Abstract
Purpose
To evaluate the impact of surgical caseload on safety, efficacy, and functional outcomes of laser enucleation of the prostate (LEP) applying a structured mentoring program.
Methods
Patient characteristics, perioperative data, and functional outcomes were analyzed descriptively. Linear and logistic regression models analyzed the effect of caseload on complications, functional outcomes and operative speed. Within the structured mentoring program a senior surgeon was present for the first 24 procedures completely, for partial steps in procedures 25–49, and as needed thereafter.
Results
A total of 677 patients from our prospective institutional database (2017–2022) were included for analysis. Of these, 84 (12%), 75 (11%), 82 (12%), 106 (16%), and 330 patients (49%) were operated by surgeons at (A) < 25, (B) 25–49, (C) 50–99, (D) 100–199, and (E) ≥ 200 procedures. Preoperative characteristics were balanced (all p > 0.05) except for prostate volume, which increased with caseload.
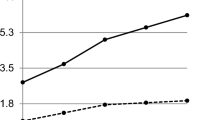
There was no significant difference in change of IPSS, Quality of life, ICIQ, pad usage, peak urine flow, residual urine, and major complications (Group A: 8.3 to E: 7.6%, p = 0.2) depending on the caseload. Caseload was not associated (Odds ratio: 0.7–1.4, p > 0.2) with major complications in the multivariable logistic regression model. Only operating time was significantly shorter with increasing caseload in the multivariable analysis (111–55 min, beta 23.9–62.9, p < 0.001).
Conclusion
With a structured mentoring program, the safety and efficacy of LEP can be ensured even during the learning curve with very good outcome quality. Only the operating time decreases significantly with increasing experience of the surgeon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laser enucleation of the prostate (LEP) has proven to be a safe and effective minimally invasive surgical treatment for bladder outlet obstruction (BOO) due to benign prostate hyperplasia (BPH) or prostate cancer (PCa) [1, 2]. Unlike transurethral resection of the prostate (TURP), it can be performed regardless of size and with less morbidity as compared to TUR-P and open simple prostatectomy [3, 4], even in patients requiring anticoagulation [5]. Although multiple enucleation techniques, using various energy sources, have been described over the past few years [6, 7], HoLEP remains the only size-independent option validated in randomized controlled trials [8, 9] and supported by level-1 evidence [10, 11]. As such HoLEP is recommended by European Association of Urology (EAU) and American Urology Association (AUA) guidelines [12, 13] and has become the gold standard for the surgical treatment of lower urinary tract symptoms due to BOO [11, 14, 15]. Despite its scientific status, diffusion into clinical practice is limited and classical TURP remains the predominant surgical BOO procedure by far [16]. An allegedly flat learning curve is regarded as main barrier against widespread clinical acceptance [17,18,19,20,21,22]. However, more recently, a growing number of mentoring programs have been introduced, aiming to accelerate the learning curve [9, 22]. Especially one recent review [9] suggested that around 50 procedures might be sufficient to achieve a stable outcome, which could be reduced to about 25 in the case of structured training. We herein evaluated the learning curve of four novel LEP surgeons with regard to functional outcomes and complications. We postulated that applying a structured LEP mentoring program, stable functional outcomes and low complication rates can be achieved independent of the surgical caseload.
Materials and methods
Study population
Within our prospectively maintained, institutional database, all consecutive patients who underwent LEP for BPH between November 2017 and January 2022 were identified. Patients with preoperative urethral strictures or previously known PCa were excluded (n = 77). Procedures were performed by two senior LEP experts with experience of > 100 procedures (A.B., F.K.H.C.), as well as by four additional surgeons who learned LEP progressively using the structured mentoring program. A senior surgeon was present for the first 24 procedures completely, for partial steps in procedures 25–49, and as a second surgeon when needed after the 50th procedure. Patients were retrospectively stratified into five groups (A: 1–24, B: 25–49, C: 50–99, D: 100–199, E: ≥ 200 cases) depending on the operating surgeon’s caseload. Our mentoring program starts after observation of 10 procedures conducted by expert surgeons (OR observation or video) and is based on the curriculum displayed in Fig. 1.
Structured mentoring program for laser enucleation of the prostate developed at University Hospital Frankfurt. In dependence of the novice surgeon's caseload, the appropriate prostate size, surgical steps and presence of a senior surgeon are determined. The mentoring program starts after observation of 10 full procedures conducted by expert surgeons (OR observation or video)
Surgical procedure
All surgical procedures were performed with the Olympus, OES Pro Laser Resectoscope, a high power (120 W) holmium laser generator (MOSES Pulse 120H, Lumenis) with a 550 nm laser fiber (Lumenis, Slim Line), or the Soltive™ SuperPulsed laser generator (Olympus) with a 550 nm laser fiber. For morcellation the PIRANHA morcellator by Richard Wolf or the Versacut morcellator by Lumenis was used.
Follow-up
Standardized questionnaires (International Prostate Symptoms Score (IPSS), Quality of life (Qol), International Consultation on Incontinence Questionnaire (ICIQ), and pad usage) were assessed preoperatively and at 4 weeks, 3 months, and then yearly and delta (Δ) was calculated by subtracting postoperative from preoperative values. A pad usage of more than one security pad was defined as incontinent. Before surgery and at dismission, peak urine flow and residual urine was registered. Postoperative complications were recorded according to the Clavien−Dindo (CLD) classification system using a graduation from CLD I to CLD V [23]. Major complications were defined as CLD equal or greater IIIb [24]. Intraoperative complications were defined as any complication occurring during the procedure as f.ex capsular perforation or bladder injury.
Statistical analysis
Descriptive statistics included frequencies and proportions for categorical variables. Means, medians, and interquartile-ranges (IR) were reported for continuously coded variables. The Chi-square test was used to assess the statistical significance in proportions’ differences. The t test and Kruskal−Wallis test examined the statistical significance of means’ and medians’ differences. Multivariable linear and logistic regression models were fit to analyze the effect of caseload on complications, functional outcomes, and OR speed. Covariates were age, prostate size, incidental PCa, American Society of Anesthesiologists (ASA) status and intraoperative complications.
In all statistical analyses, R software environment for statistical computing and graphics (version 3.6.1) was used. All tests were two-sided with a level of significance set at p < 0.05. Ethical approval was obtained from the local ethics committee at the University Hospital Frankfurt. All included patients gave informed written consent.
Results
In our institutional database, we identified 677 eligible patients who underwent LEP at the University Hospital Frankfurt from November 2017 to January 2022. Of these, 84 (12%), 75 (11%), 82 (12%), 106 (16%), and 330 patients (49%) were operated by surgeons at A: < 25, B: 25–49, C: 50–99, D: 100–199, and E: ≥ 200 procedures.
Descriptive characteristics of the study population
Preoperative characteristics were balanced (Table 1) except for prostate volume, which increased significantly with increasing caseload (prostate volume in transrectal ultrasound (TRUS) 67 (group A) to 80ccm (group E), p = 0.009). Overall 215 (35%) patients had an indwelling catheter before the surgery and 344 (74%) were continent, defined as usage of equal or less than one pad or ICIQ ≤ 4 ( the lowest amount over 0 in each ICIQ question). ASA score was predominantly low (452 patients (67%) had ASA I or II. After surgery an irrigation foley catheter was left for median 2 days, without significant differences among caseload groups. Operating room (OR) time was significantly reduced with increasing caseload, ranging from 111 min [Interquartile range (IQR): 91, 140 min] in group A to 55 min in group E (IQR 43, 76 min) (p < 0.001), while enucleated prostate volume increased from 54 g in group A to 58 g in group E, p = 0.03.
Postoperative outcomes
There was no significant difference between caseload groups with regard to follow up measures (Table 2). International Prostate Symptoms Score (IPSS) was reduced by median 11 (IQR 5–17) points as compared to preoperatively. The quality of life (Qol) was improved by median 3 (IQR 1–4) points. The median ICIQ score or pad consumption did not change significantly as compared to preoperatively. Peak urine flow was increased by median 9 ml/s (IQR 3–16 ml/s) and residual urine was reduced by median 60 ml (IQR 15-150 ml). Major complications were not recorded significantly more often at the beginning of the learning curve than in more experienced levels (group A: 8.3% vs group E: 7.6%, p = 0.2). Indwelling transurethral catheter was reduced from preoperative overall 210 (35%) patients to 25 (3.8%) at dismission, without significant differences according to caseload. Finally, 443 patients (95% (A: 91% to E: 97%, p = 0.2) were continent at last follow up (Table 2, rates over time shown in Supplemental Fig. 3).
Multivariable linear regression
OR time and isolated enucleation time was univariably plotted according to surgeon’s caseload (Supplemental Fig. 2). A multivariable linear regression model was fitted to predict OR time according to surgeon’s caseload (Supplemental Table 3). Covariates consisted of TRUS prostate volume, age, ASA status, intraoperative complications and incidental prostate carcinoma. Caseload showed a highly significant and consistent decrease in OR time with every increment of experience (beta 62.86 to 23.92 min, all p < 0.01). Intraoperative complications (beta 14.37 min) and TRUS prostate volume (beta 0.48) were significant predictors for increasing OR time (all p < 0.01).
Multivariable logistic regression
Multivariable logistic regression model was fitted to predict major complications according to surgeon’s caseload, adjusted for TRUS prostate volume, age, ASA status, and incidental prostate carcinoma (Supplemental Table 4). Caseload was not a significant predictor of complications, regardless of its increment. However, Prostate size (OR 1.01), and high ASA status (OR 2.29) were significant predictors for major complications (all p < / = 0.01). Diagnosis of incidental prostate carcinoma (OR 1.9) as predictor of major complications did not reach statistical significance (p = 0.09).
Discussion
We reported our institutional experience regarding safety and efficacy of LEP with regard to surgeon’s caseload. Our analyses yielded several important observations.
First, we reported a large series of nearly 700 patients, which is one of the biggest cohorts published concerning learning curve analyses [17,18,19]. Moreover, our report does not represent a single surgeon´s experience but pooled results from four beginner surgeons, which make our results very robust and less susceptible to individual abilities and, as such, more generalizable.
Second, we found a highly significant and consistent decrease in OR time depending on surgeons’ caseload. This finding is plausible and consistent with virtually all previous reports that also confirmed a more time efficient procedure with growing experience. Brunckhorst et al. [12] reported a retrospective analysis of 253 consecutive cases of a single HoLEP surgeon. Consistent with our results, they found that enucleation speed was significantly increasing throughout the beginning of the learning curve, however, they found a plateau after 50–60 cases which is in contrast to our results, where we saw ongoing improvements in OR time until > 200 cases.
Third, we found excellent and stable functional outcomes independent of the surgeon’s caseload. This is in contrast to most of the other studies as highlighted in a systematic review by Kampantais et al. [9], which included 24 studies with a total of 5173 patients. They found ongoing improvements in functional outcomes until a plateau was reached after approximating 25–50 cases. This is in contrast to our findings, where we found stable functional outcomes for novices trained within our structured mentoring program independent of their caseload. However, the authors also concluded that a structured mentorship program would aid for faster progress, which might explain our better results.
Fourth, we evaluated major complication rates according to caseload and found no significant association between caseload and occurrence of major complications. Interestingly, the majority of publications report on functional outcomes or OR time. Only a minority of studies also reported on complications, when assessing the learning curve. This is worrisome as a low complication rate should be the utmost goal for every intervention, especially for a surgery, which is conducted for a benign disease. Rosenhammer et al. [25] found that ASA status and prostate cancer were independent predictors for grade ≥ 2 complications but not the caseload, which is consistent with our results, where we also found ASA status and prostate volume, but not caseload, as significant predictor of major complications. Moreover, Westhofen et al. [22] found the overall incidence of treatment-related adverse events was significantly higher without a training program. Conversely, Lerner et al. [19] showed a strong correlation between complication rates and learning curve in their study, especially when time between consecutive cases was more than 5 weeks. We did not evaluate the time in between the consecutive cases of the surgeons in our analysis, so we cannot compare these results. However, it appears logical especially without a structured mentoring program that already learned skills will diminish when time is too long in between two cases. Similarly, the institutional caseload seems important in this regard, as beside personal frequency of interventions, a high level of competence of the team in dealing with the intervention ensures high quality surgical outcomes [26].
Fifth, we applied Trifecta and Pentafecta criteria as defined by Robert et al. [21] to our results. These criteria of a perfect procedure consist of the combination of complete enucleation and morcellation within less than 90 min and without any conversion to standard TURP (Trifecta). In addition, information on complications or occurrence of stress urinary incontinence in 3 months after the operation are added for the Pentafecta criteria. Applying these criteria to our results, we achieved the Trifecta criteria mainly by reaching the expected OR time of less than 90 min after more than 50 cases, as we never used conversion to TUR-P. Similarly, the Pentafecta criteria were reached at 50 cases due to OR time because of consistently low rates of complications and urinary incontinence. This is comparable to the report by Peyronnet et al. [20] who met the criteria in four consecutive patients after the 40th procedure in the HoLEP group.
Taken together, we reported on a large series of nearly 700 patients with pooled results from four beginner surgeons, which make our results very robust and pertinent. We found a highly statistically significant improvement in OR time according to surgeon’s caseload. This is in accordance to virtually all other reports. However, we found stable functional outcomes and stable low complications rates, independent from the surgeon’s caseload. This is in contrast to many other studies that report an improvement of these variables according to the surgeon’s caseload. Apparently, a structured mentoring program over the first 50 cases, which was applied in our institution can help overcome the learning curve.
Several limitations apply to our study. Although the database is designed prospectively, the analysis of the learning curve is retrospective and thus selection biases may occur. Low number of cases in each caseload group limited depth of subgroup analyses. Furthermore, our prospective database may be influenced by a negative selection bias regarding the admittance of patients with a particularly high perioperative risk to our tertiary care university center. Nevertheless, we included all LEP patients since its implementation at our institution to allow most comprehensive analyses.
Conclusion
With a structured mentoring program, the safety and efficacy of LEP can be ensured even during the learning curve with excellent functional outcomes. Only the OR time decreases significantly with increasing experience of the surgeon.
Availability of data and material
The data are available for requests.
Code availability
Not applicable.
References
Becker A, Placke A, Kluth L, Schwarz R, Isbarn H, Chun F et al (2014) Holmium laser enucleation of the prostate is safe in patients with prostate cancer and lower urinary tract symptoms–a retrospective feasibility study. J Endourol 28(3):335–341
Gild P, Lenke L, Pompe RS, Vetterlein MW, Ludwig TA, Soave A et al (2021) Assessing the outcome of holmium laser enucleation of the prostate by age, prostate volume, and a history of blood thinning agents: report from a single-center series of >1800 consecutive cases. J Endourol 35(5):639–646
Kuntz RM, Ahyai S, Lehrich K, Fayad A (2004) Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol 172(3):1012–1016
Kuntz RM, Lehrich K, Ahyai S (2004) Transurethral holmium laser enucleation of the prostate compared with transvesical open prostatectomy: 18-month follow-up of a randomized trial. J Endourol 18(2):189–191
Deuker M, Rührup J, Karakiewicz PI, Welte M, Kluth LA, Banek S et al (2021) Holmium laser enucleation of the prostate: efficacy, safety and preoperative management in patients presenting with anticoagulation therapy. World J Urol 39(4):1219–1226
Kahokehr A, Gilling PJ (2014) Enucleation techniques for benign prostate obstruction: which one and why? Curr Opin Urol 24(1):49–55
Lerner LB, Rajender A (2015) Laser prostate enucleation techniques. Can J Urol 22(Suppl 1):53–59
Enikeev D, Morozov A, Taratkin M, Misrai V, Rijo E, Podoinitsin A et al (2021) Systematic review of the endoscopic enucleation of the prostate learning curve. World J Urol 39(7):2427–2438
Kampantais S, Dimopoulos P, Tasleem A, Acher P, Gordon K, Young A (2018) Assessing the learning curve of holmium laser enucleation of prostate (HoLEP). A systematic review. Urology 120:9–22
Ahyai SA, Lehrich K, Kuntz RM (2007) Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol 52(5):1456–1463
Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C et al (2015) EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 67(6):1099–1109
EAU (2022) European Association of Urology Guidelines. In: Edition presented at the EAU Annual Congress Amsterdam. (EAU Guidelines Office, Arnhem, the Netherlands)
Lerner LB, McVary K, Barry MJ (2021) Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA Guideline part II, surgical evaluation and treatment. J Urol 206:818
Michalak J, Tzou D, Funk J (2015) HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century. Am J Clin Exp Urol 3(1):36–42
Vincent MW, Gilling PJ (2015) HoLEP has come of age. World J Urol 33(4):487–493
Uhlig A, Baunacke M, Groeben C, Borkowetz A, Volkmer B, Ahyai SA et al (2022) Die operative Therapie des benignen Prostatasyndroms in Deutschland. Der Urologe.
Brunckhorst O, Ahmed K, Nehikhare O, Marra G, Challacombe B, Popert R (2015) Evaluation of the learning curve for holmium laser enucleation of the prostate using multiple outcome measures. Urology 86(4):824–829
Kim KH, Yang HJ, Heo NH, Kim SH, Kim DS, Lee CH et al (2021) Comparison study of learning curve using cumulative sum analysis between holmium laser enucleation of the prostate and transurethral resection of the prostate: is holmium laser enucleation of the prostate a difficult procedure for beginner urologists? J Endourol 35(2):159–164
Lerner LB (2010) Stress incontinence during the learning curve of holmium laser enucleation of the prostate. J Endourol 24(10):1655–1658
Peyronnet B, Robert G, Comat V, Rouprêt M, Gomez-Sancha F, Cornu J-N et al (2017) Learning curves and perioperative outcomes after endoscopic enucleation of the prostate: a comparison between green light 532-nm and holmium lasers. World J Urol 35(6):973–983
Robert G, Cornu JN, Fourmarier M, Saussine C, Descazeaud A, Azzouzi AR et al (2016) Multicentre prospective evaluation of the learning curve of holmium laser enucleation of the prostate (HoLEP). BJU Int 117(3):495–499
Westhofen T, Weinhold P, Kolb M, Stief CG, Magistro G (2020) Evaluation of holmium laser enucleation of the prostate learning curves with and without a structured training programme. Curr Urol 14(4):191–199
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Mitropoulos D, Artibani W, Biyani CS, Bjerggaard Jensen J, Roupret M, Truss M (2018) Validation of the Clavien–Dindo grading system in urology by the European Association of Urology guidelines Ad Hoc panel. Eur Urol Focus 4(4):608–613
Rosenhammer B, Schönhärl M, Mayr R, Schnabel MJ, Burger M, Eichelberg C (2020) Introduction of a new score to assess surgical efficiency in holmium laser enucleation of the prostate. Urol Int 104(11–12):914–922
Van den Broeck T, Oprea-Lager D, Moris L, Kailavasan M, Briers E, Cornford P et al (2021) A systematic review of the impact of surgeon and hospital caseload volume on oncological and nononcological outcomes after radical prostatectomy for nonmetastatic prostate cancer. Eur Urol 80(5):531–545
Funding
Open Access funding enabled and organized by Projekt DEAL. We did not receive any funding for our work.
Author information
Authors and Affiliations
Contributions
MK: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing. BH: Data analysis, Manuscript editing. MW: Data collection or management, Manuscript editing. KMJ: Manuscript editing. KV: Data collection or management. NL: Data collection or management. J Schröder: Data collection or management. JL: Data collection or management. SFE: Data collection or management. AH: Data collection or management. FCR: Manuscript editing. LAK: Manuscript editing. PM: Manuscript editing. FKHC: Manuscript editing. AB: Protocol/project development, Data collection or management, Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Our research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The authors report no conflict of interest.
Ethical approval
Ethical approval was obtained from the local ethics committee at the University Hospital of Frankfurt.
Informed consent
All included patients gave informed written consent.
Research involving human participants and/or animals
Our Research involved Human participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kosiba, M., Hoeh, B., Welte, M.N. et al. Learning curve and functional outcomes after laser enucleation of the prostate for benign prostate hyperplasia according to surgeon’s caseload. World J Urol 40, 3007–3013 (2022). https://doi.org/10.1007/s00345-022-04177-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04177-y