Abstract
Purpose
Utilize magnetic resonance defecography (MRD) to analyze the primary pelvic floor dysfunctions in patients with stress urinary incontinence (SUI) associated with pelvic organ prolapse (POP), and in SUI patients with asymptomatic POP.
Method
We performed MRD in both SUI and POP subjects. As a primary analysis, the functional MR parameters were compared between the isolated POP and POP combined SUI groups. As a secondary analysis, the functional MR data were compared between the POP combined SUI and the SUI with asymptomatic POP (isolated SUI) groups.
Results
MRD noted the main characteristics of SUI combined moderate or severe POP, including the shorter closed urethra length (1.87 cm vs. 2.50 cm, p < 0.001), more prevalent urethral hypermobility (112.31° vs. 85.67°, p = 0.003), bladder neck funneling (48.28% vs. 20.51%, p = 0.020), lower position of vesicourethral junction (2.11 cm vs. 1.67 cm, p = 0.030), and more severe prolapse of the posterior bladder wall (6.26 cm vs. 4.35 cm, p = 0.008). The isolated SUI patients showed the shortest length of the closed urethra (1.56 cm vs. 1.87 cm, p = 0.029), a larger vesicourethral angle (153.80° vs. 107.58°, p < 0.001), the more positive bladder funneling (84.85% vs. 48.28%, p = 0.002) and a special urethral opening sign (45.45% vs. 3.45%, p < 0.001).
Conclusions
Patients with SUI accompanying POP primarily exhibit excessive urethral mobility and a shortened urethral closure. SUI patients with asymptomatic POP mainly show dysfunction of the urethra and bladder neck, characterized by the opening of the urethra and bladder neck and a shortened urethral closure.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, [Min Li], upon reasonable request.
References
Baessler K, Christmann-Schmid C, Maher C, Haya N, Crawford TJ, Brown J (2018) Surgery for women with pelvic organ prolapse with or without stress urinary incontinence. Cochrane Database Syst Rev 8(8):013108
Slieker-ten Hove MCP, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME (2019) The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct 20(9):1037–1045
El Sayed RF, Alt CD, Maccioni F, Meissnitzer M, Masselli G, Manganaro L, Vinci V, Weishaupt D, ESUR and ESGAR Pelvic Floor Working Group (2017) Magnetic resonance imaging of pelvic floor dysfunction-joint recommendations of the ESUR and ESGAR Pelvic Floor Working Group. Eur Radiol 27(5):2067–2085
Margulies RU, Hsu Y, Kearney R, Stein T, Umek WH, DeLancey JOL (2006) Appearance of the levator ani muscle subdivisions in magnetic resonance images. Obstet Gynecol 107(5):1064–1069
El Sayed RF, Morsy MM, El Mashed SM, Abdel-Azim MS (2007) Anatomy of the urethral supporting ligaments defined by dissection, histology, and MRI of female cadavers and MRI of healthy nulliparous women. Am J Roentgenol 189(5):1145–1157
Macura KJ, Genadry RR, Bluemke DA (2006) MR imaging of the female urethra and supporting ligaments in assessment of urinary incontinence: spectrum of abnormalities. Radiographics 26(4):1135–1149
Fitzgerald J, Richter LA (2020) The role of MRI in the diagnosis of pelvic floor disorders. Curr Urol Rep 21(7):26
Kanmaniraja D, Arif-Tiwari H, Palmer SL, Kamath A, Lewis SC, Flusberg M, Kobi M, Lockhart ME, Chernyak V (2021) MR defecography review. Abdom Radiol 46(4):1334–1350
Swamy N, Bajaj G, Olliphant SS, Henry JA, Jambhekar K, Pandey T, Ram R (2021) Pelvic floor imaging with MR defecography: correlation with gynecologic pelvic organ prolapse quantification. Abdom Radiol 46(4):1381–1389
Macura KJ, Thompson RE, Bluemke DA, Genadry R (2015) Magnetic resonance imaging in assessment of stress urinary incontinence in women: parameters differentiating urethral hypermobility and intrinsic sphincter deficiency. World J Radiol 7(11):394–404
Salvador JC, Coutinho MP, Venâncio JM, Viamonte B (2019) Dynamic magnetic resonance imaging of the female pelvic floor-a pictorial review. Insights Imaging 10(1):4
Hamahata Y, Akagi K, Maeda T, Nemoto K, Koike J (2022) Management of pelvic organ prolapse (POP) and rectal prolapse. J Anus Rectum Colon 6(2):83–91
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Pollock GR, Twiss CO, Chartier S, Vedantham S, Funk J, Arif Tiwari H (2021) Comparison of magnetic resonance defecography grading with POP-Q staging and Baden-Walker grading in the evaluation of female pelvic organ prolapse. Abdom Radiol 46(4):1373–1380
Roch M, Gaudreault N, Cyr M-P, Venne G, Bureau NJ, Morin M (2021) The female pelvic floor fascia anatomy: a systematic search and review. Life 11(9):900
Howard D, Miller JM, Delancey JO, Ashton-Miller JA (2000) Differential effects of cough, valsalva, and continence status on vesical neck movement. Obstet Gynecol 95(4):535–540
Delancey JOL, Ashton-miller JA (2004) Pathophysiology of adult urinary incontinence. Gastroenterology 126:S23–S32
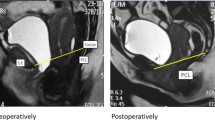
Li M, Wang B, Liu X, Qiao P, Jiao W, Jiang T (2020) MR defecography in the assessment of anatomic and functional abnormalities in stress urinary incontinence before and after pelvic reconstruction. Eur J Radiol 126:108935
Bradley CS, Zimmerman MB, Wang Q, Nygaard IE (2008) Women’s Health Initiative. Vaginal descent and pelvic floor symptoms in postmenopausal women: a longitudinal study. Obstet Gynecol 111(5):1148–1153
Pipitone F, Sadeghi Z, DeLancey JOL (2021) Urethral function and failure: a review of current knowledge of urethral closure mechanisms, how they vary, and how they are affected by life events. Neurourol Urodyn 40(8):1869–1879
Arenholt LTS, Pedersen BG, Glavind K, Glavind-Kristensen M, DeLancey JOL (2017) Paravaginal defect: anatomy, clinical findings, and imaging. Int Urogynecol J 28(5):661–673
Hokanson JA, DeLancey JOL (2022) Urethral failure is a critical factor in female urinary incontinence. Now what? Neurourol Urodyn 41(2):532–538
Ashton-Miller JA, Delancey JOL (2007) Functional anatomy of the female pelvic floor. Ann N Y Acad Sci 1101(1):266–296
McLean L, Varette K, Gentilcore-Saulnier E, Harvey M-A, Baker K, Sauerbrei E (2013) Pelvic floor muscle training in women with stress urinary incontinence causes hypertrophy of the urethral sphincters and reduces bladder neck mobility during coughing. Neurourol Urodyn 32(8):1096–1102
Delancey JO (2010) Why do women have stress urinary incontinence? Neurourol Urodyn 29(Suppl 1):S13–S17
DeLancey JO, Trowbridge ER, Miller JM, Morgan DM, Guire K, Fenner DE, Weadock WJ, Ashton-Miller JA (2008) Stress urinary incontinence: relative importance of urethral support and urethral closure pressure. J Urol 179(6):2286–2290
Stoker J, Rociu E, Bosch JL, Messelink EJ, van der Hulst VP, Groenendijk AG, Eijkemans MJ, Laméris JS (2003) High-resolution endovaginal MR imaging in stress urinary incontinence. Eur Radiol 13(8):2031–2037
Perucchini D, DeLancey JOL, Ashton-Miller JA, Galecki A, Schaer GN (2002) Age effects on urethral striated muscle. II. Anatomic location of muscle loss. Am J Obstet Gynecol 186(3):356–360
Funding
The study was supported by Beijing Municipal Administration of Hospitals Incubating Program, PX 2020015. Author Min Li was supported by the grant.
Author information
Authors and Affiliations
Contributions
Min Li: Design and conception; analysis and interpretation of data; drafting the article; revising the paper. Sumei Wang: POP patients inclusion; interpretation of clinical data for the work; revision of the paper. Biao Wang: SUI patients inclusion: interpretation of clinical data for the work. Tongtong Liu: Acquisition and analysis of MR imaging data for the work. Peng Qiao: Acquisition and analysis of clinical data for the work.
Corresponding authors
Ethics declarations
Conflict of interest
This study was a research article. All authors have read and approved to the submission of “World Journal of Urology” for publication. The authors have no conflicts of interest to declare.
Ethics approval
Research involving human participants. The study protocol was approved by the Ethics Committee of the Beijing Chao Yang Hospital, Capital Medical University. Study-Special written consents were obtained from all the subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, M., Liu, T., Wang, B. et al. MR defecography in assessing stress urinary incontinence with or without symptomatic pelvic organ prolapse. World J Urol 42, 321 (2024). https://doi.org/10.1007/s00345-024-05014-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-05014-0