Abstract
Introduction
Treatment of pelvic organ prolapse (POP) associated with stress urinary incontinence (SUI) is a surgical challenge. Surgeons may perform combined prolapse and incontinence surgery or may correct prolapse first and evaluate incontinence afterwards. We present a prospective study to evaluate the effect of abdominal sacrocolpopexy (ASC) on urethral anatomy and continence using dynamic magnetic resonance imaging (MRI).
Methods
Twenty females with concomitant apical prolapse and SUI due to urethral hypermobility were included. Patients with intrinsic sphincteric deficiency (ISD) were excluded. All patients underwent ASC operation as a sole treatment without anti-incontinence procedure. Patients were informed they may need anti-incontinence procedure afterwards. Symptom-specific questionnaires assessing prolapse, incontinence, sexual function and quality of life (QoL), dynamic MRI and pressure flow urodynamic study were administered before and after surgery.
Results
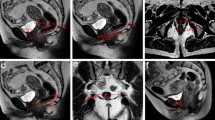
Mean age was 53 years. All patients had apical prolapse; four with cystocele, and five with rectocele. Urethral hypermobility was positive in all patients. After performing ASC, all patients reported significant improvement of all prolapse and incontinence questionnaires as well as QoL and sexual function. Significant improvement of incontinence parameters on dynamic MRI (bladder neck descent, posterior urethrovesical angle and urethral inclination angle) was observed after ASC. Similarly, significant change in the position of the leading edge of prolapse and anorectal junction was observed.
Conclusions
In patients with prolapse and urethral hypermobility, ASC may return bladder neck and urethral anatomy towards normal as proved by dynamic MRI. However, further studies on larger number of patients with longer follow-up period are required.




Similar content being viewed by others
References
Brown JS, Waetjen LE, Subak LL, Thom DH, Van Den Eeden S, Vittinghoff E (2002) Pelvic organ prolapse surgery in the United States. Am J Obstet Gynecol 186:712–716
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed POP and urinary incontinence. Obstet Gynecol 89:501–506
Elliott DS, Frank I, DiMarco DS, Chow GK (2004) Gynecologic use of robotically assisted laparoscopic sacrocolpopexy for the treatment of high-grade vaginal vault prolapse. Am J Surg 188(4A Suppl):52S–56S
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 30(4):CD004014. https://doi.org/10.1002/14651858.CD004014
Van Der Ploeg JM, Van Der Steen A, Rengerink KO, Van Der Vaart CH, Roovers JP (2014) Prolapse surgery with or without stress incontinence surgery for pelvic organ prolapse: a systematic review and meta-analysis of randomised trials. BJOG 121:537–547
Jha S, Cutner A, Moran P (2018) The UK National Prolapse Survey: 10 years on. Int Urogynecol J 22:517–528
Raman SV, Raker CA, Sung VW (2014) Concomitant apical prolapse repair and incontinence procedures: trends from 2001–2009 in the United States. Am J Obstet Gynecol 211:e1–e5
Jeffcoate TNA, Roberts H (1952) Stress incontinence of urine: opening papers. BJOG 59(5):685–697
Drutz HP, Shapiro BJ, Mandel F (1978) Do static cystourethrograms have a role in the investigation of female incontinence? Am J Obstet Gynecol 130(5):516–520
Green TH (1962) Development of a plan for the diagnosis and treatment of urinary stress incontinence. Am J Obstet Gynecol 83:632–648
Dietz HP, Hansell NK, Grace ME, Eldridge AM, Clarke B, Martin NG (2005) Bladder neck mobility is a heritable trait. BJOG 112:334–339
Chen B, Wen Y, Polan ML (2004) Elastolytic activity in women with stress urinary incontinence and pelvic organ prolapse. Neurourol Urodyn 23:119–126
Costantini E, Lazzeri M, Bini V, Del Zingaro M, Zucchi A, Porena M (2008) Burch colposuspension does not provide any additional benefit to pelvic organ prolapse repair in patients with urinary incontinence: a randomized surgical trial. J Urol 180:1007
Costantini E, Lazzeri M, Bini V, Del Zingaro M, Zucchi A, Porena M (2001) POP repair with and without prophylactic concomitant Burch colposuspension in continent women: a randomized, controlled trial with 8-year followup. J Urol 185(6):2236–2240
Brubaker L, Cundiff GW, Fine P, Nygaard I, Richter HE, Visco AG et al (2006) Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. N Engl J Med 354:1557–1566
Wei JT, Nygaard I, Richter HE, Nager CW (2012) A midurethral sling to reduce incontinence after vaginal prolapse repair. Obstet Gynecol Survey 366:2358–2367
van der Ploeg JM, Rengerink KO, van der Steen A, van Leeuwen JHS, van der Vaart CH, Roovers JPWR (2016) Vaginal prolapse repair with or without a midurethral sling in women with genital prolapse and occult stress urinary incontinence: a randomized trial. Int Urogynecol J 27(7):1029–1038
Borstad E, Abdelnoor M, Staff AC, Kulseng-Hanssen S (2010) Surgical strategies for women with pelvic organ prolapse and urinary stress incontinence. Int Urogynecol J 21(2):179–186
Lensen EJM, Withagen MIJ, Kluivers KB, Milani AL, Vierhout ME (2013) Urinary incontinence after surgery for pelvic organ prolapse. Neurourol Urodyn 32(5):455–459
Handa VL, Zyczynski HM, Brubaker L, Nygaard I, Janz NK, Richter HE et al (2007) Sexual function before and after sacrocolpopexy for pelvic organ prolapse. Am J Obstet Gynecol 197(6):e1–6
Perk H, Oral B, Yeşildağ A, Serel T, Özsoy M, Turgut T (2002) Magnetic resonance imaging for stress incontinence: evaluation of patients before and after surgical correction. Eur J Radiol 44(1):44–47
Ginath S, Garely AD, Luchs JS, Shahryarinejad A, Olivera CK, Zhou S et al (2012) Magnetic resonance imaging of abdominal versus vaginal prolapse surgery with mesh. Int Urogynecol J 23:1569–1576
Author information
Authors and Affiliations
Contributions
WM: project development, performing procedure, manuscript writing. ME: performing procedure, manuscript writing. S-AG: data collection, patient evaluation. AK: manuscript writing, project development. HH: performing procedure, project development.
Corresponding author
Ethics declarations
Conflict of interest
Wally Mahfouz, MD declares that he has no conflict of interest. Mostafa Elmissiry, MD declares that he has no conflict of interest. Saif-Alislam Gomaa, MD declares that he has no conflict of interest. Ashraf Koraitim, MD declares that he has no conflict of interest. Hebatallah H.M. Hassan, MD declares that she has no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee of Alexandria University, Egypt, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahfouz, W., Elmissiry, M., Gomaa, SA. et al. Evaluation of the effect of abdominal sacrocolpopexy (ASC) on urethral anatomy and continence mechanism using dynamic MRI. Int Urol Nephrol 52, 1429–1435 (2020). https://doi.org/10.1007/s11255-020-02444-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02444-8