, J., Makled, B., Okamura, A.M.: Augmented needle decompression task with a wrist-worn haptic device. In: 2021 IEEE World Haptics Conference (WHC), pp 873–873, (2021). https://doi.org/10.1109/WHC49131.2021.9517260
Schoonmaker, R.E., Cao, C.G.: Vibrotactile force feedback system for minimally invasive surgical procedures. In: 2006 IEEE International Conference on Systems, Man and Cybernetics, vol 3, pp 2464–2469, (2006). https://doi.org/10.1109/ICSMC.2006.385233
Wilson, K.L., Doswell, J.T., Fashola, O.S., Debeatham, W., Darko, N., Walker, T.M., Danner, O.K., Matthews, L.R., Weaver, W.L.: Using Augmented reality as a clinical support tool to assist combat medics in the treatment of tension pneumothoraces. Mil. Med. 178(9), 981–985 (2013). https://doi.org/10.7205/MILMED-D-13-00074
Yu, P., Pan, J., Qin, H., Hao, A., Wang, H.: Real-time suturing simulation for virtual reality medical training. Computer Animation and Virtual Worlds 31(4–5), e1940 (2020)
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gutiérrez-Fernández, A., Fernández-Llamas, C., Vázquez-Casares, A.M. et al. Immersive haptic simulation for training nurses in emergency medical procedures. Vis Comput (2024). https://doi.org/10.1007/s00371-023-03227-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s00371-023-03227-9