Abstract
Background
Perioperative antibiotic prophylaxis (PAP) is an integral part of kidney transplantation to prevent surgical site infections (SSI). In July 2015, we changed our standard from a multiple-dose to a single-dose (SD) prophylaxis. Here, we report on results with both regimens and a related survey among Eurotransplant renal transplantation centers.
Methods
From July 2015, all kidney graft recipients of our center were scheduled to receive SD i.v. cefazolin (group SD, n = 107). They were compared to patients, transplanted since January 2014, receiving our previous standard (i.v. piperacillin/flucloxacillin) until postoperative day (POD) 7, plus oral sultamicillin until POD 10 (group MD, n = 105). The primary endpoint was the number of SSIs during a 3-month observational period.
Results
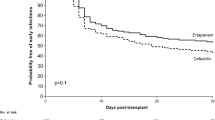
The frequency of SSI episodes was generally low (group SD vs. MD: 2 vs. 4, p = 0.40). Of note, urinary tract infections occurred in 40 SD vs. 36 MD patients, respectively (p = 0.60). Urinary tract infections were caused by Escherichia coli in 36.8%. Female gender was the only independent risk factor on multivariate analysis (p = 0.002). In addition, 12 episodes of urosepsis in both groups occurred. All-cause infection with multi-resistant bacteria occurred less frequently in SD vs. MD patients (3.7% vs. 8.6%, p = 0.16). A majority of Eurotransplant centers used i.v. single-dose cephalosporins (36.9%), although substances and duration varied remarkably.
Conclusion
Single-dose cefazolin was equally effective and less expensive compared to our previous MD regimen. Based on these findings, we conclude that future prospective studies should be designed to confirm the non-inferiority of single-dose antibiotic regimens.


Similar content being viewed by others
Abbreviations
- ABMR:
-
Antibody-mediated rejection
- AB0i:
-
AB0-incompatible
- DGF:
-
Delayed graft function
- EAU:
-
European Association of Urology
- ITT:
-
Intention-to-treat
- MDR:
-
Multidrug-resistant
- MRGN:
-
Multidrug-resistant Gram-negative
- NODAT:
-
New onset diabetes after transplantation
- PAP:
-
Perioperative antibiotic prophylaxis
- POD:
-
Postoperative day
- PP:
-
Per-protocol
- SSI:
-
Surgical site infection
- UTI:
-
Urinary tract infection
References
Cohen J, Rees AJ, Williams G (1988) A prospective randomized controlled trial of perioperative antibiotic prophylaxis in renal transplantation. J Hosp Infect 11(4):357–363
Kasiske BL, Zeier MG, Chapman JR et al (2010) KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int 77(4):299–311
Chadban SJ, Barraclough KA, Campbell SB et al (2012) KHA-CARI guideline: KHA-CARI adaptation of the KDIGO clinical practice guideline for the care of kidney transplant recipients. Nephrol (Carlton) 17(3):204–214
Bratzler DW, Dellinger EP, Olsen KM et al (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt) 14(1):73–156
Baker RJ, Mark PB, Patel RK, Stevens KK, Palmer N (2017) Renal association clinical practice guideline in post-operative care in the kidney transplant recipient. BMC Nephrol 18(1):174
Wacha H, Hoyme U, Isenmann R et al (2010) Perioperative antibiotika-prophylaxe. Chemother J 19(3):70–84
Hevia V (2018) EAU Guidelines. Edn. presented at the EAU Annual Congress Copenhagen 2018. EAU Guidelines Office, Arnhem, The Netherlands
Laftavi MR, Rostami R, Patel S et al (2012) Universal perioperative antimicrobial prophylaxis is not necessary in kidney transplantation. Clin Transpl 26(3):437–442
Haas M, Sis B, Racusen LC, Solez K et al (2014) Banff 2013 meeting report: inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am J Transpl 14(2):272–283
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Levy MM, Fink MP, Marshall JC, Abraham E et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31(4):1250–1256
Wendt C (2012) Hygienemaßnahmen bei Infektionen oder Besiedelung mit multiresistenten gramnegativen Stäbchen. Empfehlung der Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) beim Robert Koch-Institut (RKI). Bundesgesundheitsblatt 55:1311–1354 (Springer)
Fritsche L, Schroter K, Lindemann G, Kunz R, Budde K, Neumayer HH (2000) A web-based electronic patient record system as a means for collection of clinical data. Lect Notes Comput Sci 1933:198–205
El-Bandar N, Kroy DC, Fuller TF et al (2017) Development of graft-site candidiasis in 3 solid organ transplant recipients from the same donor. Am J Case Rep. 18:777–781
Midtvedt K, Hartmann A, Midtvedt T, Brekke IB (1998) Routine perioperative antibiotic prophylaxis in renal transplantation. Nephrol Dial Transpl 13(7):1637–1641
Pfundstein J, Roghmann MC, Schwalbe RS et al (1999) A randomized trial of surgical antimicrobial prophylaxis with and without vancomycin in organ transplant patients. Clin Transpl 13(3):245–252
Wszola M, Kwiatkowski A, Ostazewska A et al (2013) Surgical site infections after kidney transplantation—where do we stand now? Transplantation 95:878–882
Orlando G, Manzia TM, Sorge R et al (2015) One-shot versus multidose perioperative antibiotic prophylaxis after kidney transplantation: a randomized, controlled clinical trial. Surgery 157(1):104–110
Battaglia M, Ditonno P, Fiore T, De Ceglie G, Regina G, Selvaggi FP (2000) True mycotic arteritis by Candida albicans in 2 kidney transplant recipients from the same donor. J Urol 163(4):1236–1237
Mai H, Champion L, Ouali N et al (2006) Candida albicans arteritis transmitted by conservative liquid after renal transplantation: a report of four cases and review of the literature. Transplantation 82(9):1163–1167
Albano L, Bretagne S, Mamzer-Bruneel MF et al (2009) Evidence that graft-site candidiasis after kidney transplantation is acquired during organ recovery: a multicenter study in France. Clin Infect Dis 48(2):194–202
Guy A, Chinai N, Ashley S, Rowe P, Cunningham R, Barwell J (2013) Candida arteritis in a pair of renal transplant recipients. Exp Clin Transplant 11(6):558–561
Canaud G, Zuber J, Sberro R et al (2009) Intensive and prolonged treatment of focal and segmental glomerulosclerosis recurrence in adult kidney transplant recipients: a pilot study. Am J Transpl 9(5):1081–1086
Garrouste C, Canaud G, Buchler M et al (2017) Rituximab for recurrence of primary focal segmental glomerulosclerosis after kidney transplantation: clinical outcomes. Transplantation 101(3):649–656
Waiser J, Budde K, Schutz M et al (2012) Comparison between bortezomib and rituximab in the treatment of antibody-mediated renal allograft rejection. Nephrol Dial Transpl 27(3):1246–1251
Anesi JA, Blumberg EA, Abbo LM (2018) Perioperative antibiotic prophylaxis to prevent surgical site infections in solid organ transplantation. Transplantation 102:21–34
Acknowledgements
We are grateful to our colleagues from all Eurotransplant centers, who participated in our survey.
Funding
The authors received no funding for this work.
Author information
Authors and Affiliations
Contributions
Friederike Bachmann and Johannes Waiser: conception, data acquisition, data analysis, preparation and writing of the manuscript. Thomas Adam: conception, data analysis, and critical revision of the manuscript. Frank Friedersdorff: transplant surgery, and critical revision of the manuscript. Lutz Liefeldt, and Torsten Slowinski: critical revision of the manuscript. Klemens Budde: conception, critical revision and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bachmann, F., Adam, T., Friedersdorff, F. et al. Perioperative antibiotic prophylaxis in renal transplantation: a single-center comparison between two regimens and a brief survey among the Eurotransplant renal transplantation centers. World J Urol 37, 957–967 (2019). https://doi.org/10.1007/s00345-018-2440-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2440-2