Abstract
Introduction
Holmium:yttrium–aluminium–garnet (Ho:YAG) and thulium fiber (TFL) lasers are currently the two laser sources recommended for endocorporeal laser lithotripsy (ELL). Recently, the pulsed-thulium:YAG (Tm:YAG) laser was also proposed for ELL, as an answer to both Ho:YAG and TFL limitations. We aimed to evaluate the efficiency, safety, and laser settings of Tm:YAG laser in ELL during retrograde intrarenal surgery (RIRS).
Methods
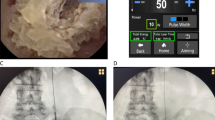
A prospective study of the first 25 patients with ureteral and renal stones who underwent RIRS using the Thulio (pulsed-Tm:YAG, Dornier©, Germany) was performed in a single center. 272 µm laser fibers were used. Stone size, stone density, laser-on time (LOT) and laser settings were recorded. We also assessed the ablation speed (mm3/s), Joules/mm3 and laser power (W) values for each procedure. Postoperative results, such as stone-free rate (SFR) and zero fragments rate (ZFR) were also recorded.
Results
A total of 25 patients were analyzed (Table 1). The median (IQR) age was 55 (44–72) years old. Median (IQR) stone volume was 2849 (916–9153)mm3. Median (IQR) stone density was 1000 (600–1174)HU. Median (IQR) pulse energy, pulse rate and total power were 0.6 (0.6–0,8)J, 15(15–20)Hz and 12(9–16)W, respectively. All procedures used “Captive Fragmenting” pulse modulation (Table 2). The median (IQR) J/mm3 was 14,8 (6–21). The median (IQR) ablation rate was 0,75 (0,46–2)mm3/s. One postoperative complications occurred (streinstrasse). SFR and ZFR were 95% and 55%, respectively.
Conclusion
The pulsed-Tm:YAG laser is a safe and effective laser source for lithotripsy during RIRS, using low pulse energy and low pulse frequency.

Similar content being viewed by others

References
Traxer O, Keller EX (2019) Thulium fiber laser: the new player for kidney stone treatment? A comparison with Holmium:YAG laser. World J Urol. 38:1883
Johnson DE, Cromeens DM, Price RE (1992) Use of the holmium:YAG laser in urology. Lasers Surg Med 12(4):353–363
Gupta PK (2007) Is the holmium:YAG laser the best intracorporeal lithotripter for the ureter? A 3-year retrospective study. J Endourol Mars 21(3):305–309
Urofrance | Recommandations de bonne pratique pour la prise en charge des calculs et de la lithiase urinaires: diagnostic, traitement, suivi et prévention secondaire - Argumentaire - Urofrance [Internet]. [cité 17 nov 2022]. Disponible sur: https://www.urofrance.org/recommandation/recommandations-de-bonne-pratique-pour-la-prise-en-charge-des-calculs-et-de-la-lithiase-urinaires-diagnostic-traitement-suivi-et-prevention-secondaire-argumentaire/
Blackmon RL, Irby PB, Fried NM (2011) Comparison of holmium:YAG and thulium fiber laser lithotripsy: ablation thresholds, ablation rates, and retropulsion effects. J Biomed Opt juill 16(7):071403
Ventimiglia E, Doizi S, Kovalenko A, Andreeva V, Traxer O (2020) Effect of temporal pulse shape on urinary stone phantom retropulsion rate and ablation efficiency using holmium:YAG and super pulse thulium fiber lasers. BJU Int. 126:159
Petzold R, Miernik A, Suarez-Ibarrola R (2021) In vitro dusting performance of a new solid state thulium laser compared to holmium laser lithotripsy. J Endourol févr 35(2):221–225
Petzold R, Miernik A, Suarez-Ibarrola R (2021) Retropulsion force in laser lithotripsy-an in vitro study comparing a Holmium device to a novel pulsed solid-state thulium laser. World J Urol. 39:3651
Petzold R, Suarez-Ibarrola R, Miernik A (2021) Temperature assessment of a novel pulsed thulium solid-state laser compared with a holmium:yttrium-aluminum-garnet laser. J Endourol juin 35(6):853–859
Kraft L, Yilmaz M, Petzold R, Gratzke C, Suarez-Ibarrola R, Miernik A (2022) Dusting efficiency of a novel pulsed thulium: yttrium aluminum garnet laser vs a thulium fiber laser. J Endourol févr 36(2):259–265
Kraft L, Petzold R, Suarez-Ibarrola R, Miernik A (2022) In vitro fragmentation performance of a novel, pulsed Thulium solid-state laser compared to a Thulium fibre laser and standard Ho:YAG laser. Lasers Med Sci avr 37(3):2071–2078
Brisbane W, Bailey MR, Sorensen MD (2016) An overview of kidney stone imaging techniques. Nat Rev Urol 13(11):654–662
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S et al (2012) 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging 30(9):1323–1341
Panthier F, Traxer O, Yonneau L, Lebret T, Berthe L, Illoul L et al (2021) Evaluation of a free 3D software for kidney stones’ surgical planning: kidney stone calculator a pilot study. World J Urol. 39:3607
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg août 240(2):205–213
Thulio® [Internet]. Dornier MedTech. [cité 19 mai 2023]. Disponible sur: https://www.dornier.com/products-item/dornier-thulio/
Sierra A, Corrales M, Piñero A, Traxer O (2022) Thulium fiber laser pre-settings during ureterorenoscopy: Twitter’s experts’ recommendations. World J Urol. 40:1529
Sierra A, Corrales M, Piñero A, Kolvatzis M, Somani B, Traxer O (2022) Glossary of pre-settings given by laser companies: no consensus! World J Urol 40(9):2313–2321
Weiss B, Shah O (2016) Evaluation of dusting versus basketing—can new technologies improve stone-free rates? Nat Rev Urol 13(12):726–733
Keller EX, De Coninck V, Doizi S, Daudon M, Traxer O (2020) What is the exact definition of stone dust? An in vitro evaluation. World J Urol. 39:187
Ventimiglia E, Pauchard F, Gorgen ARH, Panthier F, Doizi S, Traxer O (2020) How do we assess the efficacy of Ho:YAG low-power laser lithotripsy for the treatment of upper tract urinary stones? Introducing the Joules/mm3 and laser activity concepts. World J Urol. 39:891
Petzold R, Suarez-Ibarrola R, Miernik A (2021) Gas bubble anatomy during laser lithotripsy: an experimental in vitro study of a pulsed solid-state tm:yag and ho:yag device. J Endourol juill 35(7):1051–1057
Panthier F, Doizi S, Gorny C, Berthe L, Traxer O (2020) Impact of laser fiber diameter and irrigation fluids on induced bubble stream dynamics with superpulsed thulium fiber laser : an in vitro study. J Endourol. 35:1883
Hardy LA, Kennedy JD, Wilson CR, Irby PB, Fried NM (2017) Analysis of thulium fiber laser induced bubble dynamics for ablation of kidney stones. J Biophotonics 10(10):1240–1249
Ulvik Ø, Æsøy MS, Juliebø-Jones P, Gjengstø P, Beisland C. Thulium Fibre Laser versus Holmium:YAG for Ureteroscopic Lithotripsy: Outcomes from a Prospective Randomised Clinical Trial. Eur Urol [Internet]. 14 mars 2022 [cité 16 mars 2022];0(0). Disponible sur: https://www.europeanurology.com/article/S0302-2838(22)01669-4/fulltext
Panthier F, Doizi S, Lapouge P, Chaussain C, Kogane N, Berthe L et al (2020) Comparison of the ablation rates, fissures and fragments produced with 150 µm and 272 µm laser fibers with superpulsed thulium fiber laser: an in vitro study. World J Urol. 39:1683
Sierra A, Corrales M, Kolvatzis M, Traxer O (2022) Initial clinical experience with the thulium fiber laser from Quanta System: First 50 reported cases. World J Urol 40(10):2549–2553
Corrales M, Traxer O (2021) Initial clinical experience with the new thulium fiber laser: first 50 cases. World J Urol. 39:3945
Professionals SO. EAU Guidelines: Urolithiasis [Internet]. Uroweb. [cité 21 sept 2020]. Disponible sur: https://uroweb.org/guideline/urolithiasis/
Louters MM, Dau JJ, Hall TL, Ghani KR, Roberts WW (2022) Laser operator duty cycle effect on temperature and thermal dose: in-vitro study. World J Urol 40(6):1575–1580
Funding
No funding to declare for this study.
Author information
Authors and Affiliations
Contributions
FP: protocol development, data collection and management, data analysis, manuscript writing and editing. CS: data collection and management. SD: protocol development, manuscript writing and editing. SK: data collection and management. MC: manuscript writing and editing. LC: manuscript writing and editing. MC: manuscript writing and editing. OT: protocol development, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest but: Olivier Traxer has declared as consultant for Karl Storz, Coloplast, IPG photonics, Ambu, Quanta System and Rocamed. Steeve Doizi has declared as consultant for Boston Scientific Corporation and Coloplast.
Research involving human participants or animals
Approval was obtained from the ethics committee of the French Association of Urology. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Verbal and written informed consent were obtained prior to the surgery.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the supplementary videoclip.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 3042 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Panthier, F., Solano, C., Chicaud, M. et al. Initial clinical experience with the pulsed solid-state thulium YAG laser from Dornier during RIRS: first 25 cases. World J Urol 41, 2119–2125 (2023). https://doi.org/10.1007/s00345-023-04501-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04501-0