Abstract
Purpose
Holmium laser enucleation of the prostate (HoLEP) represents the current standard procedure for size-independent surgical therapy of benign prostatic obstruction (BPO). With advent of the novel laser technology thulium fiber laser (TFL), we hypothesized that the functional outcome of TFL enucleation of the prostate (ThuFLEP) is non-inferior compared to HoLEP.
Methods
From October 2021 to October 2022, 150 patients with BPO were recruited for the prospective randomized trial in accordance with CONSORT. Stratified randomization into the arms ThuFLEP (n = 74) or HoLEP (n = 76) was carried out. The primary endpoint was non-inferior international prostate symptom score (IPSS) and quality of life (QoL) at three months after treatment. Secondary endpoints were rates of complications, peak flow, residual urine and operation times.
Results
Preoperative characteristics showed no significant differences. Overall IPSS and QoL improved from 21 to 8 and 4 to 1.5, respectively, after three months of follow-up. No statistically significant differences between ThuFLEP and HoLEP were observed regarding median postoperative IPSS (8.5 vs. 7, p > 0.9), QoL (1 vs. 2, p = 0.6), residual urine (48 vs. 30ml, p = 0.065) and peak flow (19 vs. 17ml/s, p > 0.9). Similarly, safety profile was comparable with no statistically significant differences regarding rate of major complications (5.3 vs. 5.4%, p = 0.5), laser hemostasis time (3 vs. 2min, p = 0.2), use of additive electric coagulation (74 vs. 87%, p = 0.06) or electric coagulation time (8 vs. 8min, p = 0.4).
Conclusions
In this prospective, randomized trial ThuFLEP showed non-inferior results compared to HoLEP in terms of functional outcomes measured by IPSS and QoL as primary endpoint.
Trial registration number
DRKS00032699 (18.09.2023, retrospectively registered).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Holmium laser enucleation of the prostate (HoLEP) has proven to be a safe and effective minimally invasive surgical treatment for bladder outlet obstruction (BOO) due to benign prostatic hyperplasia (BPH) [1, 2]. It can be performed regardless of size and with less morbidity as compared to transurethral resection of the prostate (TURP) and open simple prostatectomy, even in patients requiring anticoagulation [3,4,5].
With the thulium fiber laser (TFL), a novel energy source with different physical properties is available, which may have a positive impact on the safety profile of the LEP [6,7,8,9,10]. The wavelength of the TFL (1940nm) has a beneficial energy absorption maximum in water, which leads to a more shallow tissue penetration depth and reduced carbonization [11,12,13,14,15]. The TFL allows a wide variety of laser settings [11]. The potentially harmful effects are described as reduced while the hemostatic effect appears to be improved [11, 14, 16]. Due to less vaporization of the water between laser fiber and tissue TFL creates less bursting energy for tissue dissection and therefore has an improved cutting efficiency [11, 15].
In the studies available to date, the TFL enucleation of the prostate (ThuFLEP) has been shown to be equivalent to the HoLEP in terms of absolute operating time, enucleation and morcellation speed and functional results [10, 17,18,19,20]. However, most of the published evidence is of retrospective nature or based on small number of cases [8]. The only randomized prospective study, which was conducted by Enikeev et al. defined the severity of urinary incontinence according to the ICIQ-MLUTS as primary outcome [10]. There is still limited evidence on the use and clinical outcomes of ThuFLEP [8, 21, 22]. To fill this void, we conducted the following prospective randomized trial. Our goal is to verify that ThuFLEP is not inferior to HoLEP regarding functional outcomes, measured by IPSS and QoL three months after surgery. Urinary continence, objective voiding parameters, safety profile and efficiency represented secondary outcomes.
Material and methods
Data collection
This prospective randomized non-inferiority trial was performed at the University Hospital in Frankfurt after obtaining approval from the Institutional Ethics Committee (2021–171, approval No. E 98/21). We included all patients scheduled for LEP. Exclusion criteria were prostate volume measured by transrectal ultrasound (TRUS) of less than 30ccm, history of urethral stricture, preoperative evidence of prostate carcinoma or confirmed neurogenic bladder emptying disorder. From October 2021 to October 2022, 268 patients were planned for LEP, of whom 158 patients gave informed written consent.
Following strata were used for a stratified randomization into the two arms ThuFLEP and HoLEP: indwelling transurethral catheter vs. IPSS ≥ 20 vs. IPSS < 20, age < 70 years vs. age ≥ 70 years and prostate volume < 80ccm vs. ≥ 80ccm.
For ThuFLEP a Soltive™ SuperPulsed TFL (Olympus) with 550nm laser fiber (Olympus), 1.5J pulse energy and 40 Hz frequency setting was used. For HoLEP a high-power holmium laser (MOSES™ Pulse 120H, Boston Scientific) with 550nm laser fiber (Slim Line, Boston Scientific), 1.4J pulse energy and 50 Hz frequency setting was used. MOSES™ pulse modulation was deactivated. Enucleation efficiency was defined as enucleation weight per enucleation time. Postoperative complications were recorded according to the Clavien-Dindo (CLD) classification system [23]. Five surgeons (2 high-volume surgeons: mean experience 592 cases, 3 low-volume surgeons: mean experience 57 cases) were assigned randomly to both treatment groups according to personal availabilities.
PROMs (patient reported outcome measures) were collected preoperatively and three months postoperatively including standardized validated questionnaires: international prostate symptom score (IPSS), quality of life (QoL) and international consultation of incontinence questionnaire short form (ICIQ-SF). Pre- and postoperative continence was defined as ICIQ-SF ≤ 4 or usage of at most one security pad per day.
Statistical analysis
Based on an assumed standard deviation regarding IPSS reduction at three months of 4 points, a non-inferiority margin of 2 points (half the standard deviation) was determined for the sample size calculation. Totally 128 patients should be included for the analysis of the study for an 80% statistical power with the upper limit of a one-sided 95% confidence interval exceeding a > 5% difference in favor of the standard treatment group. Considering a drop-off rate of 15%, 152 study participants should be randomized per minimum.
Multivariable regression models tested the effect of the laser technology on the target criterions mentioned above. In all statistical analyses, R software environment for statistical computing (version 3.6.1) was used. The level of significance was set at p < 0.05.
Results
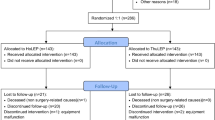
158 patients consented to be enrolled in the study, in one case an intraoperative urethral stricture was found, four patients were lost to follow-up and in three cases a randomization error occurred. These eight patients were excluded from data analysis.
Descriptive characteristics of the study population
Finally, data from 150 patients could be included for the analysis, so that the initial sample size calculation of a minimum of 128 patients was met (Fig. 1). 74 (49%) received ThuFLEP and 76 (51%) received HoLEP. The mean age was 69 years. The mean prostate volume was 80ccm. All preoperative characteristics did not show significant differences (p > 0.05, Table 1).
Functional outcomes
The three-month follow-up showed an improvement of overall IPSS and QoL from 21 preoperatively to 8 and from 4 to 1.5 points. No statistically significant differences between ThuFLEP and HoLEP were observed regarding the primary endpoints median postoperative IPSS (8.5 vs. 7, p > 0.9) and QoL (1 vs. 2, p = 0.6). The preoperative mean peak flow (Qmax) of 9.3ml/s and post voiding residual urine (PVR) of 100 ml improved to 18ml/s and PVR of 39ml after surgery. No statistically significant differences regarding postoperative Qmax (19 vs. 17ml/s, p > 0.9) and PVR (48 vs. 30ml, p = 0.065) were observed between the two treatment groups. Regarding urinary incontinence, only 74% of the patients were continent preoperatively vs. 82% at 3 months after the operation and the mean ICIQ-SF was 5 vs. 4 points before and after the operation. Three months after surgery, 2% of the patients still were supplied with an indwelling catheter vs. 24% preoperatively. No statistically significant differences between ThuFLEP and HoLEP were observed regarding rates of continence (79 vs. 85%, p = 0.3), ICIQ-SF (4 vs. 4 points, p > 0.9) and rates of indwelling catheter (8.1 vs. 3.9%, p = 0.3).
Perioperative efficacy and safety outcomes
Overall operation time (58 vs. 56min, p = 0.12) and morcellation time (7 vs. 8min, p = 0.13) showed no significant differences between ThuFLEP and HoLEP. However, HoLEP showed a significantly faster enucleation time of 27min and higher enucleation efficiency of 2.03g/min than ThuFLEP with 36min (p = 0.02) and 1.45g/min (p = 0.001). There were no significant differences regarding minor (15 vs. 7.9%, p = 0.5) or major (5.4 vs. 5.3%, p = 0.5) complication rates in ThuFLEP vs. HoLEP. Furthermore, there were no significant differences regarding laser hemostasis time (2 vs. 3min, p = 0.2), the use of additive electric coagulation (87 vs. 74%, p = 0.06) or electric coagulation time (8 vs. 8min, p = 0.4). Regarding possible learning curve effects using the novel laser source, we examined the second half of each surgeon's ThuFLEP cases as a subgroup comparison. HoLEP also showed a significantly faster enucleation time (27 vs. 37min, p = 0.04) and faster enucleation efficiency (2.03 vs. 1.13min/g, p < 0.001) compared to these last ThuFLEP cases (supplementary table).
Multivariable regression models
Multivariable linear regression models were fitted to predict enucleation time according to the laser source adjusted for enucleation weight, age, surgeon’s caseload, ASA (American Society of Anesthesiologists) risk status and occurrence of complications. The use of the TFL resulted in a significant increase in enucleation time (OR 1.41, p < 0.001). Furthermore, also the surgeon’s caseload (OR 0.53, p < 0.001) and the enucleation weight (OR 1.01, p < 0.001) were significant predictors of prolonged enucleation time (Table 2). Multivariable logistic regression models were fitted to predict major complications according to the laser source adjusted for age, operation time and enucleation weight. The laser source was not a significant predictor of complications (supplementary table).
Discussion
There is still limited evidence on the use and clinical outcomes of ThuFLEP. To fill this void, we conducted the following prospective randomized trial and made several important observations.
First, our study’s primary outcome revealed no significant differences in functional outcomes measured by IPSS and QoL between HoLEP and ThuFLEP. Possible differences were suspected in theoretical tissue penetration depth, carbonization effects and heat development due to different energy absorption maxima of the two lasers in water tissue [11, 15]. However, in our study the subjective questionnaire scores and objective functional assessment did not differ between the two groups at 3 months of follow-up. This finding is in line with the exploratory analyses of the randomized prospective study by Enikeev et al. and the review of Pang et al. [10, 24].
Second, we found no differences in safety outcomes. Discussions about possible safety differences between TFL and holmium laser arose from the same reasons as mentioned above regarding functional outcomes [11]. The first ex vivo trials showed significant differences between the laser sources with improved hemostatic effect [11, 14, 16]. On the contrary, one ex vivo trial showed comparable coagulation between the two laser sources and another ex vivo trial even postulated a significant better coagulation with the holmium laser than with TFL [25, 26]. A systemic review of experimental studies postulated similar temperature changes caused by TFL and holmium laser [15]. Taken together, the ex vivo data are inhomogeneous. Our study observed no difference in all investigated hemostasis parameters, such as hemostasis time, additional use of electric coagulation for hemostasis or complications. This finding is supported by previous clinical studies investigating the safety of ThuFLEP [10, 17, 19, 24]. Only one publication comparing the TFL with holmium laser using MOSES™ 2.0 with BPH mode described significantly longer hemostasis time for TFL while the hemoglobin drop was not significantly different [20]. It is unclear to what extent the MOSES™ technology influenced this comparison [27].
Third, we found a higher enucleation efficiency in HoLEP cases compared to ThuFLEP cases in exploratory analyses. A possible explanation for this significant speed difference might be due to the laser characteristics. Tissue rupturing due to fast vaporization of the water between laser fiber and tissue as it is typical for the holmium laser may achieve better tissue separation than a sharp incision which is typical for the TFL [11]. In two ex vivo trials the tissue separation depth was greater with the holmium laser than TFL and objectively preferred by the surgeons [16, 25]. In three in vivo studies available to date, ThuFLEP was equivalent to HoLEP in terms of enucleation time and efficiency [10, 12, 18]. Only one trial described a better enucleation efficiency for HoLEP using MOSES™ 2.0 with BPH mode compared to ThuFLEP [20]. To what extent the MOSES™ technology could have influenced the comparison here is part of future research. However, our study showed no significant differences regarding overall operation time and morcellation time. This finding is supported by all previous data and the review of Taratkin et al. [10, 18, 19, 22]. Although the TFL was a relatively new laser source for our surgeons, who were all used to the holmium laser, our reported ThuFLEP enucleation efficiency of 1.45g/min is still higher than achieved in other publications (1.04 to 1.40g/min) [8, 10, 13, 17, 19, 20, 28]. This suggests that ThuFLEP has already been performed efficient and concerns about the learning curve can be put into perspective [12, 29].
Taken together, the results confirm that ThuFLEP is not inferior to HoLEP regarding functional outcomes, measured by IPSS and QoL 3 months after surgery.
Limitations
This study was designed to provide best evidence regarding the non-inferiority of ThuFLEP vs. HoLEP. Nevertheless, also a prospective randomized trial is not devoid of limitations. The follow-up of the micturition symptoms was assessed without additional objective assessment of the voiding situation except at discharge. Thus, we cannot provide objective measurements such as Qmax and PVR for the follow-up time. However, the main target criterion of the study was to assess the subjective micturition performance and its related quality of life and there is evidence that the collection of PROMs can measure differences in subjective effects of health care interventions best [30]. All other analyses were just exploratory evaluations. Thus, conclusions drawn from our exploratory analysis regarding the operation times should bare this in mind. Electric coagulation was applied at the discretion of the surgeon at a relatively high rate, but it did not differ according to high- vs low-volume surgeons and was comparable within the two treatment groups. Moreover, the personal experience of each surgeon could influence the operation times and outcomes. However, we avoided assessing single surgeons’ outcomes and evaluated pooled results from five LEP surgeons, which allows to assess the operation technique as a whole. In addition, the proportion of experienced surgeons was distributed equally between the two treatment groups. Furthermore, late complications as bladder neck contracture and urethral stricture could not be evaluated as the current study focused on short-term functional outcomes and was not designed to estimate late complications. Finally, our prospective database may be influenced by a negative selection bias regarding the admittance of patients with a particularly high perioperative risk to our tertiary care university center. Nevertheless, the preoperative characteristics of our patients sampled a typical LEP collective [24]. Moreover, we included all consenting patients planned for LEP at our institution to allow most comprehensive analyses. This trial was conducted without professional study support and designed and carried out by clinical urologists.
Conclusion
In this prospective, randomized study ThuFLEP is not inferior to HoLEP in terms of functional outcomes. In addition, a comparable safety profile and similar overall operation time was shown. Both ThuFLEP and HoLEP are effective and safe ways of treating benign prostatic obstruction.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Gild P, Lenke L, Pompe RS et al (2021) Assessing the Outcome of Holmium Laser Enucleation of the Prostate by Age, Prostate Volume, and a History of Blood Thinning Agents: Report from a Single-Center Series of >1800 Consecutive Cases. J Endourol 35:639–646
Higazy A, Tawfeek AM, Abdalla HM et al (2021) Holmium laser enucleation of the prostate versus bipolar transurethral enucleation of the prostate in management of benign prostatic hyperplasia: A randomized controlled trial. Int J Urol 28:333–338
Li M, Qiu J, Hou Q et al (2015) Endoscopic enucleation versus open prostatectomy for treating large benign prostatic hyperplasia: a meta-analysis of randomized controlled trials. PLoS ONE 10:e0121265
Deuker M, Rührup J, Karakiewicz PI et al (2021) Holmium laser enucleation of the prostate: efficacy, safety and preoperative management in patients presenting with anticoagulation therapy. World J Urol 39:1219–1226
Sun J, Shi A, Tong Z et al (2018) Safety and feasibility study of holmium laser enucleation of the prostate (HOLEP) on patients receiving dual antiplatelet therapy (DAPT). World J Urol 36:271–276
Kronenberg P, Traxer O (2019) The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol 8:S398-s417
Enikeev D, Shariat SF, Taratkin M et al (2020) The changing role of lasers in urologic surgery. Curr Opin Urol 30:24–29
Rice P, Somani BK (2021) A Systematic Review of Thulium Fiber Laser: Applications and Advantages of Laser Technology in the Field of Urology. Res Rep Urol 13:519–527
Herrmann TRW, Becker B, Netsch C (2023) Thulium YAG is the Best Laser for the Prostate Because of Versatility. Eur Urol Open Sci 48:18–21
Enikeev D, Taratkin M, Babaevskaya D et al (2022) Randomized prospective trial of the severity of irritative symptoms after HoLEP vs ThuFLEP. World J Urol 40:2047–2053
Fried NM, Murray KE (2005) High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol 19:25–31
Enikeev D, Glybochko P, Rapoport L et al (2018) A Randomized Trial Comparing The Learning Curve of 3 Endoscopic Enucleation Techniques (HoLEP, ThuFLEP, and MEP) for BPH Using Mentoring Approach-Initial Results. Urology 121:51–57
Enikeev D, Netsch C, Rapoport L et al (2019) Novel thulium fiber laser for endoscopic enucleation of the prostate: A prospective comparison with conventional transurethral resection of the prostate. Int J Urol 26:1138–1143
Taratkin M, Kovalenko A, Laukhtina E et al (2022) Ex vivo study of Ho:YAG and thulium fiber lasers for soft tissue surgery: which laser for which case? Lasers Med Sci 37:149–154
Ortner G, Rice P, Nagele U et al (2023) Tissue thermal effect during lithotripsy and tissue ablation in endourology: a systematic review of experimental studies comparing Holmium and Thulium lasers. World J Urol 41:1–12
Yilmaz M, Esser J, Kraft L et al (2022) Experimental ex-vivo performance study comparing a novel, pulsed thulium solid-state laser, chopped thulium fibre laser, low and high-power holmium:YAG laser for endoscopic enucleation of the prostate. World J Urol 40:601–606
Petov V, Babaevskaya D, Taratkin M et al (2022) Thulium Fiber Laser Enucleation of the Prostate: Prospective Study of Mid- and Long-Term Outcomes in 1328 Patients. J Endourol 36:1231–1236
Enikeev D, Taratkin M, Laukhtina E et al (2019) En bloc and two-lobe techniques for laser endoscopic enucleation of the prostate: retrospective comparative analysis of peri- and postoperative outcomes. Int Urol Nephrol 51:1969–1974
Morozov A, Taratkin M, Kozlov V et al (2020) Retrospective Assessment of Endoscopic Enucleation of Prostate Complications: A Single-Center Experience of More Than 1400 Patients. J Endourol 34:192–197
Elmansy H, Hodhod A, Elshafei A et al (2022) Comparative analysis of MOSES(TM) technology versus novel thulium fiber laser (TFL) for transurethral enucleation of the prostate: A single-institutional study. Arch Ital Urol Androl 94:180–185
Enikeev D, Taratkin M (2023) Thulium Fiber Laser: Bringing Lasers to a Whole New Level. Eur Urol Open Sci 48:31–33
Taratkin M, Checcucci E, Androsov A et al (2022) Thulium fiber laser in BPH surgery: Bench to bedside - a systematic review on behalf of YAU Urotechnology Working Group. Front Urol 2:1017069
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Pang KH, Ortner G, Yuan Y et al (2022) Complications and functional outcomes of endoscopic enucleation of the prostate: a systematic review and meta-analysis of randomised-controlled studies. Cent European J Urol 75:357–386
Doizi S, Germain T, Panthier F et al (2022) Comparison of Holmium:YAG and Thulium Fiber Lasers on Soft Tissue: An Ex Vivo Study. J Endourol 36:251–258
Taratkin M, Netsch C, Enikeev D et al (2021) The impact of the laser fiber-tissue distance on histological parameters in a porcine kidney model. World J Urol 39:1607–1612
Corsini C, de Angelis M, Villa L et al (2022) Holmium: yttrium-aluminum-garnet laser with Moses: does it make a difference? Curr Opin Urol 32:324–329
Enikeev D, Okhunov Z, Rapoport L et al (2019) Novel Thulium Fiber Laser for Enucleation of Prostate: A Retrospective Comparison with Open Simple Prostatectomy. J Endourol 33:16–21
Kosiba M, Hoeh B, Welte MN et al (2022) Learning curve and functional outcomes after laser enucleation of the prostate for benign prostate hyperplasia according to surgeon’s caseload. World J Urol 40:3007–3013
Agarwal A, Pain T, Levesque JF et al (2022) Patient-reported outcome measures (PROMs) to guide clinical care: recommendations and challenges. Med J Aust 216:9–11
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for conducting this study. Marina Kosiba, Andreas Becker and Felix K.-H. Chun are proctors for Olympus and Boston Scientific.
Author information
Authors and Affiliations
Contributions
MK: manuscript writing, protocol development, project development, data management, data analysis. MF: manuscript writing, project development. MN.W: protocol development, data management. LH: data collection. AC.K: data collection. MI.T: manuscript editing. MJ.M: manuscript editing. LA.K: manuscript editing. PC.M: manuscript editing. FK.-H.C: manuscript editing. AB: protocol development, project development, manuscript editing. All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MK, MN.W, LH and AC.K. The first draft of the manuscript was written by MF and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kosiba, M., Filzmayer, M., Welte, M.N. et al. Thulium fiber laser vs. holmium laser enucleation of the prostate: results of a prospective randomized non-inferiority trial. World J Urol 42, 49 (2024). https://doi.org/10.1007/s00345-023-04748-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-023-04748-7